Head and spinal cord injuries Department of Neurology LF UPJŠ
68 Slides5.11 MB
Head and spinal cord injuries Department of Neurology LF UPJŠ Košice 6.12.2017
Brain/head injury Brain and spinal cord injuries and post-traumatic conditions is a serious medical and socio-economic problem (permanent consequences, disability, financial costs, .) Most often in traffic accidents, sports and occupational accidents Craniocerebral injury is damage to the skull, brain, or both, an injury mechanism Splitt into : - open and closed - focal and diffuse
Brain/head injury - mechanism of action Translating - head collision with second body Acceleration - linear or rotary The patient may also fall as a result of the disease condition: – – – – Syncope Epileptic seizure Intoxication Stroke
Head injuries: classification Primary – occur at the time of the accident - Diffuse: Brain concussion, Brain contusion, Diffuse axonal injury-DAI - Focal/multifocal: Brain contusion Secondary – occur later (the result of an accident) A) intracranial - complications of primary injury (epidural bleeding, subdural bleeding, intracerebral and traumatic subarachnoid haemorrhage) B) extracranial - brain damage eg. hypotension, hypovolemia, etc. Interdisciplinary approach: traumatologist, anesthetist, neurologist and neurosurgeon, physiotherapist, orthopedic .
Introduction: Craniocerebral Injuries Effect of an external force on the skull and the brain tissue with permanent or transient impairment of brain functions 1. CLOSED 2. OPEN – Impairment of the dura mater integrity
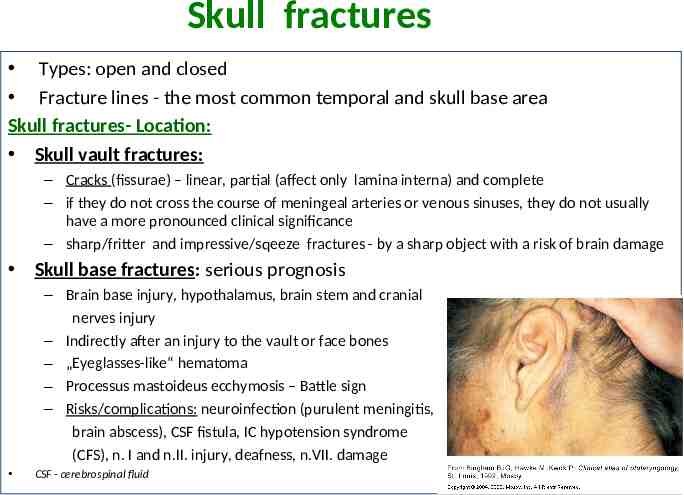
Skull fractures Types: open and closed Fracture lines - the most common temporal and skull base area Skull fractures- Location: Skull vault fractures: – Cracks (fissurae) – linear, partial (affect only lamina interna) and complete – if they do not cross the course of meningeal arteries or venous sinuses, they do not usually have a more pronounced clinical significance – sharp/fritter and impressive/sqeeze fractures - by a sharp object with a risk of brain damage Skull base fractures: serious prognosis – Brain base injury, hypothalamus, brain stem and cranial nerves injury – Indirectly after an injury to the vault or face bones – „Eyeglasses-like“ hematoma – Processus mastoideus ecchymosis – Battle sign – Risks/complications: neuroinfection (purulent meningitis, brain abscess), CSF fistula, IC hypotension syndrome (CFS), n. I and n.II. injury, deafness, n.VII. damage CSF - cerebrospinal fluid
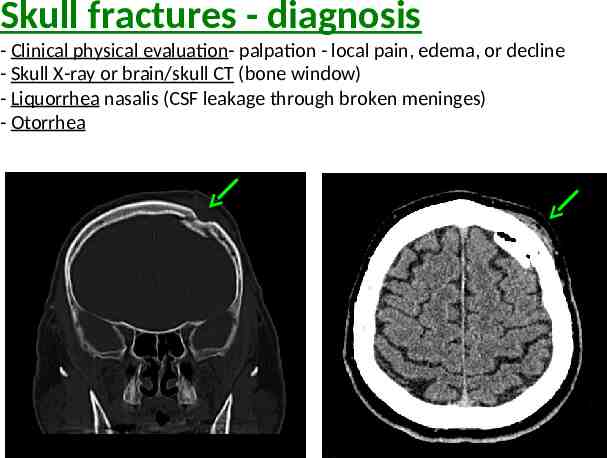
Skull fractures - diagnosis - Clinical physical evaluation- palpation - local pain, edema, or decline - Skull X-ray or brain/skull CT (bone window) - Liquorrhea nasalis (CSF leakage through broken meninges) - Otorrhea
Skull fractures- therapy Linear skull fractures (fissurae calvae) Mostly without clinical symptoms and requiring no surgical treatment Observation to exclude the development of extracerebral hematoma Impressive skull fractures with significant bone dislocation surgical repositioning of debris under great impression - rupture of the dura and brain contusion on the brain surface with expansive character in the frontal area - even less impression is elevated in a case when cosmetically significant defect is posed to the patient for skull base fractures - ATB coverage is recommended, risk of pathogens /bacterias entry from oropharynx and airways
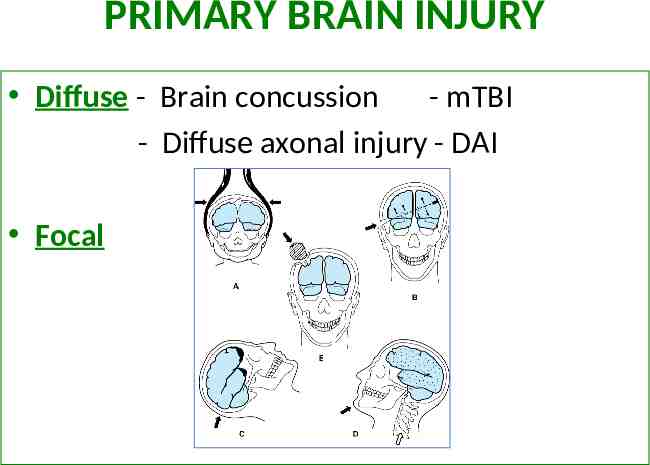
PRIMARY BRAIN INJURY Diffuse - Brain concussion - mTBI - Diffuse axonal injury - DAI Focal
1. BRAIN CONCUSSION (COMMOTIO CEREBRI, MILD TRAUMATIC BRAIN INJURY- MTBI) 2 definitions: 1. Reversibile,global brain function failure (transient lost of synaptic function) - generalised asynapsia, reticular formation dysfunction - disturbance of consciousness (revised definition from 2008) 2. Brain injury caused by external mechanical energy on the head area associated with a subsequent CNS disorder Appearance: 70 – 90 % of all cranio-cerebral injuries men are twice as likely to be affected the most at risk is the age group 15 – 24 years Reasons: traffic accidents and falls in which the brains are shuffled back and forth
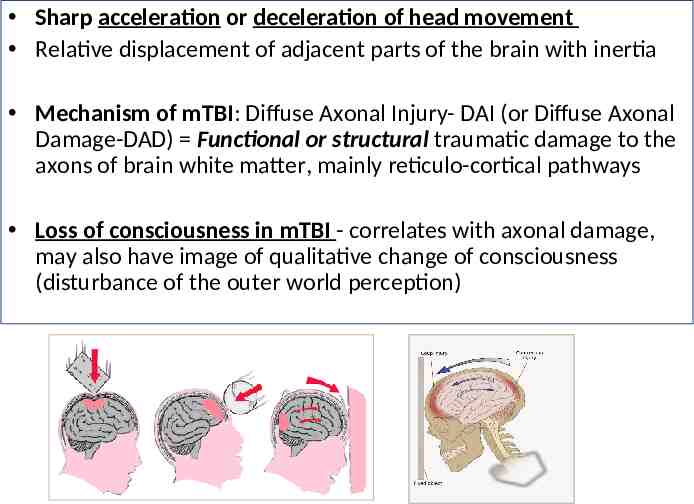
