Expanding Access to Behavioral Health through Hospital and
21 Slides3.57 MB
Expanding Access to Behavioral Health through Hospital and CCBHC Collaboration Unity Center for Behavioral Health and LifeWorks NW
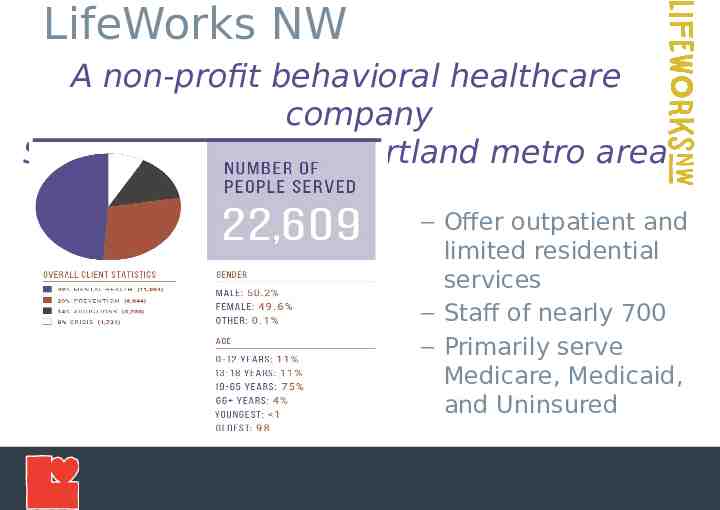
LifeWorks NW A non-profit behavioral healthcare company Serving the greater Portland metro area – Offer outpatient and limited residential services – Staff of nearly 700 – Primarily serve Medicare, Medicaid, and Uninsured
Unity Center for Behavioral Health Unique collaboration between Legacy, OHSU, Adventist Health and Kaiser to provide services to the region Community-wide effort (city, counties, state, payers, EMS, police, mental health and addictions providers- more than 30 participating agencies Facility licensed under Legacy Emanuel Medical Center 102 inpatient beds (80 adult beds, 22 adolescent beds) Adult Psychiatric Emergency Service (45-55 pts/day) Strong Peer support built into structure of Unity Built-in space for Community Providers to help navigate handoffs from Unity to community treatment and resources
History – Why? Response to community need Increasing efficiencies amongst local hospital systems (OHSU, Kaiser, Legacy, Adventist) Mitigating gaps within the system Fragmented legal, medical and psychiatric processes and services Decrease Emergency Room boarding and increase care experience Reduce Inpatient admissions 4
