Data + Analysis = Decision Support Rema Padman, PhD Professor of
94 Slides5.36 MB
Data Analysis Decision Support Rema Padman, PhD Professor of Management Science and Health Informatics The Heinz School Carnegie Mellon University MMM Program [email protected]

Outline - Day 1 Introduction – Motivation – Illustrative Examples – DSS Analysis Framework – DSS Reference Architecture – Key Challenges Decision making – Process – Strategies used by humans – Implications for decision support

Outline - Day 2 Technology Enablers – Data Management Databases Data warehousing Data marts OLAP, ROLAP, MOLAP, WOLAP – Analysis Technologies Decision analysis methods Rule-based systems Knowledge discovery and pattern recognition

Outline - Day 3 – DSS Integration, Deployment, Use Intermountain Health Care Clinical Reminder System

Information – The Emerging Capital of Healthcare Volume of Information (Diamond Cluster International, Inc.) Provider Information Processing Capacity Available Patient Information Healthcare Informatics Time

The Future- A Decision Support Focus Real time decision support at the point of care Customized disease management for the individual and the population Knowledge nodes that leverage pervasive computing infrastructure – Telemedicine – Public health

Drivers Demand Pull – Value of information – Reduction of errors – Managing information overload Technology Push – Computing and communication technologies, decision and information technologies, medical technologies,. Regulatory Push – HIPAA, Insurance reform, Patient’s bill of rights

Motivation: Value of Information “In attempting to arrive at the truth, I have applied everywhere for information, but in scarcely an instance have I been able to obtain hospital records fit for any purpose of comparison. If they could be obtained.they would show subscribers how their money was being spent, what amount of good was really being

Evidence for CDSS Adoption? DL Hunt, RB Haynes, SE Hanna, K Smith. Effects of computer-based clinical decision support systems on physician performance and patient outcomes. JAMA 1998 280: 1339-1346. Drug dosing systems Diagnostic aids Preventive care systems Other medical care All CDSS studies - 9/15 1/5 14/19 19/26 43/65

Motivation: Reducing Medical Errors 1999 IOM report on medical errors - “To Err is Human: Building A Safer Health System” – "The stunningly high rates of medical errors - resulting in deaths, permanent disability, and unnecessary suffering - are simply unacceptable in a medical system that promises first to 'do no harm,'" says William Richardson, chair of the committee that wrote the report and president and chief executive officer of the W.K. Kellogg Foundation, Battle Creek, Mich. – "Our recommendations are intended to encourage the health care system to take the actions necessary to improve safety. We must have a health care system that makes it easy to do things right and hard to do them wrong.”

Evidence for ADE Reduction? DW Bates et al. JAMA 1998 280: 1311-1316, DW Bates et al. JAMIA 2003 10:115-128. BWH interventions Applications devoted to workflow Existing, expandable clinical systems Order entry only way to enter orders – 15,000 orders a day, 400 changed due to intervention (warnings, reminders, .) – drug-allergy, drug-drug, drug-problem – drug-lab, lab-drug – drug dosing, renal dosing – appropriate dosage – drug substitution High user satisfaction

Motivation: Managing Information Overload “It is simply unrealistic to think that individuals can synthesize in their heads scores of pieces of evidence, accurately estimate the outcomes of different options, and accurately judge the desirability of those outcomes for patients.” David M. Eddy, MD, PhD JAMA 1990, 263:1265 - 1275

Technology Drivers Reduced barriers to facilitated and customized information access – Data storage, management, retrieval, and analysis technologies – Input-output technologies – Communication and networking technologies – Internet and web technologies

Technology Drivers Building efficiency, effectiveness, and quality into healthcare delivery and administration – use data in EMRs and CDRs for more than individual patient management

Regulatory Drivers HIPAA – Administrative provisions – Privacy, security provisions – . Leapfrog Group Recommendations – Computer Physician Order Entry (CPOE) – Evidence-based Hospital Referral (EHR) – ICU Physician Staffing (IPS) .

Contextual Drivers Increased risk-sharing by providers IOM reports – To Err is Human: Building a Safer health System (1999) – Crossing the Quality Chasm: A New Health System for the 21st century (2001) – Unequal Treatment: Confronting Racial and Ethnic Disparities in Healthcare (2002) – Patient Safety: Achieving a New Standard for Care (2003) Bioterrorism and biosurveillance–related objectives

Current Initiatives (EBM Solutions) Payers will focus on these co-dependent variables to reduce costs and improve care Reduced inappropriate variation and increased adherence to evidence-based guidelines by providers Increased comprehension of and adherence to evidence-based guidelines by patients.