Sharp acceleration or deceleration of head movement Relative displacement of adjacent parts of the brain with inertia Mechanism of mTBI: Diffuse Axonal Injury- DAI (or Diffuse Axonal Damage-DAD) Functional or structural traumatic damage to the axons of brain white matter, mainly reticulo-cortical pathways Loss of consciousness in mTBI - correlates with axonal damage, may also have image of qualitative change of consciousness (disturbance of the outer world perception)
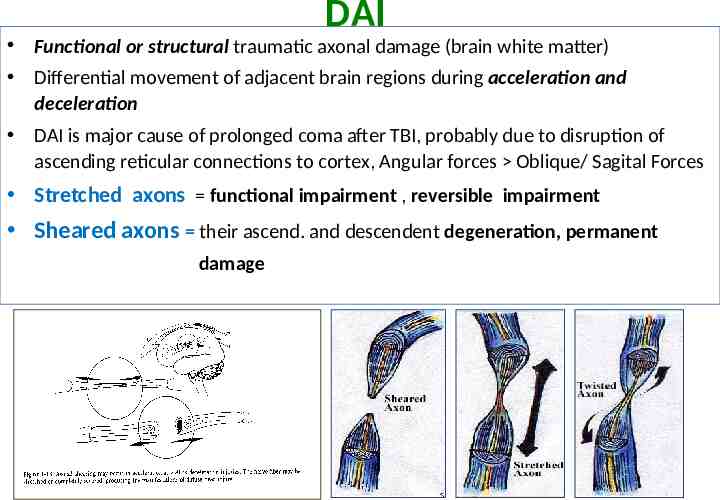
DAI Functional or structural traumatic axonal damage (brain white matter) Differential movement of adjacent brain regions during acceleration and deceleration DAI is major cause of prolonged coma after TBI, probably due to disruption of ascending reticular connections to cortex, Angular forces Oblique/ Sagital Forces Stretched axons functional impairment , reversible impairment Sheared axons their ascend. and descendent degeneration, permanent damage
MTBI - MILD TRAUMATIC BRAIN INJURY always comes suddenly duration of symptoms - different (a few seconds to hours) Injury mechanism: – either by moving the head that is stopped by the motionless object or the impact of the moving object on the head – direct attack on the head, face, neck, or any part of the body with inertial force transfer to the brain region Unconsciousness and retrograde amnesia without the presence and evident structural brain lesion, which will take off without consequences
MTBI : clinical picture Neurological evaluation score of GCS (Glasgow Coma Scale) mTBI: GCS 13 – 15 and duration of unconsciousness (if present) within 30 minutes Clinical picture must meet at least one of the following criteria : confusion and / or disorientation Unconsciousness of up to 30 minutes (may or may not be) - DAI Post-traumatic amnesia up to 24 hours (the lost memory of the event) Other transient neurological symptomatology – focal neurological deficit, convulsion and detected intracranial lesion, not required neurosurgical intervention
MTBI: clinical picture Areflexia, bradycardia and hypotension, nauzea Gradually, the patient takes over, is disoriented, can not make simple commands, confused, behavior changes, slow reactions, incoherent speech, motion coordination disorder, restlessness, crying (disappear within minutes) Post-traumatic stunning (obnubilation) state: restlessness, aggression, uncritical status more often alcoholics and people with brain damage already before the accident amnesia covers the entire time of the obnubilation Post- mTBI convulsions: specific non-epileptic phenomenon occurs within 2 seconds of the crash short-term tonic stiffness and subsequent two-sided, often asymmetrical myoclonic jerks up to 3 minutes (similar to convulsive syncope)
POST-CONCUSSION SYNDROME Occurs when trying to start a normal personal and working life after head injury Symptoms retreat within a few days or weeks Improvement after mTBI – within 3 to 12 months 5 % - 1 or more symptoms are persistent even one year after the injury (headache, dizziness, fatigue, attention deficit, memory and selected executive functions problems) Somatic and vegetative: headache, dizziness, nausea, vomiting, smell deficit, insomnia, rapid tiredness, pathological fatigue, visual problems, hypersensitivity to light and noise Cognitive: disturbance of attention, memory, slowing of thinking, faults in executive functions, decreased performance Emotional : emotional lability, depression, anxiety, nervousness, apathy
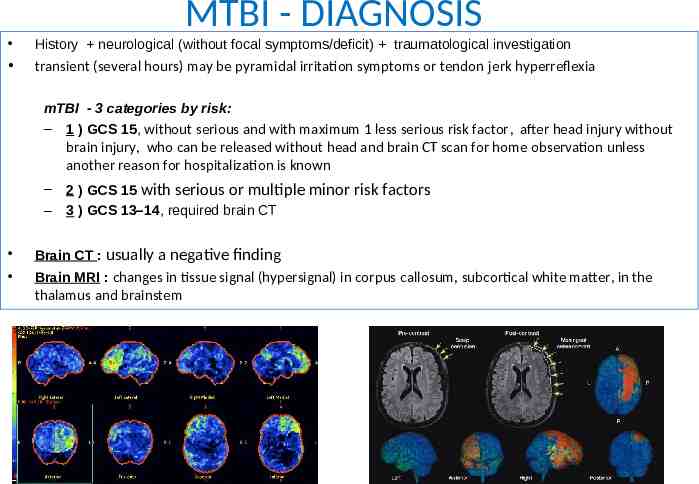
MTBI - DIAGNOSIS History neurological (without focal symptoms/deficit) traumatological investigation transient (several hours) may be pyramidal irritation symptoms or tendon jerk hyperreflexia mTBI - 3 categories by risk: – 1 ) GCS 15, without serious and with maximum 1 less serious risk factor, after head injury without brain injury, who can be released without head and brain CT scan for home observation unless another reason for hospitalization is known – – 2 ) GCS 15 with serious or multiple minor risk factors 3 ) GCS 13–14, required brain CT Brain CT : usually a negative finding Brain MRI : changes in tissue signal (hypersignal) in corpus callosum, subcortical white matter, in the thalamus and brainstem
MTBI – DIFFERENTIAL DIAGNOSIS Other states of short-term loss of consciousness: Epileptic seizure Syncope Arhytmia Intoxication Diabetic coma Patient with an uncertain history, is approaching laboratory examination of biochemical parameters in order to exclude metabolic disorders, cardiac disorders /ECG/, etc.
