The following document is for historical purposes and is no
30 Slides7.58 MB
The following document is for historical purposes and is no longer being updated. Please go to the COVID-19 Vaccination Clinical & Professional Resources for more recent information. 1
Building Confidence in COVID-19 Vaccines Among Your Patients: Tips for the Healthcare Team Developed by: CDC COVID-19 Response Vaccine Task Force June 2021 cdc.gov/coronavirus
Presentation Overview Elements of vaccine confidence Strategies for building vaccine confidence Strategies for talking with patients about COVID-19 vaccine Communication resources 3

Elements of Vaccine Confidence
Defining Vaccine Confidence Vaccine confidence is the trust that patients, parents, or healthcare professionals have in: – recommended vaccines; – professionals who administer vaccines; and – processes and policies that lead to vaccine development, licensure, manufacturing, and recommendations for use. 5
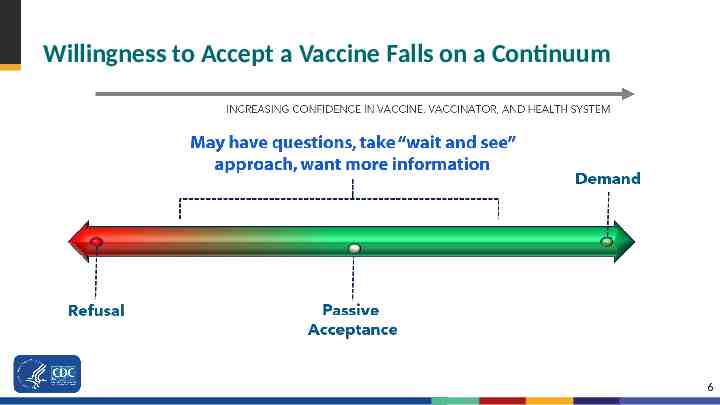
Willingness to Accept a Vaccine Falls on a Continuum 6

Strategies for Building Vaccine Confidence
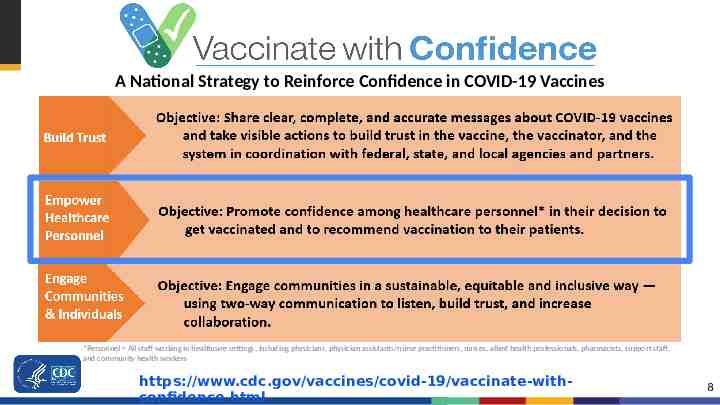
A National Strategy to Reinforce Confidence in COVID-19 Vaccines *Personnel All staff working in healthcare settings, including physicians, physician assistants/nurse practitioners, nurses, allied health professionals, pharmacists, support staff, and community health workers https://www.cdc.gov/vaccines/covid-19/vaccinate-withconfidence.html 8
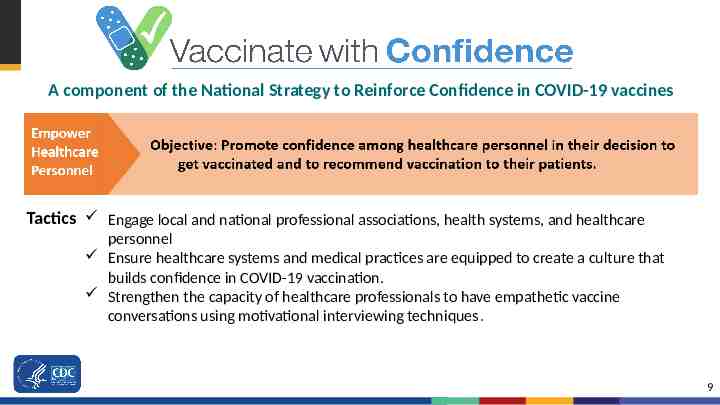
A component of the National Strategy to Reinforce Confidence in COVID-19 vaccines Tactics Engage local and national professional associations, health systems, and healthcare personnel Ensure healthcare systems and medical practices are equipped to create a culture that builds confidence in COVID-19 vaccination. Strengthen the capacity of healthcare professionals to have empathetic vaccine conversations using motivational interviewing techniques. 9
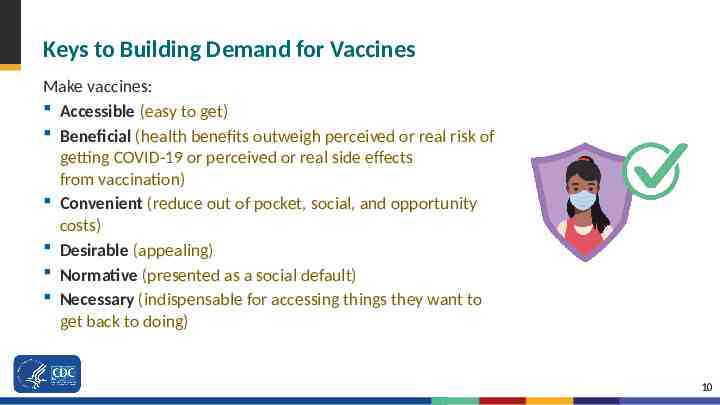
Keys to Building Demand for Vaccines Make vaccines: Accessible (easy to get) Beneficial (health benefits outweigh perceived or real risk of getting COVID-19 or perceived or real side effects from vaccination) Convenient (reduce out of pocket, social, and opportunity costs) Desirable (appealing) Normative (presented as a social default) Necessary (indispensable for accessing things they want to get back to doing) 10
Strategies to Build COVID-19 Vaccine Confidence Among Healthcare Professionals Host discussions where personnel at different levels can ask questions and share concerns in a safe space. Share key messages with staff through emails, breakroom posters, and other channels. Highlight the experiences of employees who were initially hesitant to get vaccinated, but who later made the decision to get the vaccine. Encourage senior leaders to be vaccine champions. 11

