Fallon Health Mass Collaborative Provider Credentialing
7 Slides164.79 KB
Fallon Health Mass Collaborative Provider Credentialing Symposium April 27, 2016
Provider Credentialing Credentialing Process Fallon Health credentials Providers initially, and then every 2 years based on the date of the birth cycle using the HCAS process Import files on a daily basis Credentials Associates audits for accuracy Providers are approved daily by the Fallon Health Medical Director or are forwarded to the Fallon Health Credentials Committee for second level review The Fallon Health Credentials Committee meets the fourth Wednesday of each month
Provider Credentialing Credentialing turn around time Based upon the Massachusetts Statement of Principles for MD/DO Fallon Health credentials 95% of clean and completed files within 30 days or less
Provider Credentialing Process Improvements Online sites that allow Hospital and Training verifications Accept electronic signatures for Hospital verifications CVs updated for initial credentialing in month/year format
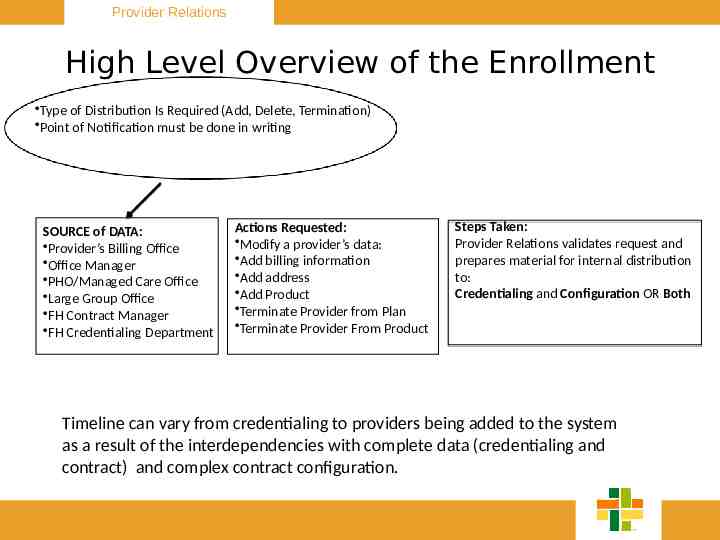
Provider Relations High Level Overview of the Enrollment Type of Distribution Is Required (Add, Delete, Termination) Point of Notification must be done in writing SOURCE of DATA: Provider’s Billing Office Office Manager PHO/Managed Care Office Large Group Office FH Contract Manager FH Credentialing Department Actions Requested: Modify a provider’s data: Add billing information Add address Add Product Terminate Provider from Plan Terminate Provider From Product Steps Taken: Provider Relations validates request and prepares material for internal distribution to: Credentialing and Configuration OR Both Timeline can vary from credentialing to providers being added to the system as a result of the interdependencies with complete data (credentialing and contract) and complex contract configuration.
Provider Credentialing Questions

Provider Credentialing Contact info Sandy Dussault 508-368-9819 [email protected]