MTBI – THERAPY 1) In the case of negative brain CT, and negative neurological findings and amnesia up to maximally 60 minutes - patient may be released 2) Observation – – – – – – – – – Focal neurological deficit GCS 15 points prolonged posttraumatic amnesia/ agitation Headache of high intensity Persisting vomitus Liquorrhea with suspected skull base fracture Polytrauma Koagulaopathy Alcohol or drug intoxication Suspected non- traumatic damage Mode: repeatedly evaluated neurological status – GCS 15. every 30 minutes – GCS 15. every 30 minutes for the first 2 hours and if there is no deterioration every 1 hour for the next 4 hours and then once every 2 hours – Patient observation should be at least 12-24 hours
MTBI – THERAPY Acute state: physical and mental relax until symptoms disappear, followed by gradual loading analgetics (inappropriate non-steroidal anti-inflammatory drugs, ASA-risk of bleeding higher opiates - effect on consciousness) Prognosis : generally favorable spontaneous disappearance of post-mTBI symptoms Profylaxy: use of helmets (bicycles, motorbikes), education of adults and children about the brain injury risks and consequences adjustment of risk working practices in individual jobs
POST-CONCUSSION SYNDROME (POST-MTBI SYNDROME) Definition a set of multiple defined persistent post-concussion symptoms Occurrence: 50 % of cases of mTBI either immediately after the concussion or with latency of a few days after the accident Substrate: unknown Headache, attention disturbance, sleep disordres, fatigue, inefficiencies, dizziness, vegetative dysfunction, 2-12 months, EEG – slight patologic pattern 5 – 20 % - lasts up to one year Chronic traumatic encephalopathy Repeated head injuries ! (boxers, epileptic falls, physically abused persons) can trigger a neurodegenerative cascade - progressive tau-pathies
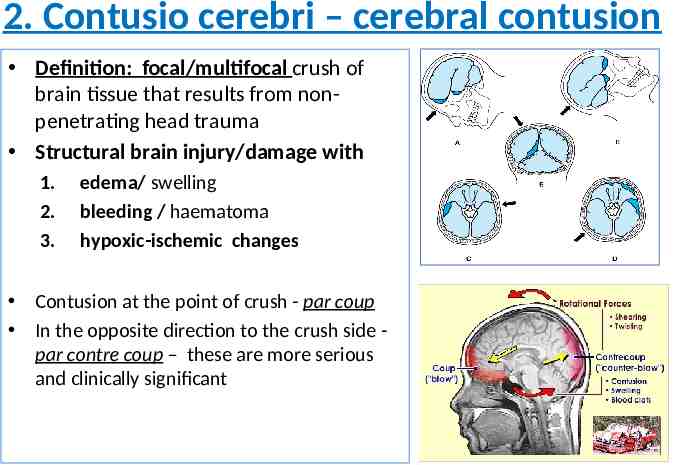
2. Contusio cerebri – cerebral contusion Definition: focal/multifocal crush of brain tissue that results from nonpenetrating head trauma Structural brain injury/damage with 1. 2. 3. edema/ swelling bleeding / haematoma hypoxic-ischemic changes Contusion at the point of crush - par coup In the opposite direction to the crush side par contre coup – these are more serious and clinically significant
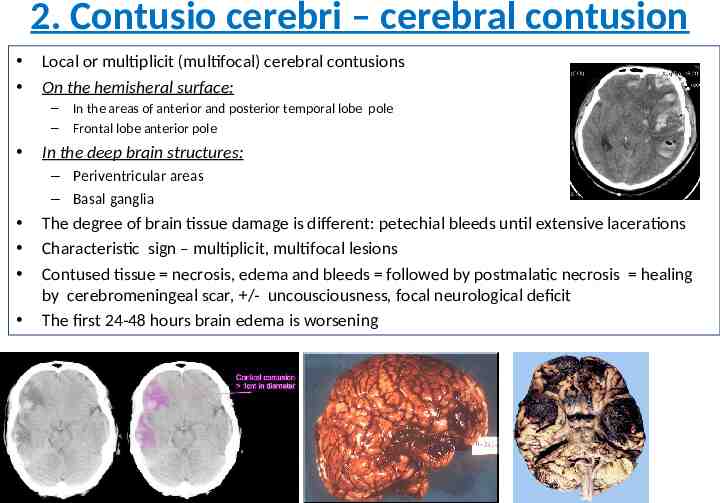
2. Contusio cerebri – cerebral contusion Local or multiplicit (multifocal) cerebral contusions On the hemisheral surface: – – In the areas of anterior and posterior temporal lobe pole Frontal lobe anterior pole In the deep brain structures: – Periventricular areas – Basal ganglia The degree of brain tissue damage is different: petechial bleeds until extensive lacerations Characteristic sign – multiplicit, multifocal lesions Contused tissue necrosis, edema and bleeds followed by postmalatic necrosis healing by cerebromeningeal scar, /- uncousciousness, focal neurological deficit The first 24-48 hours brain edema is worsening
2. Cerebral contusion Clinical symptoms and disease course: depends on the extent and location of lesions totally asymptomatic . up to heavy contusions with unconsciousness Clinically manifested brain contusion: always present disorder of consciousness (qualitative and quantitative) and focal neurological deficit (e.g. hemiparesis, aphasia, agnosia, epileptic seizures) qualitative consciousness changes – prefrontal syndrome behavioral disturbance, affectivity change, restless, loss of orientation in space, lack of criticism and deliberation sleepiness can be alternated with restlessness, agitation and confusion state
2. Cerebral contusion In the beginning, unconsciousness may be present - usually longer! as in brain concussion (mTBI) (hours to days) an amnesia for head injury is always present A) a temporal - lucide interval (short wakefulness) may occur and the development of the focal symptoms due to perifocal edema continues again a disturbance of consciousness arise B) in many cases the lucide interval is missing the patient is unconscious from the beginning GCS 7 serious state, poor prognosis GCS 9 better prognosis (the border is GCS 8 points) GCS- Glasgow Coma Scale
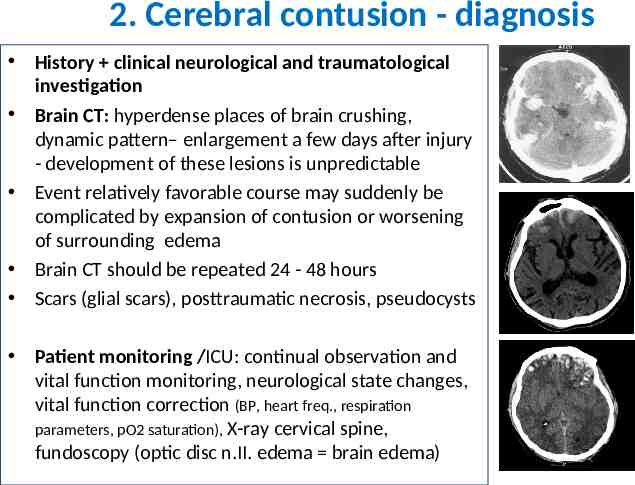
2. Cerebral contusion - diagnosis History clinical neurological and traumatological investigation Brain CT: hyperdense places of brain crushing, dynamic pattern– enlargement a few days after injury - development of these lesions is unpredictable Event relatively favorable course may suddenly be complicated by expansion of contusion or worsening of surrounding edema Brain CT should be repeated 24 - 48 hours Scars (glial scars), posttraumatic necrosis, pseudocysts Patient monitoring /ICU: continual observation and vital function monitoring, neurological state changes, vital function correction (BP, heart freq., respiration parameters, pO2 saturation), X-ray cervical spine, fundoscopy (optic disc n.II. edema brain edema)
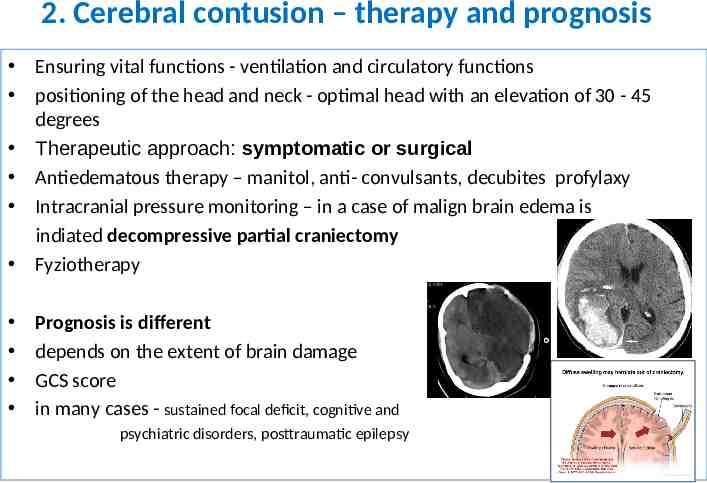