History – How? Built by key stakeholders within the community Hospitals Behavioral Health Providers Criminal Justice System Peers Oregon Health Authority Emergency Medical Services Counties Trauma Informed Care Framework Co-locating providers within hospital system 5
PES: Psychiatric Emergency Service 6
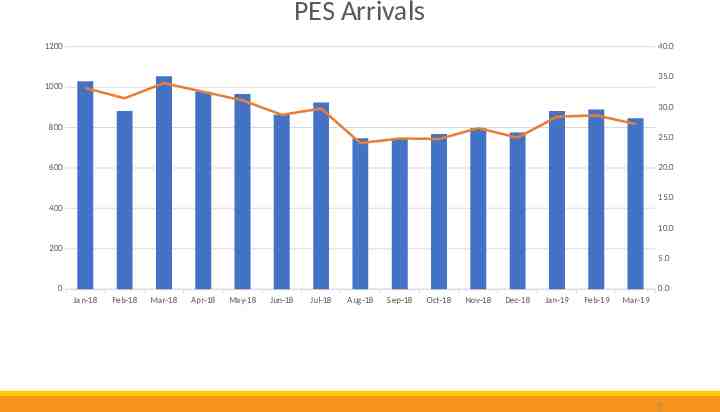
PES Arrivals 1200 40.0 35.0 1000 30.0 800 25.0 600 20.0 15.0 400 10.0 200 5.0 0 0.0 Jan-18 Feb-18 Mar-18 Apr-18 May-18 Jun-18 Jul-18 Aug-18 Sep-18 Oct-18 Nov-18 Dec-18 Jan-19 Feb-19 Mar-19 7
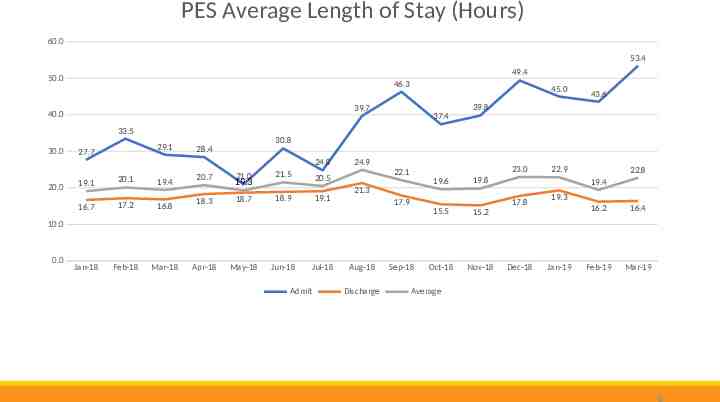
PES Average Length of Stay (Hours) 60.0 53.4 49.4 50.0 46.3 45.0 39.7 40.0 37.4 43.6 39.8 33.5 30.0 29.1 27.7 30.8 28.4 24.8 20.0 19.1 20.1 19.4 16.7 17.2 16.8 Jan-18 Feb-18 Mar-18 20.7 18.3 21.0 21.5 20.5 18.7 18.9 19.1 19.3 24.9 23.0 22.1 19.6 21.3 17.9 22.9 19.8 17.8 15.5 15.2 Oct-18 Nov-18 22.8 19.4 19.3 16.2 16.4 Feb-19 Mar-19 10.0 0.0 Apr-18 May-18 Jun-18 Jul-18 Admit Aug-18 Discharge Sep-18 Dec-18 Jan-19 Average 8
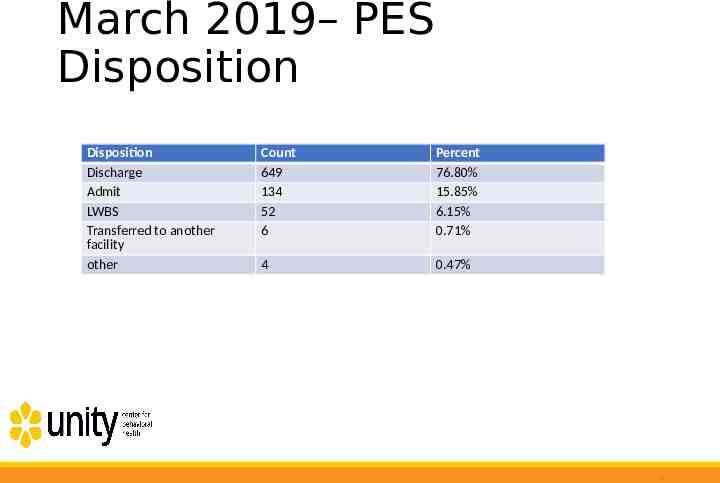
March 2019– PES Disposition Disposition Discharge Admit LWBS Transferred to another facility other Count 649 134 52 6 Percent 76.80% 15.85% 6.15% 0.71% 4 0.47% 9
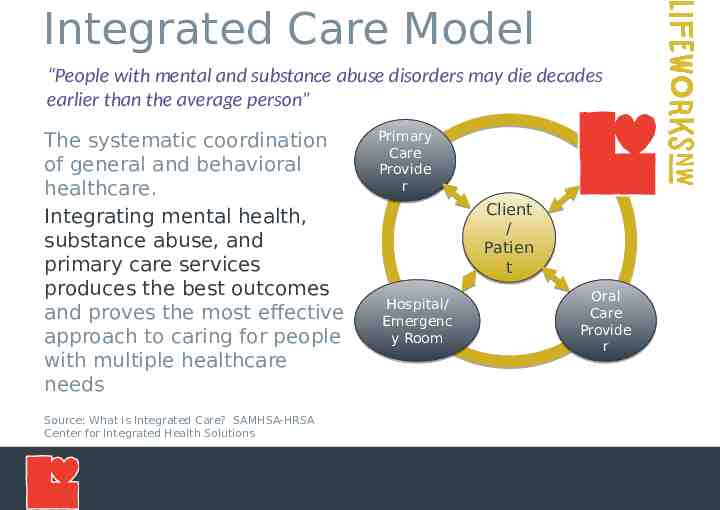
Integrated Care Model “People with mental and substance abuse disorders may die decades earlier than the average person” The systematic coordination of general and behavioral healthcare. Integrating mental health, substance abuse, and primary care services produces the best outcomes and proves the most effective approach to caring for people with multiple healthcare needs Source: What is Integrated Care? SAMHSA-HRSA Center for Integrated Health Solutions Primary Care Provide r Client / Patien t Hospital/ Emergenc y Room Oral Care Provide r