Variation Reduction Patient Compliance - Potential Results Patient Compliance – 20-50B opportunity (UBS Warburg) Inappropriate variability – 200-300B opportunity (Juran) The two are inextricably related essential to manage how care is delivered to manage costs and improve care

Transforming Health Care with IT TABLE 1 Simple Rules for the 21st-Century Health Care Current Approach System New Rule . Care is based primarily on visits. Care is based on continuous healing relationships. Professional autonomy drives variability. Care is customized according to patient needs and values. Professionals control care. The patient is the source of control. Information is a record. Knowledge is shared and information flows freely. Decision making is based on training and experience. Decision making is evidence-based. Do no harm is an individual responsibility. Safety is a system property. Secrecy is necessary. Transparency is necessary. The system reacts to needs. Needs are anticipated. Cost reduction is sought. Waste is continuously decreased. Preference is given to professional roles over the system. Cooperation among clinicians is a priority. SOURCE: Table 3-1 in Crossing the Quality Chasm, IOM, 2001

Pay-Off: Health Cost Reduction Potential of 10% with New Care Management Model (Gartner) Necessary for system to move from adverse event model to utilization management model with 10% savings achievable by 2007. Drivers are – – – – Increased costs Patient protection legislation Increased demand for services New technology Using Patient Care Management to Preserve and Enhance Profitability Gartner Inc., September, 2002

Pay-Off: Anticipated Impact of Internet Clinical Applications 20% of Office Visits Eliminated 30% of Physicians Time Reduced PriceWaterhouse Survey of 400 Healthcare Thought Leaders Healthcast 2010

Organizational Context Most organizational decision-making can be classified as occurring at 3 levels: strategic, tactical, and operational (Anthony, 1965) Unstructured Strategic Long-term impact Tactical Structured Operational Short-term impact

Illustrative Examples Biosurveillance – RODS Clinical DSS – Theradoc, Dxplain Administrative DSS – ThinkMed Expert, Internetivity Personalized DSS – Medicalogic, DecisionCoaches

A Conceptual Model of a DSS (Alter) Supporting semi-structured or unstructured decisions Information Data about past and present projections, assumptions People Decision makers, support staff Goals Work Practices Information Technology Interactive systems, software for data analysis, model building, and graphical display

Clinical Decision Framework Patient data Domain info Clinical Decisions Interventions Patient Responses Admin info rts e l A rs e d in Rem Guidelines and Decision Support Pathways Clinical Guidelines and Pathways

DSS Reference Architecture Language System Presentation System Problem Processing System Knowledge System

DXPlain: Diagnostic DSS from Massachusetts General Hospital Uses a set of clinical findings to produce a ranked list of diagnoses that might explain the findings – provides justification – suggests additional clinical information to collect – lists unusual manifestations for each disease

Dxplain Information repository – 2000 diseases – 5000 clinical manifestations – Uses a bayesian probabilistic method to draw inferences about diseases based on presented clinical findings Educational tool for clinical education and clinical problem solving – Electronic medical textbook and a medical reference system

Dxplain info http://www.lcs.mgh.harvard.edu/privlic.htm – to become a registered user – limited to clinicians

Analyzing a DSS Is the goal problem finding or problem solving? What type of activity is involved: planning, execution or control? What approach is used to improve the decision? What kinds of answers does the system provide?

Analyzing a DSS What is the users role and degree of interaction with the system? What kind of impact does the system have on desired objectives? What kind of information technology is used?

Feature of system Extent to which system imposes structure – access to information/tools – enforcement of rules/procedures – substitution of technology for people

Feature of Task Level of coordination – individual/discretionary – individual/mandatory – workgroup – organizational – inter-organizational

Approach used Provide background data – individual discretionary, access to info Support analytic work – individual discretionary, access to tools structure repetitive decisions – individual mandatory, enforcement of rules automate decisions – individual mandatory, substitution of technology for people structure planning processes – organizational, enforcement of rules structure control processes – organizational, enforcement of rules

DSS Reference Architecture Language System Presentation System Problem Processing System Knowledge System

Clinical DSS: Theradoc Antibiotic Assistant

DSS Reference Architecture Language System Presentation System Problem Processing System Knowledge System

DSS and Organizational Decision Making Operational – Theradoc: antibiotic prescription is operational DSS Tactical – Theradoc: provides cost information alongside antibiotic lists for managing infection, thereby resulting in bottom line impact on patient outcomes and costs and revenues Strategic – Antibiotic assistant: prescribes “right” antibiotic, taking costs, demographics, drug interactions and allergies into account Has impact on reducing medical errors, a metric that is compiled and made public See US News and World Report and University ratings – Meets biosurveillance needs and objectives