2. Cerebral contusion – therapy and prognosis Ensuring vital functions - ventilation and circulatory functions positioning of the head and neck - optimal head with an elevation of 30 - 45 degrees Therapeutic approach: symptomatic or surgical Antiedematous therapy – manitol, anti- convulsants, decubites profylaxy Intracranial pressure monitoring – in a case of malign brain edema is indiated decompressive partial craniectomy Fyziotherapy Prognosis is different depends on the extent of brain damage GCS score in many cases - sustained focal deficit, cognitive and psychiatric disorders, posttraumatic epilepsy
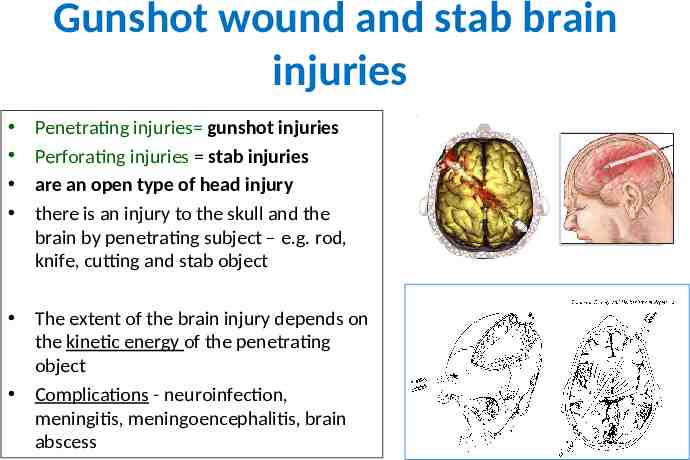
Gunshot wound and stab brain injuries Penetrating injuries gunshot injuries Perforating injuries stab injuries are an open type of head injury there is an injury to the skull and the brain by penetrating subject – e.g. rod, knife, cutting and stab object The extent of the brain injury depends on the kinetic energy of the penetrating object Complications - neuroinfection, meningitis, meningoencephalitis, brain abscess
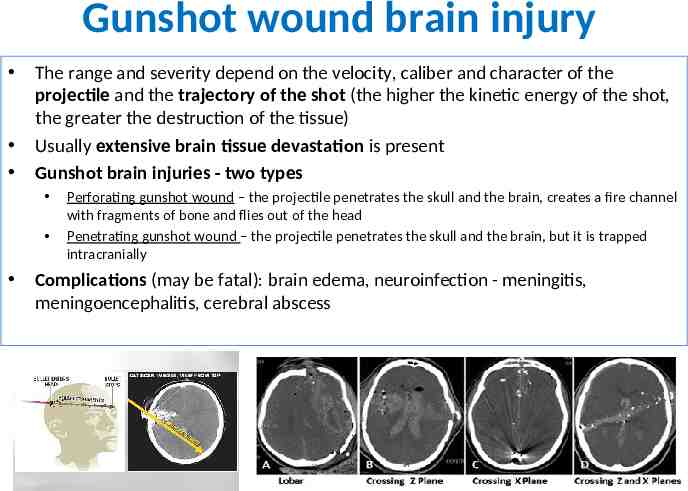
Gunshot wound brain injury The range and severity depend on the velocity, caliber and character of the projectile and the trajectory of the shot (the higher the kinetic energy of the shot, the greater the destruction of the tissue) Usually extensive brain tissue devastation is present Gunshot brain injuries - two types Perforating gunshot wound – the projectile penetrates the skull and the brain, creates a fire channel with fragments of bone and flies out of the head Penetrating gunshot wound – the projectile penetrates the skull and the brain, but it is trapped intracranially Complications (may be fatal): brain edema, neuroinfection - meningitis, meningoencephalitis, cerebral abscess
Gunshot wound brain injury Diagnosis: Inspection of the entry site /shot X-ray, CT scan – skull injury, bone fragments in the fire channel and locating the projectile (at the aperture) brain CT- brain tissue damage, brain contusion around the fire channel and hematoma Therapy: surgical antibiotics (14 days) Prognosis: always very severe damage total mortality - 90 % up to 70 % of patients die before hospital treatment
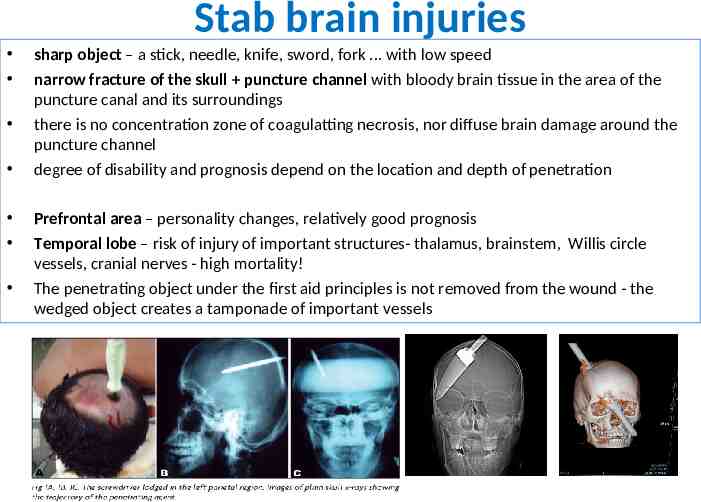
Stab brain injuries sharp object – a stick, needle, knife, sword, fork . with low speed narrow fracture of the skull puncture channel with bloody brain tissue in the area of the puncture canal and its surroundings there is no concentration zone of coagulatting necrosis, nor diffuse brain damage around the puncture channel degree of disability and prognosis depend on the location and depth of penetration Prefrontal area – personality changes, relatively good prognosis Temporal lobe – risk of injury of important structures- thalamus, brainstem, Willis circle vessels, cranial nerves - high mortality! The penetrating object under the first aid principles is not removed from the wound - the wedged object creates a tamponade of important vessels
Stab brain injuries Diagnosis – Brain CT - clarifies the depth and magnitude of brain damage – CT brain- bone window - useful for indicating skull plastic surgery or removal of bone fragments, foreign body from brain tissue – AG brain vessels – suspected vascular posttraumatic complications Therapy- perforating brain injuries - surgical – craniotomy and with the revision of the punch or fire channel – drainage of bloody brain tissue – removing available foreign bodies and bone fragments – surgical treatment does not interfere with deep structures! (brainstem, thalamus) – maximal carefully review and treatment of the speech and visual cortex! – antibiotics - an infection profylaxy
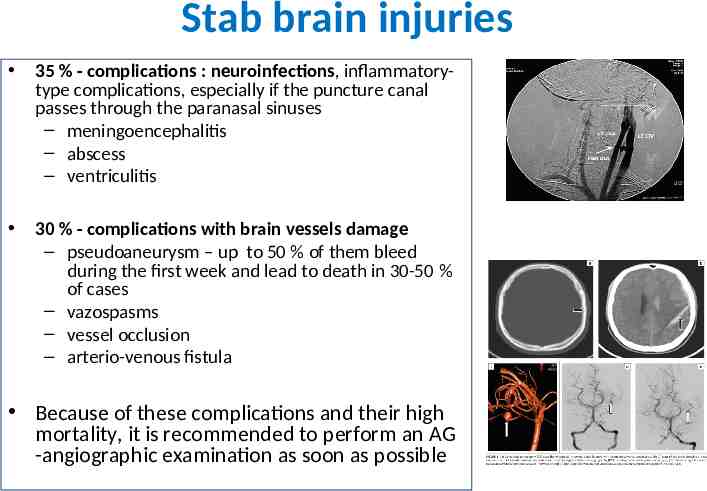
Stab brain injuries 35 % - complications : neuroinfections, inflammatorytype complications, especially if the puncture canal passes through the paranasal sinuses – meningoencephalitis – abscess – ventriculitis 30 % - complications with brain vessels damage – pseudoaneurysm – up to 50 % of them bleed during the first week and lead to death in 30-50 % of cases – vazospasms – vessel occlusion – arterio-venous fistula Because of these complications and their high mortality, it is recommended to perform an AG -angiographic examination as soon as possible
Secondary brain injuries Primary head injury can cause secondary brain injury 1.Epidural bleeding 2.Subdural bleeding 3.Intracerebral traumatic bleeding 4.Traumatic subarachnoidal bleeding
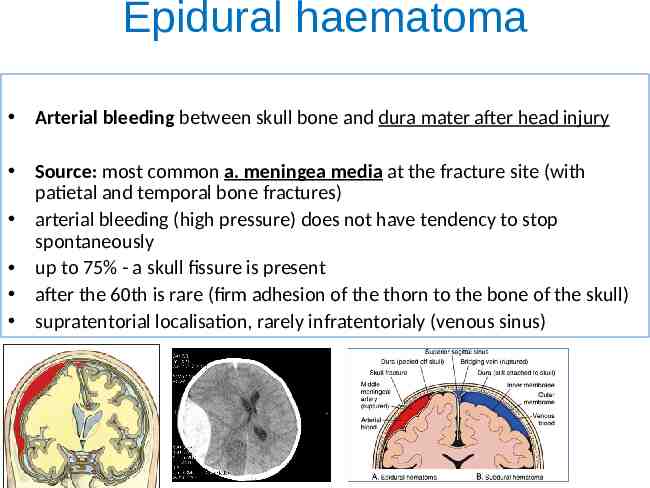
Epidural haematoma Arterial bleeding between skull bone and dura mater after head injury Source: most common a. meningea media at the fracture site (with patietal and temporal bone fractures) arterial bleeding (high pressure) does not have tendency to stop spontaneously up to 75% - a skull fissure is present after the 60th is rare (firm adhesion of the thorn to the bone of the skull) supratentorial localisation, rarely infratentorialy (venous sinus)
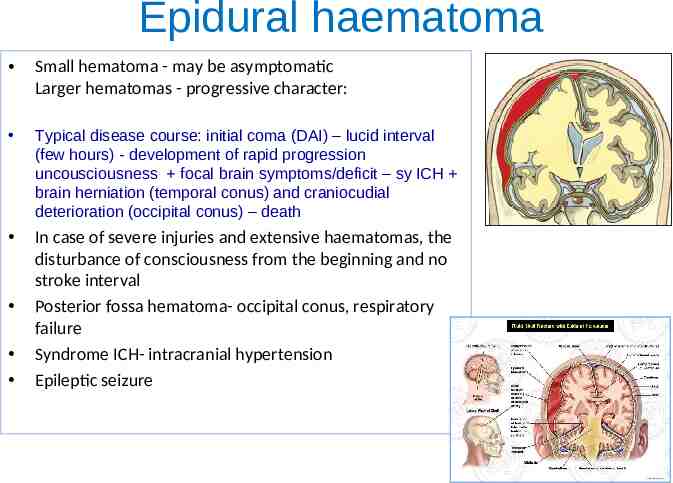
