Health Disparities and Cultural Competence
33 Slides2.39 MB

Health Disparities and Cultural Competence
Health Disparities and Cultural Competence G.W. is a 62 year old male who came to the United States 12 years ago from Mexico with his son and three daughters. His eldest daughter is the primary care giver. He owns his own brick laying company. He works full-time and is often out on job sites working during the day.
Health Disparities and Cultural Competence G.W. is regularly seen at the Apple Health Clinic for a variety of health concerns. He has chronic hypertension and chronic back pain related to a fall he experienced ten years ago. Today he is accompanied by his daughter, daughterin-law and four grandchildren. He has been prescribed a DASH diet and takes Lisinopril 10 mg once daily by mouth for his high blood pressure. He says he takes ibuprofen occasionally for back pain. English is the second language for the adult family members. G.W.’s granddaughter Eleiyah is 12 years old and frequently translates for the family.
Health Disparities and Cultural Competenc e Through his granddaughter’s translation, G.W. reports he is in the clinic today because his eye hurts. It is red and has yellow drainage. He says he has been working a lot, it’s very hot outside. He is very tired and always thirsty. He notices that his pants seem to be getting too big.
The nurse completes her assessment. G.W.’s blood pressure is 132/90. Health Disparities and Cultural Competence Given the language barrier and the chaos with all of the family with G.W. the nurse does not ask G.W. further about his fatigue. She does not ask for a diet record for the past 24 hours nor review management of high blood pressure with the family. The physician diagnosis G.W. with bacterial conjunctivitis (pink eye). G.W. is prescribed Gentamicin sulfate antibiotic eye drops. Two drops to left eye twice daily for ten days. The nurse hands the prescription to the granddaughter and asks her to tell her grandfather to put two drops in his left eye twice daily. The nurses asks if he understands. G.W. nods his head and the family leaves the clinic. The nurse smiles and tell them good-bye.
What type of health disparity has G.W. experienced? Health Disparities and Cultural Competence
What type of health disparity has G.W. experienced? Ethnicity Health Disparities and Cultural Competence
What type of health disparity has G.W. experienced? Ethnicity Health Disparities and Cultural Competence What factors contributed to G.W. not receiving the standard of care?
What type of health disparity has G.W. experienced? Ethnicity Health Disparities and Cultural Competence What factors contributed to G.W. not receiving the appropriate standard of care? Language barrier. Attitude of the nurse. Age of the translator.
What type of health disparity has G.W. experienced? Ethnicity Health Disparities and Cultural Competence What factors contributed to G.W. not receiving the standard of care? Language barrier. Attitude of the nurse. Age of the translator. What additional assessments should have been completed at this visit?
What type of health disparity has G.W. experienced? Ethnicity Health Disparities and Cultural Competence What factors contributed to G.W. not receiving the standard of care? Language barrier. Attitude of the nurse. Age of the translator. What additional assessments should have been completed at this visit? Complete health history. Further questions about complaints of fatigue. Medication reconciliation. 24 Hour diet recall.
What type of health disparity has G.W. experienced? Ethnicity Health Disparities and Cultural Competence What factors contributed to G.W. not receiving the standard of care? Language barrier. Attitude of the nurse. Age of the translator. What additional assessments should have been completed at this visit? Complete health history. Further questions about complaints of fatigue. Medication reconciliation. 24 Hour diet recall. What additional education could have been completed at this time?
What type of health disparity has G.W. experienced? Ethnicity Health Disparities and Cultural Competence What factors contributed to G.W. not receiving the standard of care? Language barrier. Attitude of the nurse. Age of the translator. What additional assessments should have been completed at this visit? Complete health history. Further questions about complaints of fatigue. Medication reconciliation. 24 Hour diet recall. What additional education could have been completed at this time? Dash diet. Proper administration of eye drops.
G.W. returns to the clinic one week later. He is accompanied by his daughter and four grandchildren. Health Disparities and Cultural Competence He continues to feel tired and his eye is red with yellow drainage. You are the nurse this weekend. You assess G.W. and take his VS. They are within normal limits. You also note that he has lost more than 15 pounds over the past six month. You recognize the adult members of the family do not speak English.

How do you choose a translator?
Use an agency interpreter if possible who is trained medical interpreter. Only use a family member if absolutely necessary. How do you choose a translator?

What are the key characteristics for an interpreter to possess?
What are the key characteristics for an interpreter to possess? Interpreters should be able to interpret: Verbal and non-verbal cues. Translate medical terms into understandable terms. Act as a patient advocate. Understand how to provide teaching instructions.