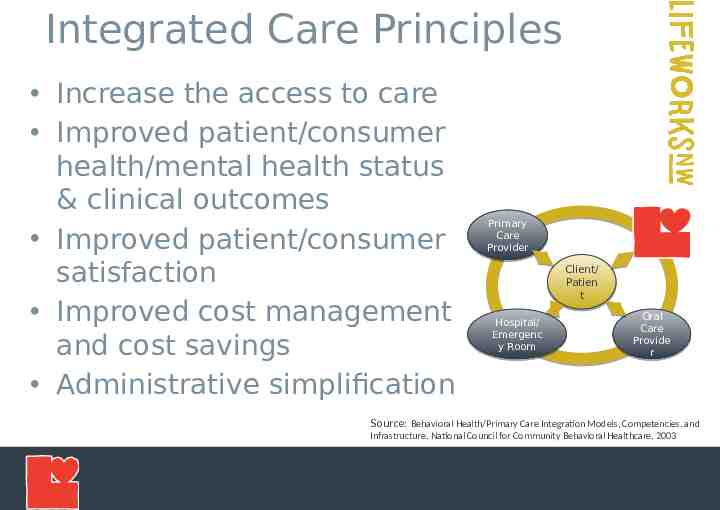
Integrated Care Principles Increase the access to care Improved patient/consumer health/mental health status & clinical outcomes Improved patient/consumer satisfaction Improved cost management and cost savings Administrative simplification Primary Care Provider Client/ Patien t Hospital/ Emergenc y Room Oral Care Provide r Source: Behavioral Health/Primary Care Integration Models, Competencies, and Infrastructure, National Council for Community Behavioral Healthcare, 2003
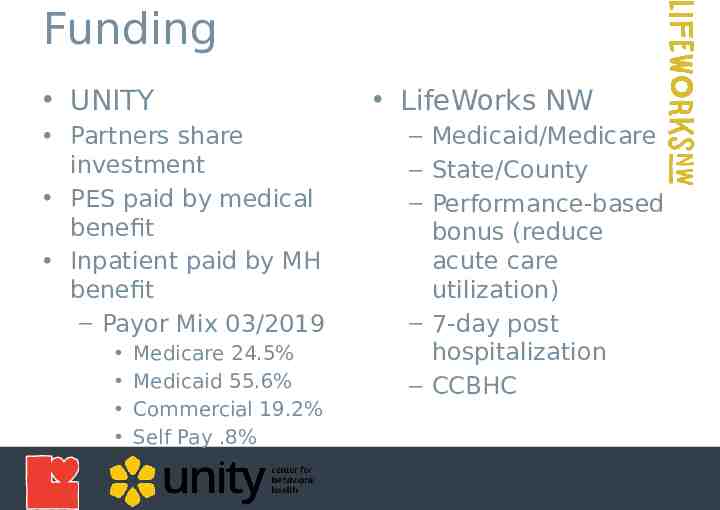
Funding UNITY Partners share investment PES paid by medical benefit Inpatient paid by MH benefit – Payor Mix 03/2019 Medicare 24.5% Medicaid 55.6% Commercial 19.2% Self Pay .8% LifeWorks NW – Medicaid/Medicare – State/County – Performance-based bonus (reduce acute care utilization) – 7-day post hospitalization – CCBHC
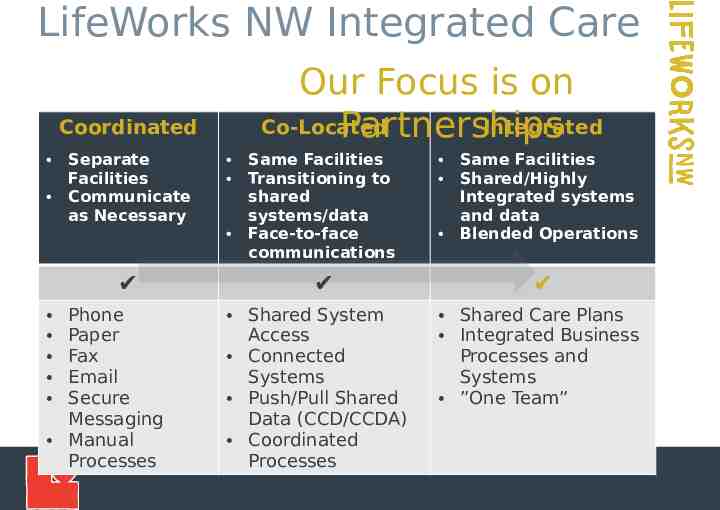
LifeWorks NW Integrated Care Our Focus is on Co-Located Integrated Partnerships Coordinated Separate Facilities Communicate as Necessary ️ Phone Paper Fax Email Secure Messaging Manual Processes Same Facilities Transitioning to shared systems/data Face-to-face communications ️ Shared System Access Connected Systems Push/Pull Shared Data (CCD/CCDA) Coordinated Processes Same Facilities Shared/Highly Integrated systems and data Blended Operations ️ Shared Care Plans Integrated Business Processes and Systems ”One Team”