Epidural haematoma Small hematoma - may be asymptomatic Larger hematomas - progressive character: Typical disease course: initial coma (DAI) – lucid interval (few hours) - development of rapid progression uncousciousness focal brain symptoms/deficit – sy ICH brain herniation (temporal conus) and craniocudial deterioration (occipital conus) – death In case of severe injuries and extensive haematomas, the disturbance of consciousness from the beginning and no stroke interval Posterior fossa hematoma- occipital conus, respiratory failure Syndrome ICH- intracranial hypertension Epileptic seizure
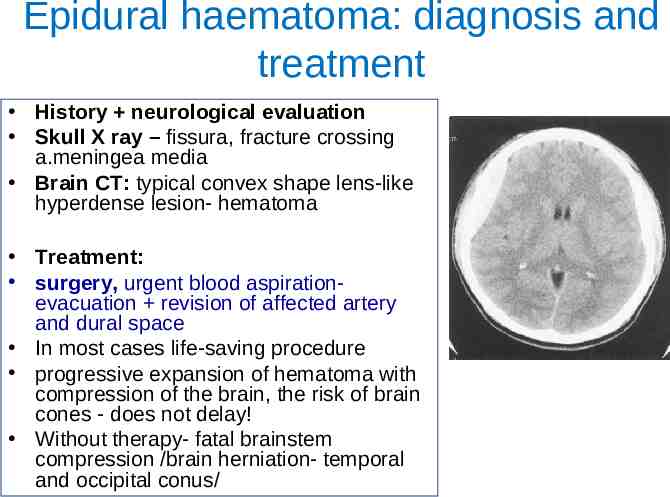
Epidural haematoma: diagnosis and treatment History neurological evaluation Skull X ray – fissura, fracture crossing a.meningea media Brain CT: typical convex shape lens-like hyperdense lesion- hematoma Treatment: surgery, urgent blood aspirationevacuation revision of affected artery and dural space In most cases life-saving procedure progressive expansion of hematoma with compression of the brain, the risk of brain cones - does not delay! Without therapy- fatal brainstem compression /brain herniation- temporal and occipital conus/
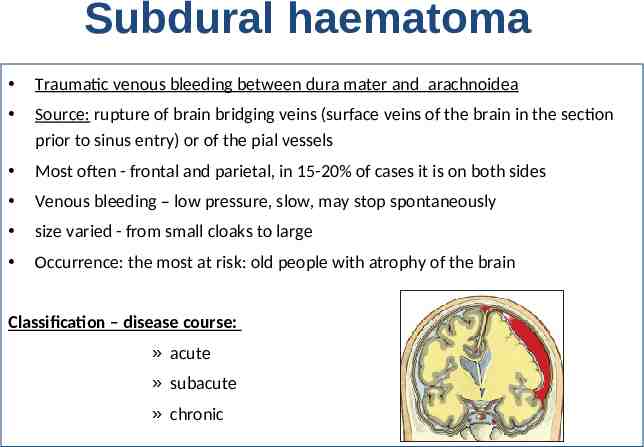
Subdural haematoma Traumatic venous bleeding between dura mater and arachnoidea Source: rupture of brain bridging veins (surface veins of the brain in the section prior to sinus entry) or of the pial vessels Most often - frontal and parietal, in 15-20% of cases it is on both sides Venous bleeding – low pressure, slow, may stop spontaneously size varied - from small cloaks to large Occurrence: the most at risk: old people with atrophy of the brain Classification – disease course: » acute » subacute » chronic
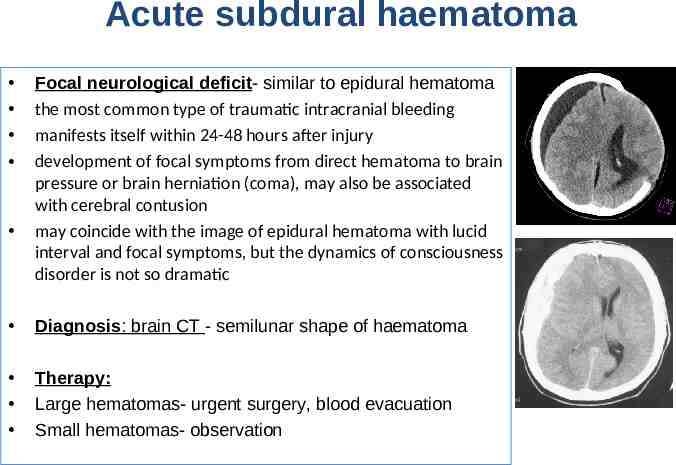
Acute subdural haematoma Focal neurological deficit- similar to epidural hematoma the most common type of traumatic intracranial bleeding manifests itself within 24-48 hours after injury development of focal symptoms from direct hematoma to brain pressure or brain herniation (coma), may also be associated with cerebral contusion may coincide with the image of epidural hematoma with lucid interval and focal symptoms, but the dynamics of consciousness disorder is not so dramatic Diagnosis: brain CT - semilunar shape of haematoma Therapy: Large hematomas- urgent surgery, blood evacuation Small hematomas- observation
Subacute subdural hematoma manifests itself within 3 weeks of injury more frequent in older age dominated progressive consciousness disorder, headache, dizziness and light palsy/ hemiparesis
Chronic subdural haematoma Slow progressive or persistent symptoms Less severe disease course and symptoms The onset of several weeks to months after the head injury Own bleeding does not clinically occur in the acute phase Chronic headache, ICH syndrome, hemiparesis, psychic changes, apathy, balance disorders, speech disorder (aphasia), epileptic seizures Occurrence: chronic alcoholics, people with blood clotting disorder, infants In the elderly - even after the banal head injury Can be undiagnosed or silent Unrecognized - an image of progressive dementia, incontinence, walking disorders, and can be mistakenly evaluated as Alzheimer's disease, brain tumor in the frontal region, dementia of alcoholics Often slight head injury Haematoma- blood/Hb metabolic changes are osmotic active – water, lesion enlargement hygroma Complications: ICH syndrome, brain herniation
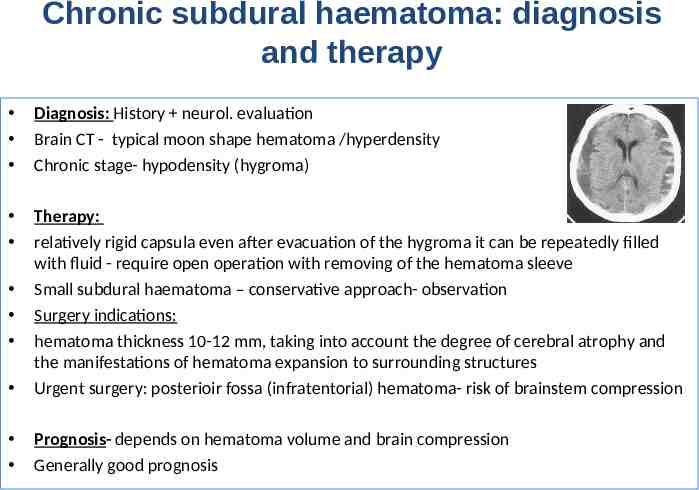
Chronic subdural haematoma: diagnosis and therapy Diagnosis: History neurol. evaluation Brain CT - typical moon shape hematoma /hyperdensity Chronic stage- hypodensity (hygroma) Therapy: relatively rigid capsula even after evacuation of the hygroma it can be repeatedly filled with fluid - require open operation with removing of the hematoma sleeve Small subdural haematoma – conservative approach- observation Surgery indications: hematoma thickness 10-12 mm, taking into account the degree of cerebral atrophy and the manifestations of hematoma expansion to surrounding structures Urgent surgery: posterioir fossa (infratentorial) hematoma- risk of brainstem compression Prognosis- depends on hematoma volume and brain compression Generally good prognosis
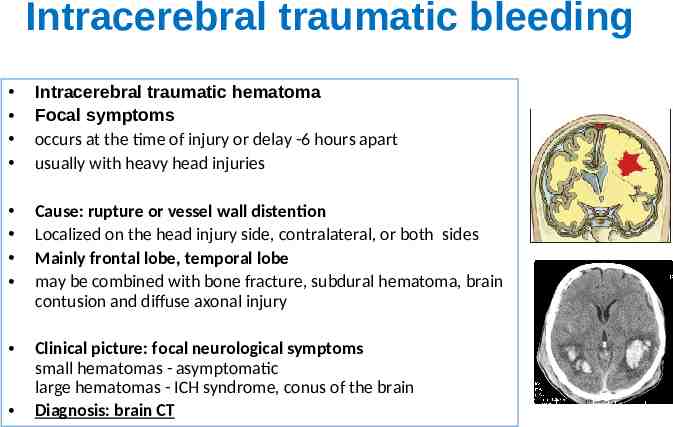
Intracerebral traumatic bleeding Intracerebral traumatic hematoma Focal symptoms occurs at the time of injury or delay -6 hours apart usually with heavy head injuries Cause: rupture or vessel wall distention Localized on the head injury side, contralateral, or both sides Mainly frontal lobe, temporal lobe may be combined with bone fracture, subdural hematoma, brain contusion and diffuse axonal injury Clinical picture: focal neurological symptoms small hematomas - asymptomatic large hematomas - ICH syndrome, conus of the brain Diagnosis: brain CT
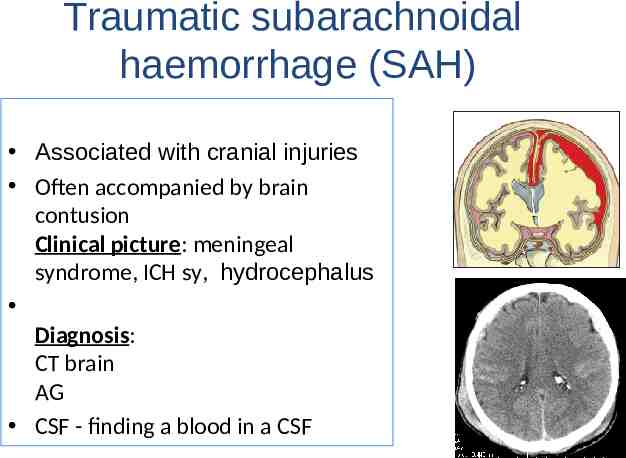
Traumatic subarachnoidal haemorrhage (SAH) Associated with cranial injuries Often accompanied by brain contusion Clinical picture: meningeal syndrome, ICH sy, hydrocephalus Diagnosis: CT brain AG CSF - finding a blood in a CSF
