Clinical Documentation Excellence Program February, 2015
37 Slides852.89 KB
Clinical Documentation Excellence Program February, 2015
Clinical Documentation Team BRIDGING THE GAP Between: The clinical language providers use to describe the patient’s condition And The technical terminology of the ICD-9 system February 2015 2
Provider Scrutiny and Physician Profiling Complete documentation, reflective of the true severity of your patients, helps justify outcomes CMS has rules regarding what wording is acceptable for a condition to be coded Documentation that doesn’t meet the set rules / standards leads to: - Lower severity of illness and risk of mortality assignments - Increased denials - Lower case mix index Physician Profiling - Profiles are used for both commercial and public data sources - Future reimbursement methods will likely incorporate profiles in the formula (e.g. pay for performance) - Hospital Report Cards - Health grades and Leapfrog - Medicare Physician Data (since 2007) - Federal and state regulatory agencies (e.g. OIG) - Quality Improvement Organizations February 2015 3

Why do we Query? Clinical Indicators for diagnosis but no documentation of a condition Clinical evidence for higher degree of specificity or severity A cause and effect relationship between two conditions or organisms An underlying cause when admitted with symptoms Only the documentation of treatment is documented, (without documentation of a diagnosis) Possible present upon admission (POA) indicator status Suspected diagnosis not clearly ruled in or ruled out “close the loop In court, an attorney can’t “lead” a witness into a statement. In hospitals, coders and clinical documentation specialists can’t lead healthcare providers with queries February 2015 4
Documentation must be written licensed provider (MD, DO, NP,PA) Diagnostic documentation must be written by treating provider (We cannot code diagnosis from nurses, nutritionists, therapists, etc.) It is acceptable to co-sign the nutritionist evaluation Nursing documentation of pressure ulcer stage can be coded, but physicians MUST include the site of ulcer and if present on admission (POA) in their progress notes Any abnormal test or lab value must be interpreted and documented in the medical record Pathology results require an associated diagnosis Primary team should confirm diagnoses established by a consultant February 2015 5
Document clear reason for admission Principal diagnosis: The condition established after study to be chiefly responsible for occasioning the admission Secondary diagnosis / Comorbid conditions: Additional conditions that affect patient care in terms of requiring one of the following: - Clinical evaluation - Therapeutic treatment - Diagnostic procedures - Extended length of hospital stay - Increased nursing care and/or monitoring February 2015 6