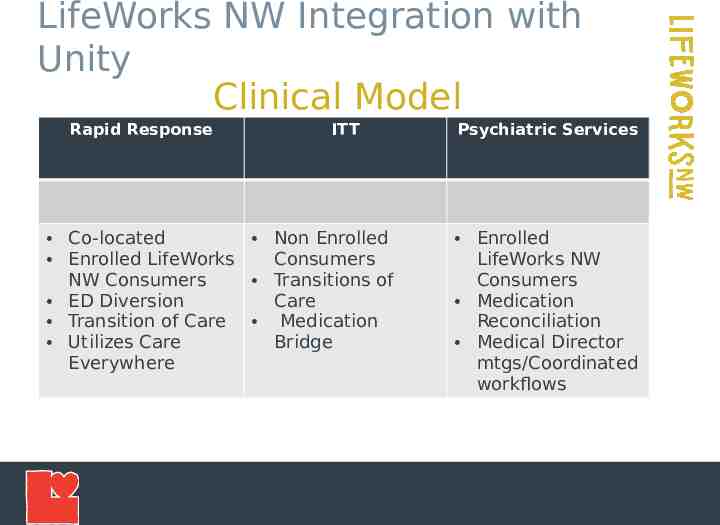
LifeWorks NW Integration with Unity Clinical Model Rapid Response ITT Co-located Non Enrolled Enrolled LifeWorks Consumers NW Consumers Transitions of ED Diversion Care Transition of Care Medication Utilizes Care Bridge Everywhere Psychiatric Services Enrolled LifeWorks NW Consumers Medication Reconciliation Medical Director mtgs/Coordinated workflows
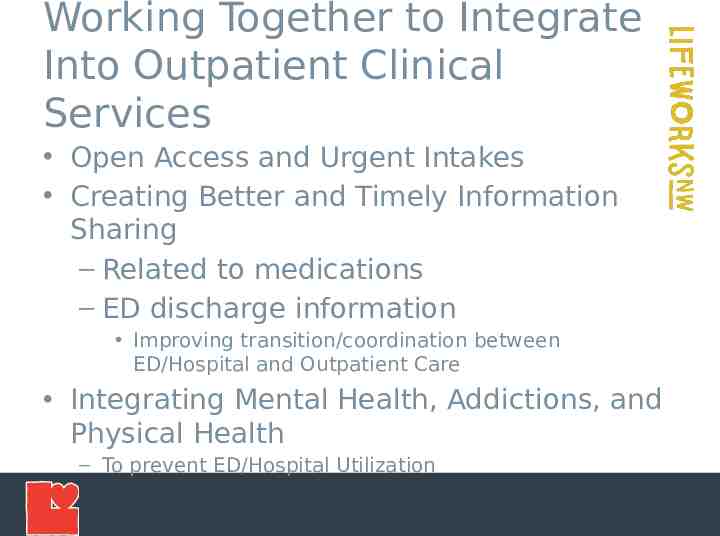
Working Together to Integrate Into Outpatient Clinical Services Open Access and Urgent Intakes Creating Better and Timely Information Sharing – Related to medications – ED discharge information Improving transition/coordination between ED/Hospital and Outpatient Care Integrating Mental Health, Addictions, and Physical Health – To prevent ED/Hospital Utilization
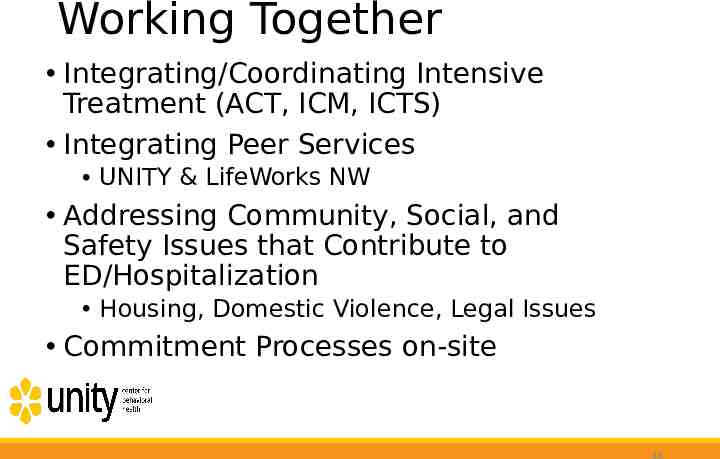
Working Together Integrating/Coordinating Intensive Treatment (ACT, ICM, ICTS) Integrating Peer Services UNITY & LifeWorks NW Addressing Community, Social, and Safety Issues that Contribute to ED/Hospitalization Housing, Domestic Violence, Legal Issues Commitment Processes on-site 16
Continuous Learning and Improvement Transitions of Care Meeting – Monthly meeting with providers Transportation Workgroup Advisory Council – Regular meeting of key stakeholders UNITY, Providers, Emergency Services, County, Medical School, Law Enforcement