Postraumatic syndromes 1. 2. 3. 4. 5. 6. Brain edema and ICH syndrome Brain congestion, neuroinfection (meningitis, brain abscess), likvorhea Epileptic seizures and posttraumatic epilepsy Hydrocephalus Posttraumatic syndrome, irritability, instability, diziness, sleep problems, emotions, mood, . Dementia pugilistica Posttraumatic parkinsonism
Posttraumatic complications and syndromes The critical period for the development of secondary brain damage is the period immediately after the injury Clinical status progression and secondary brain damage can also be caused by many extracerebral causes: hypovolaemia hypotension hypoxia or hypercapnia respiratory distress pulmonary embolism, adult respiratory distress syndrome (ARDS) infection disseminated coagulopathy, organ failure arhytmia
ICH syndrome Brain edema: Generalized, local or around focal lesion Hemispheric edema - is caused by the progression of focal edema Edema is vasogenic, less cytotoxic ICH sy syndrome of intracranial hypertension: worsening of cerebral perfusion promotes further worsening of edema overpressure of central structures to contralateral side ide by more than 10-12 mm - it is necessary to consider decompressive partial craniectomy Early detection of critical IC pressure increase – by IC pressure monitoring Diagnosis of brain edema: brain CT Treatment: conservative-anti-edematous (mannitol) malignant edema - decompressive partial craniectomy (temporary local removal of calves beyond the largest edema)
Posttraumatic complications Brain congestion (vascular swelling, brain hyperaemia) increased cerebral blood volume, followed by increased brain volume stasis in the vein brain system, post-vasoprevention and vasodilation Neuroinfections - complications of open penetrating skull injuries: meningitis, meningoencephalitis, abscess of the brain Liquorrhea - CSF (5 to 10% of patients with skull base fracture) pathological communication (fistula) between the subarachnoid and extracranial space: the nasal leakage rhinorhea, or the ear otorhea the risk of posttraumatic cranial hypotension and bacterial meningitis DG: isotopic examination by radionuclide Treatment: head lift, antibiotics, if it lasts for more than 2 weeks, while fistula persists, recommended plastic surgery of the dura mater
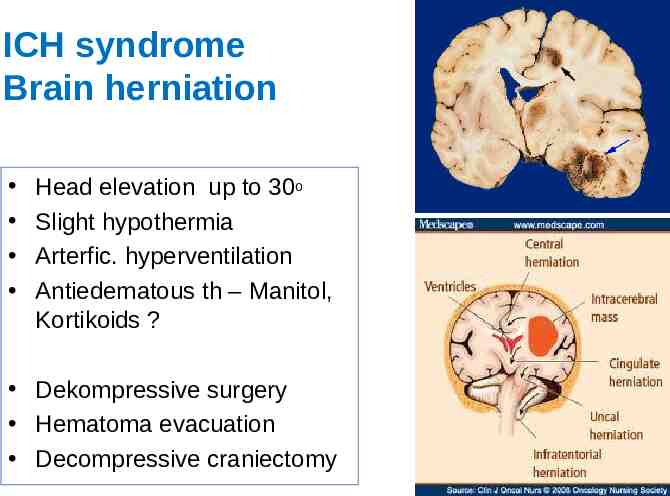
ICH syndrome Brain herniation Head elevation up to 30o Slight hypothermia Arterfic. hyperventilation Antiedematous th – Manitol, Kortikoids ? Dekompressive surgery Hematoma evacuation Decompressive craniectomy
Posttraumatic complications Hydrocephalus slowed CSF reabsorption after brain injury communicating normotensive hydrocephalus - cognitive impairment (dementia), walking disorder and incontinence, DG: Brain CT Treatment: surgery temporary or permanent shunt - ventriculoperitoneal drainage with removal CSF from the ventricle into the peritoneal abdominal cavity Epileptic seizures 5-10% of patients with craniocerebral trauma Early post-traumatic epileptic seizures (within 1-2 weeks of injury) – symptomatic Late - the development of epilepsy brain injury have a 29-fold higher risk of developing epilepsy than a normal population Cause: hematomas, contusive lesions, fragments of bone with impression The greatest risk of late seizures - 0.5-2 years from head injury and 10 GCS Treatment: anti-convulsants (2 weeks after head / brain injury)

Spine and spinal cord injuries
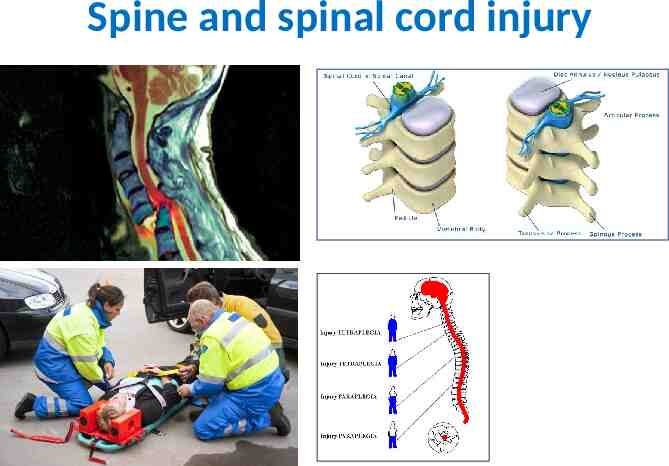
Spine and spinal cord injury
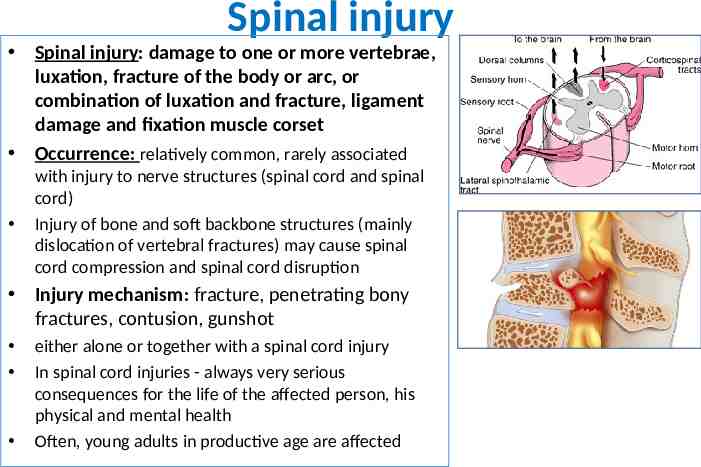
Spinal injury Spinal injury: damage to one or more vertebrae, luxation, fracture of the body or arc, or combination of luxation and fracture, ligament damage and fixation muscle corset Occurrence: relatively common, rarely associated with injury to nerve structures (spinal cord and spinal cord) Injury of bone and soft backbone structures (mainly dislocation of vertebral fractures) may cause spinal cord compression and spinal cord disruption Injury mechanism: fracture, penetrating bony fractures, contusion, gunshot either alone or together with a spinal cord injury In spinal cord injuries - always very serious consequences for the life of the affected person, his physical and mental health Often, young adults in productive age are affected
Spinal injury World incidence of traumatic spinal cord injuries:15 to 30 cases per million inhabitants per year USA: 28-50 cases/million inhabitants per year Slovakia: 20 cases/million inhabitants per year, of which about ¼ is a complete lesion of the spinal cord Up to 80% is between 18-35 years of age Men are 2,5 to 3 times more than women 55 % of spinal cord injuries are reported in road accidensts 30 % in industry and 15% in sport The most common causes of spinal cord trauma are road accidents, sports injuries, height drops, violent and gunshooting injuries