What are the disadvantag es of using a family member as an interpreter?
What are the disadvantag es of using a family member as an interpreter? What are the disadvantages of using a family member as an interpreter? May not understand medical terms. Patient may not be comfortable sharing information in front of family. Family interpreters may not be aware of health care procedures or medical ethics.
You call the translation hotline the clinic uses for translation services. Health Disparities and Cultural Competence You complete your history of G.W. using the translation services. G.W. always feels thirsty. You review his 24 hour food history. He is not following the dash diet. He reports his appetite has not decreased. He keeps eating but noticed his clothes are too big for him. He wasn’t sure how to take the eye drops. He was putting two drops in both eyes twice daily. He quit using the eye drop three days because his eye wasn’t red anymore. You share the history of weight loss and symptoms with the clinic physician. He is concerned G.W. may have Type 2 Diabetes Mellitus. You take his FSBS. It is 290 mg/dL. Upon reviewing G.W. history you also note that he has never received education about the DASH diet. You prepare to educate G.W.

What strategies can you use to work with an interpreter?
What strategies can you use to work with an interpreter? Speak slowly. Maintain eye contact with the patient. Talk to the patient not the interpreter. Use simple language, using as few medical terms as possible. Speak in one or two sentences at a time for easier translation. Avoid raising your voice during the interaction. Ask for feedback from the patient to verify the patient understands (teach-back method) . Plan on the visit taking twice as long. Document usage of translator in the medical record.

Understandabl e Explanations
How would you explain Finger Stick Blood Sugar to G.W Understandabl e Explanations
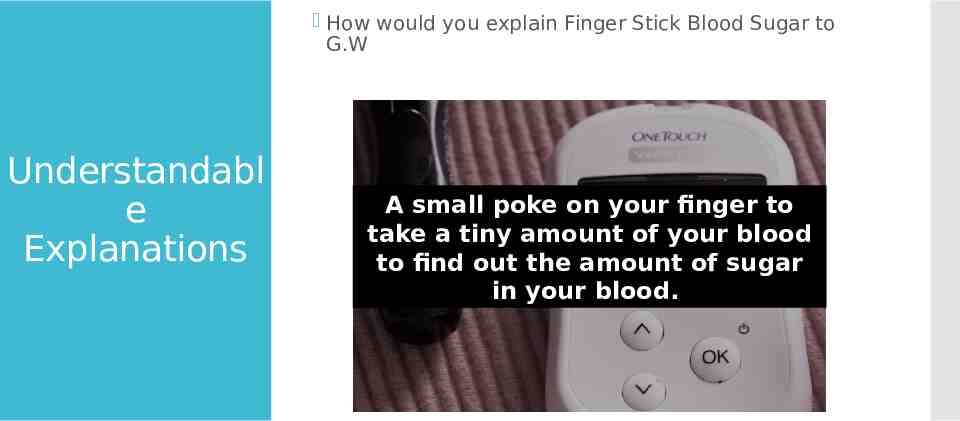
How would you explain Finger Stick Blood Sugar to G.W Understandabl e Explanations A small poke on your finger to take a tiny amount of your blood to find out the amount of sugar in your blood.
You have collected appropriate lab to confirm the possible diagnosis of Type II Diabetes. Health Disparities and Cultural Competenc e The physician has prescribed Glyburide. You explain how to used the medication. Utilizing the translator, you allow G.W. to repeat the instructions back to you. You have assisted in scheduling an appointment for G.W. to meet with a diabetic educator and a dietician the following week. G.W. is scheduled to come back next week
In healthcare, you will encounter situations that require you to communicate important information to other members of the healthcare team. Communicati ng With Peers How would you recommend following up with the first nurse?
In healthcare, you will encounter situations that require you to communicate important information to other members of the healthcare team. Communicati ng With Peers How would you recommend following up with the first nurse? C-I am concerned. U-I am uncomfortable. S-This is a safety issue. https://www.ahrq.gov/professionals/quality-patient-s afety/hais/tools/ambulatory-surgery/sections/implem entation/training-tools/cus-tool.html Practice with a classmate.
How would you recommend following up with the first nurse? Communicati ng With Peers Practice with a classmate. C-I am concerned about G.W. U-I am uncomfortable with the care G.W. received in our clinic. S-This is a safety issue. G.W. did not understand the D.A.S.H. diet and he didn’t understand how to take his eye drops. He was experiencing new symptoms had experienced significant weight loss. We did not offer a translator and we did not provide the proper care for him.
What additional actions are appropriate? Communicati ng With Peers
What additional actions are appropriate? Communicati ng With Peers It is important to report errors and “near misses” to your charge nurse, supervisor or manager. Report the facts without assessing blame. Through the reporting of errors or “near misses” process improvement and education can be implemented. Failure to address safety concerns leads to error and prevents healthcare professionals from improving their practice.
THE END