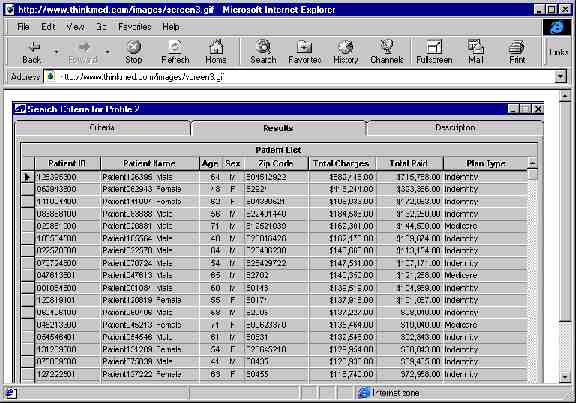
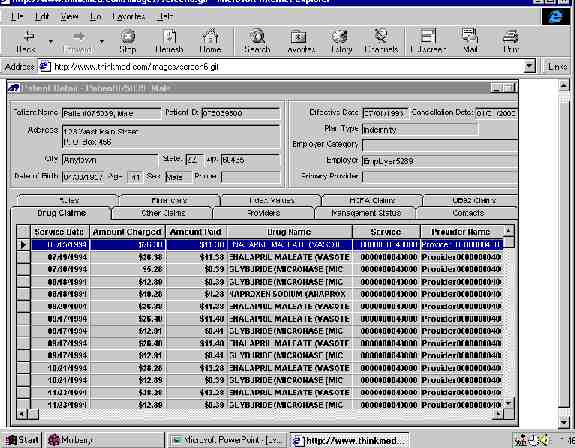
Thinkmed Expert: Data Visualization and Profiling (http://www.click4care.com) http://www.thinkmed.com/soft/ softdemo.htm

ThinkMed Expert Processing of consolidated patient demographic, administrative and claims information using knowledge-based rules Goal is to identify patients at risk in order to intervene and affect financial and clinical outcomes

Vignette High risk diabetes program Need to identify – patients that have severe disease – patients that require individual attention and assessment by case managers Status quo – rely on provider referrals – rely on dollar cutoffs to identify expensive patients

Vignette ThinkMed approach – Interactive query facility with filters to identify patients in the database that have desired attributes patients that are diabetic and that have cardiac, renal, vascular or neurological conditions (use of codes or natural language boolean queries) visualize financial data by charge type

DSS Reference Architecture Language System Presentation System Problem Processing System Knowledge System

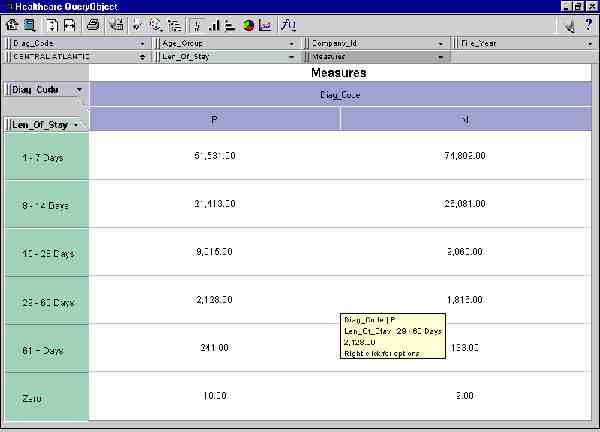
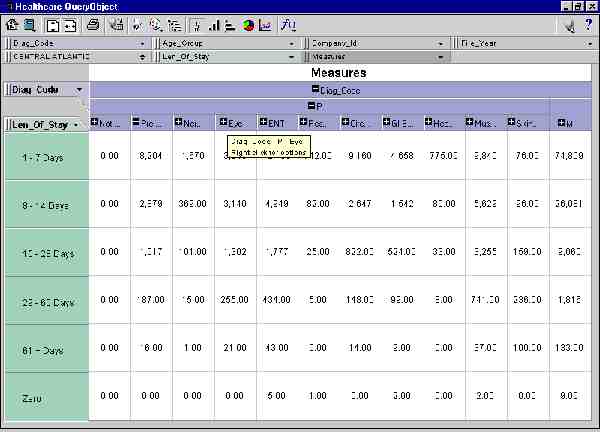
Administrative DSS using WOLAP

DSS Reference Architecture Language System Presentation System Problem Processing System Knowledge System
Personalized DSS for Automating Decisions: Online practice profiling

DSS Reference Architecture Language System Presentation System Problem Processing System Knowledge System

DecisionCoaches (www.decisioncoaches.com)

IT Architecture

DSS Reference Architecture Language System Presentation System Problem Processing System Knowledge System

Case for Change (PriceWaterhouseCoopers 2003) Creating the future hospital system – Focus on high-margin, high-volume, highquality services – Strategically price services – Understand demands on workers – Renew and replace aging physical structures – Provide information at the fingertips – Support physicians through new technologies

Case for Change (PriceWaterhouseCoopers 2003) Creating the future payor system – Pay for performance – Implement self-service tools to lower costs and shift responsibility – Target high-volume users through predictive modeling – Move to single-platform IT and data warehousing systems – Weigh opportunities, dilemmas amid public and private gaps

Challenges Understanding human decision making Understanding the technology environment – status quo (islands of information, legacy systems) – desired status (integrated enterprise-wide view and model of data that can be analyzed and is ubiquitously available)