Commotio medullae spinalis Reversible spinal cord injury, no organic changes Reversible loss of spinal functions followed by full improvement within 24 - 72 hours (usually several minutes to hours) Causes: fall from a height or crush Most common levels: C 5-7, Th 10 - L1 and Th5 KO: spinal shock, acute transversal spinal lesion with quadriplegia or paraplegia and urinary retention – Cause: spinal cord edema, temporary ischemia or depolarization of cell membranes. There is no complete transversal spinal cord lesion, as some functions remain preserved; typical is the volatile and transient finding of a neurological deficit Therapy: Lihgt form: do not required treatment, sponatneous complete improvement Severe forms: steroids (methylprednisolone i.v. ) Analgetics, sedatives, thrombosis profylaxy (low molec. Heparins) Prognosis: generally good, most cases improve ad integrum
Spinal cord injury most commonly associated with spinal cord injury as a result of luxation or vertebral fractures, spinal cord or spinal cord compression occurs rarely spinal cord injury is present without simultaneous spinal vertebres (in children and adolescents) Mechanism of action- spinal cord injury: direct spinal cord destruction by injury spinal cord compression by hematoma, bone fragments, prolapsed intervertebral disc spinal cord ischemia due to spinal artery injury or compression
Spinal cord injury Depending on the extent of injury we divide the traumatic lesions of the spinal cord: A – partial, incomplete spinal cord lesion – 55 % spinal cord injuries – Some modality of sensitivity or motor function remains preserved (e.g. central spinal cord lesion syndrome) – Right after the injury, some incomplete spinal lesions may be manifested by a picture of complete plegia as a result of spinal shock B – total, complete transverzal spinal cord lesion – 45 % spinal cord injuries – The spinal cord is affected by necrosis due to ischemia or tissue dilaceration – There are no motor and sensory functions preserved distally to the wound site – Interruption of sympathetic nerves leads to hypotension and below the level of injury is loss of blood vessels tonus, stagnation of venous blood flow (risk of venous thrombosis) – Bradycardia - the result of predominance of parasympathetic tonus – This condition is part of the „neurogenic shock“ - characterized by haemodynamic triad of hypotension, bradycardia and peripheral vasodilation from discontinuation of sympathetic innervation in acute spinal cord injury, especially above the level of Th6 segment
Primary spinal cord injury In spinal cord injury: primary and secondary spinal cord injury occurs Primary injury: mechanical spinal cord injury by concussion, tearing, squirting, compression, or indirectly by extradural processes - hematoma, tumor, metastasis It occurs at the time of injury and is most often caused by bone structures fractures, or sequestration of the intervertebral disc The result is bleeding and necrosis of the tissue from the oppression and shear force Tachycardia, later bradycardia and blood pressure fluctuation, hypotension and hypoxia Local auroregulation changing mechanisms leads to bleeding occurs mainly in the spinal cord gray matter, leads to vasospasms and thrombosis
Secondary spinal cord injury consequence of auto-destruction, disturbances in blood supply to the tissue, disturbed vascular supply by arterial injury, thrombosis, or hypoperfusion and spinal shock hypoxia massive release of cytokines, neurotoxins, arachidonic acid, free radicals and prostaglandins, which further aggravate the state of already damaged tissue These factors leads to worsening of blood flow in the spinal cord and aggravate edema, which extends several segments up and down from the site of damage Capillary damage, haemorrhage - traumatic hematomyelia and secondary ischaemia of mainly spinal cord gray matter - myelomalatia and necrosis occur Protection of the spinal cord from immediate damage resulting from primary injury is not possible therapy may only be aimed at avoiding secondary changes in the tissue Secondary changes begin already in the first hours after the injury and have a significant impact on the outcome
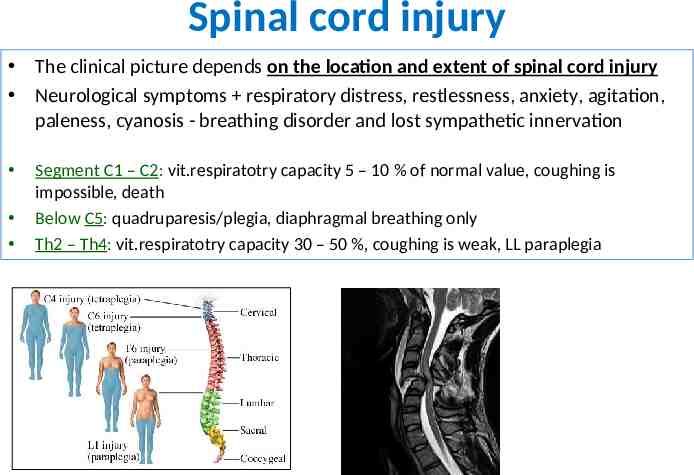
Spinal cord injury The clinical picture depends on the location and extent of spinal cord injury Neurological symptoms respiratory distress, restlessness, anxiety, agitation, paleness, cyanosis - breathing disorder and lost sympathetic innervation Segment C1 – C2: vit.respiratotry capacity 5 – 10 % of normal value, coughing is impossible, death Below C5: quadruparesis/plegia, diaphragmal breathing only Th2 – Th4: vit.respiratotry capacity 30 – 50 %, coughing is weak, LL paraplegia
Below Th11: minimal rspir. insufficiency, LL paraplegia Brown-Séquard syndrome Syndrome anterior spinal cord lesion- ventral spinal compression, syndrome a.spinalis anterior, syndrome of syringomyelic dissociation Syndrome central spinal cord injury Syndrome posterior spinal columns Syndrome epiconus medullaris: segment L4 – S2 Syndrome conus medullaris: segmentov S3 – Co3 Syndrome cauda equina: roots L3 – S5