Talking with Patients about COVID-19 Vaccination
The Role of Healthcare Professionals Healthcare professionals are patients’ and parents’ most trusted source of information on vaccines. Your answers to their questions matter and will help them make an informed decision about getting a COVID-19 vaccination for themselves or their children. Your strong vaccine recommendation is the most important part of the conversation. www.cdc.gov/vaccines/covid-19/hcp/engaging-patients.html 13
Lead with Listening Do not make assumptions about whether your patients will choose to get vaccinated or the reasons for their decisions. – Instead, begin with an open-ended question, such as “What are your thoughts on getting a COVID-19 vaccination today?” Actively listen and seek to understand the patient’s point of view. Recognize that these conversations can take time and may continue over the course of multiple encounters. 14
Use Patient-Centered Communication Techniques Use open-ended questions to promote dialogue. Ask about readiness to vaccinate and what questions or concerns they may have. Paraphrase any information shared to show that you have heard and understood it. Praise measures already taken to protect themselves or their children from COVID-19, like mask wearing and physical distancing. Then frame vaccination as a safe and effective way to help protect them and their loved ones from getting COVID-19. Ask for permission to share more information on COVID-19 vaccines. This will foster openness and connection. 15
Respond to Questions and Concerns with Empathy Respond to questions and concerns in a non-judgmental, respectful, and empathic way. Provide accurate answers using clear, simple language. Explore questions patients ask most often about vaccines (see URLs below). Some concerns may stem from mistrust in the medical establishment or the government as result of collective or individual mistreatment and traumas. Acknowledging past traumas may promote patients’ trust in you and your message. Acknowledge uncertainty about what we don’t yet know about COVID-19 vaccines. This can help build trust. www.cdc.gov/vaccines/covid-19/hcp/answering-questions.html www.cdc.gov/coronavirus/2019-ncov/vaccines/faq.html 16
Give Your Strong Recommendation Let your patients know that you recommend COVID-19 vaccination for them. Your strong recommendation is critical for vaccine acceptance. Tailor your recommendation to include any relevant reasons why COVID-19 vaccination might be important for this particular patient. 17
Give Your Strong Recommendation (cont’d) Talk about your personal decision and experience in getting a COVID-19 vaccine and your experience treating COVID-19 patients. Share the benefits of getting vaccinated, including: – Protecting themselves and others who may be more vulnerable, and – Enabling them to get back to activities they have missed. Explain what they can do when they’ve been fully vaccinated. 18
Examples “I strongly recommend you get a COVID-19 vaccine ” “ This shot is especially important for you because of your [job/underlying health condition/vulnerable family member].” “ I believe in this vaccine so strongly that I got vaccinated as soon as it was available to me, and I recommended that everyone in my family do the same.” “I have seen what COVID-19 can do to patients and their families. I want to protect you as best I can from COVID-19 infection and complications.” 19
Key Messages About COVID-19 Vaccination 1. You can help stop the COVID-19 pandemic by getting a COVID-19 2. 3. 4. 5. vaccine. COVID-19 vaccines are safe and effective. COVID-19 vaccines are free. After COVID-19 vaccination, you might have some temporary side effects. These are normal signs that your body is building protection. Once you are fully vaccinated, you can resume most activities that you stopped doing because of the COVID-19 pandemic, such as gathering indoors with family and friends, without wearing a mask. 20
Address Misinformation About COVID-19 Vaccination by Sharing Key Facts COVID-19 vaccines cannot give you COVID-19. https://www.cdc.gov/coronavirus/2019ncov/vaccines/facts.html People who have already gotten sick with COVID-19 may still benefit from getting vaccinated. There is currently no evidence that COVID-19 vaccination causes any problems with pregnancy or fertility. COVID-19 vaccines do not change your DNA in any way. 21
Help Individuals Find Their Motivation for Getting Vaccinated Steer the conversation away from “why not?” and toward the important reasons that matter to them—their “why.” The reasons that someone may choose to get vaccinated will always be those that are most compelling to them personally. You may choose to share your reasons for getting vaccinated or discuss common goals you may have, like visiting with family safely. 22
Wrap Up the Conversation Encourage patients or parents to take at least one action, such as: – Scheduling a vaccination appointment with your office, a pharmacy, or another vaccination site, or – Reading any handouts that you provide to them. If they decline vaccination, acknowledge that this is their decision, and keep the door open to revisiting the topic during future visits. 23
It Will Take More Than One Conversation to Change Minds Vaccine hesitancy, especially when rooted in lack of trust rather than lack of information, is best addressed through trusted messengers in trusted spaces. Encourage two-way dialogue and allow space for people to ask questions. 24