Key Challenges Network of Connectivity – Integrate with multiple EHRs, HIEs – Integrate with multiple extended service providers i.e. laboratories – Integrate with multiple Collaboratives, Collectives Blending of Medical and Behavioral Health Worlds – Nomenclature – Business Processes Variance in Data Definition, Collection, and Reporting Evolving Policy Changes at Federal, State levels Primary Primary Care Care Provider Provider – Funding – Reporting Client/ Client/ Patient Patient Hospital/ Hospital/ Emergency Emergency Room Room Oral Oral Care Care Provider Provider
Innovation – What’s Needed Data Exchange Standards – Data Definitions – Common key Identifiers for record matching Flexibility & Configurability Designed into Data Exchange – Design to support the network of connectivity – Design to support integrating business processes across different organizations Role based, Rule based, Triggers, Escalation Policies, Data Selection Integrated Sign-on/System Authentication
LifeWorks NW - What’s Next? Identifying the Priority Business Processes and Data – Operationally collaborative – Healthcare service necessary Working with Partner Network – Identify gaps in current technologies and methods – Develop and establish the data exchanges and technology Establishing Partner Collaborative – Define Data Exchange Standards – Data Definitions Integrated ED Diversion/Care Plans – Utilizing Collective Medical Technology Pre-Manage Care Plans – Developing integrated client focused care plans
QUESTIONS?