Spinal cord injury- spinal shock Transient depression of all sensitive and motor functions connected to autonomous innervation lost right after spinal injury the loss of all spinal functions and reflexes distal to the site of the injury at the beginning, we find the image of the flaccid plegia (2 weeks to several months) then develops spastic paresis / plegia (usually spastic paraplegia of the lower limbs with a disorder of urinary and stool control) An unfavorable prognostic symptom: - presence of a complete transverse lesion more than 24 hours - priapism (pathological painful penile erection) - prolonged plantar leg flexion
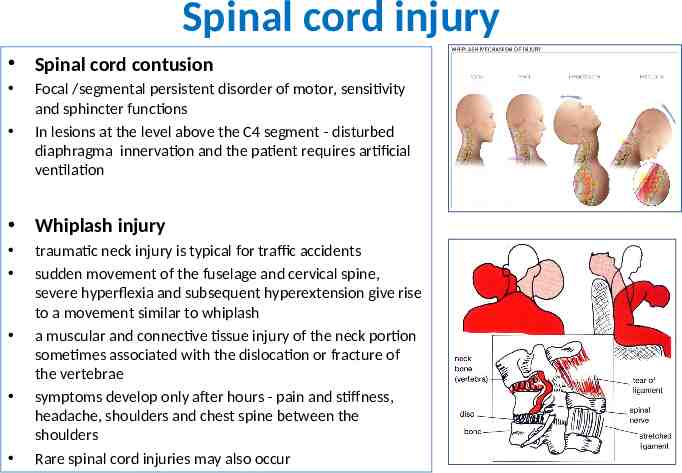
Spinal cord injury Spinal cord contusion Focal /segmental persistent disorder of motor, sensitivity and sphincter functions In lesions at the level above the C4 segment - disturbed diaphragma innervation and the patient requires artificial ventilation Whiplash injury traumatic neck injury is typical for traffic accidents sudden movement of the fuselage and cervical spine, severe hyperflexia and subsequent hyperextension give rise to a movement similar to whiplash a muscular and connective tissue injury of the neck portion sometimes associated with the dislocation or fracture of the vertebrae symptoms develop only after hours - pain and stiffness, headache, shoulders and chest spine between the shoulders Rare spinal cord injuries may also occur
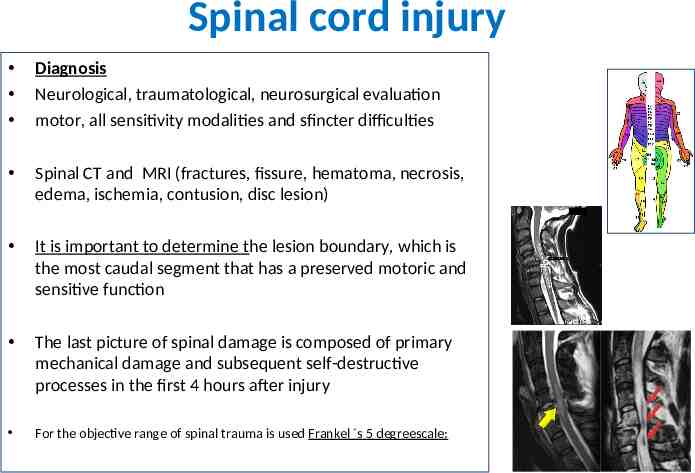
Spinal cord injury Diagnosis Neurological, traumatological, neurosurgical evaluation motor, all sensitivity modalities and sfincter difficulties Spinal CT and MRI (fractures, fissure, hematoma, necrosis, edema, ischemia, contusion, disc lesion) It is important to determine the lesion boundary, which is the most caudal segment that has a preserved motoric and sensitive function The last picture of spinal damage is composed of primary mechanical damage and subsequent self-destructive processes in the first 4 hours after injury For the objective range of spinal trauma is used Frankel s 5 degreescale:
Spinal cord injury Therapy Dynamic process the full range of injury can only occur after some time Incomplete lesion may go to complete, the extent of the injury is aggravated by one to two segments above the initial level in hours and days Respiratory complication of spinal trauma First Aid and Patient Transport Principles: stabilization and fixation of the injured spine during patient's transport minimize manipulation, maintain normal spinal axis position transport on a hard pad or in a vacuum mattress fix the neck with a hard - Philadelphia collar it is necessary to predict spinal cord injury and to take precautions to prevent deterioration of the spine, correction of respiratory distress (supportive breathing, intubation and artificial ventilation), cardiac activity and possible hypotension
Spinal cord injury Early administration of corticosteroids Methylprednisolone high dose 30 mg/kg i.v. for 45 minutes and after 15 minutes - 5.4 mg / kg for 23 hours (the procedure is valid if the 1st dose is administered within 3 hours after the injury - If corticosteroids can be administered from 3 to 8 hours after the injury, it is continued continuously for 48 hours - The aim of corticotherapy is to reduce secondary changes in the spinal cord Surgery to prevent further deterioration of the neurological condition to create optimal conditions for restoration of functions and to ensure decompression of the spinal cord, reposition and stabilization of bone structures
Spinal cord injury Symptomatic therapy Analgetics, prevention of decubitus and infections, treatment of spasticity, disorders of autonomic regulation, psychotherapy Sexual dysfunction therapy Transuretral catheterization – sfincter problems Suprapubic epicystostomy neurogenic reflex bladder: spinal cord lesion above segment S2 - S4, the patient does not feel the bladder filling, the bladder is emptied spontaneously, reflexively, automatically atonic bladder: spinal cord injury at or below the Budge Center, the bladder must be emptied passively. Rehabilitation: the focus of concurrent treatment of spinal cord injuries restoring the affected functions and making the best use of preserved functions and muscle potential preventing the development of muscular atrophy
Spinal cord injury- prognosis Prognosis is individual, depends on severity and location neurological deficit may increase even further over the hours and days after the injury extending neurological deficits cranially is a sign of deterioration complete spinal lesions have an adverse prognosis, with permanent loss of motor activity, sensitivity, sphincter control, and impotence upper cervical segments lesion – may progress to ascendent necrosis of medulla oblongata Complications: decubites, aspiration, hypothermia and respiratory problems At complete spinal cord lesion - only about 5 % of the recovery is available The dynamics of the change in the first hours and days is important: – if complete paralysis persists for more than 72 hours – improvement is not possible – if at least minimal sensitive innervation is maintained – 50 % chance of restoring the ability to walk