Resources
Sample Email or Letter on COVID-19 Vaccination To Send to Your Patients https://www.cdc.gov/vaccines/covid-19/downloads/Sample-Physician-Letter-COVID-19-Vaccine.docx
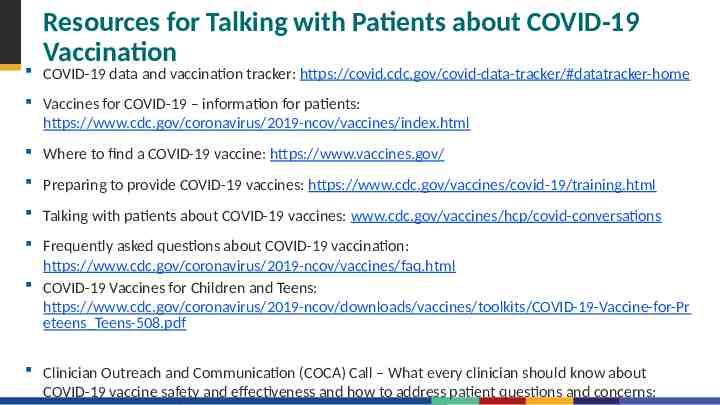
Resources for Talking with Patients about COVID-19 Vaccination COVID-19 data and vaccination tracker: https://covid.cdc.gov/covid-data-tracker/#datatracker-home Vaccines for COVID-19 – information for patients: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/index.html Where to find a COVID-19 vaccine: https://www.vaccines.gov/ Preparing to provide COVID-19 vaccines: https://www.cdc.gov/vaccines/covid-19/training.html Talking with patients about COVID-19 vaccines: www.cdc.gov/vaccines/hcp/covid-conversations Frequently asked questions about COVID-19 vaccination: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/faq.html COVID-19 Vaccines for Children and Teens: https://www.cdc.gov/coronavirus/2019-ncov/downloads/vaccines/toolkits/COVID-19-Vaccine-for-Pr eteens Teens-508.pdf Clinician Outreach and Communication (COCA) Call – What every clinician should know about COVID-19 vaccine safety and effectiveness and how to address patient questions and concerns:
COVID-19 Vaccination Communication Toolkit for Medical Centers, Clinics, and Clinicians Stickers Social media Slides Fact sheets & FAQs Posters www.cdc.gov/vaccines/covid-19/health-systems-communication-toolkit.html
Vaccine Safety Monitoring Systems Existing systems and data sources are used to monitor safety of vaccines post-authorization and post-licensure, such as: – – – – Vaccine Adverse Event Reporting System (VAERS) Vaccine Safety Datalink (VSD) Clinical Immunization Safety Assessment (CISA) Biologics Effectiveness and Safety System (BEST) New systems have been developed to monitor COVID-19 vaccine safety, such as v-safe: – Active surveillance that uses text messaging to initiate web-based survey monitoring. – Provides telephone follow up to anyone who reports medically significant adverse events. 29

For more information, contact CDC 1-800-CDC-INFO (232-4636) TTY: 1-888-232-6348 www.cdc.gov The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.