Diagnostic Documentation – Can be coded All conditions even when clinically obvious must be clearly documented Documentation must be written in Diagnostic Terms for compliance, coding and profiling purposes In the absence of a definitive diagnosis document as: - Possible - Probable - Suspected - Likely If you don’t know what is causing the patient’s symptom or condition, this is important to document as well February 2015 7
Specify Causality Please specify (if known) secondary to due to most likely due to probably due to sepsis due to UTI or any other condition hyperglycemia / uncontrolled DM is due to steroids or other medications cause of pancytopenia most likely due to medications /chemo or other cause cause of AKI most likely due to tubular necrosis or other cause chest pain secondary to CAD or Acute MI, or other cause link diabetes to ulcers, osteomyelitis, neuropathy, PVD, gastroparesis February 2015 8
Acute vs. Chronic Conditions Diagnoses should be documented as: Acute Acute on chronic Chronic Example: Acute renal failure Acute on chronic renal failure Chronic renal failure with stage Acute or chronic osteomyelitis Acute or chronic delirium Acute or chronic DVT-include site February 2015 9
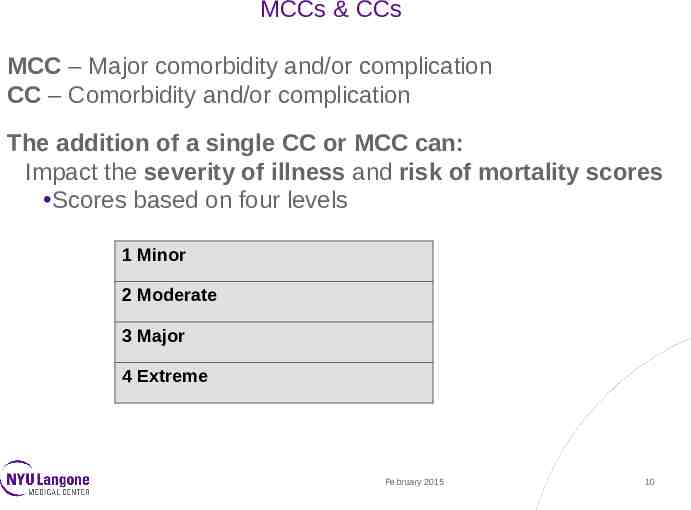
MCCs & CCs MCC – Major comorbidity and/or complication CC – Comorbidity and/or complication The addition of a single CC or MCC can: Impact the severity of illness and risk of mortality scores Scores based on four levels 1 Minor 2 Moderate 3 Major 4 Extreme February 2015 10
Major Complications & Comorbidities Acute and chronic respiratory failure Acute respiratory failure / ARDS Pneumonia Pulmonary embolism Acute renal failure specified etiology: ATN / acute glomerulonephritis End stage renal disease Hepatorenal syndrome Acute systolic & diastolic heart failure Acute pulmonary edema Cardiac arrest / asystole Acute myocardial infarction / necrosis Shock: cardiogenic or septic Sepsis / Severe sepsis Stage 3 and 4 pressure ulcers Mediastinitis Acute/subacute endocarditis Peritonitis Ventricular fibrillation Acute cor pulmonale Toxic and metabolic encephalopathy Severe Protein-calorie malnutrition Pancytopenia due to chemo Acute CVA embolic, hemorrhagic, ischemic Quadriplegia Cerebral infarction Thoracic aneurysm ruptured Diabetic ketoacidosis February 2015 11
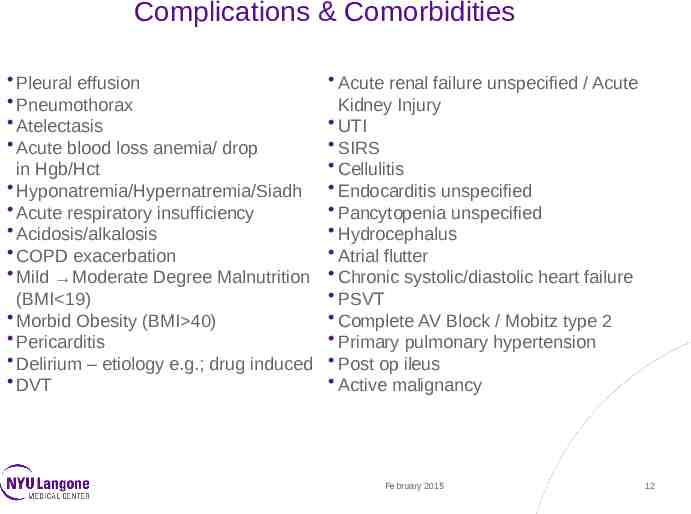
Complications & Comorbidities Pleural effusion Pneumothorax Atelectasis Acute blood loss anemia/ drop in Hgb/Hct Hyponatremia/Hypernatremia/Siadh Acute respiratory insufficiency Acidosis/alkalosis COPD exacerbation Mild Moderate Degree Malnutrition (BMI 19) Morbid Obesity (BMI 40) Pericarditis Delirium – etiology e.g.; drug induced DVT Acute renal failure unspecified / Acute Kidney Injury UTI SIRS Cellulitis Endocarditis unspecified Pancytopenia unspecified Hydrocephalus Atrial flutter Chronic systolic/diastolic heart failure PSVT Complete AV Block / Mobitz type 2 Primary pulmonary hypertension Post op ileus Active malignancy February 2015 12
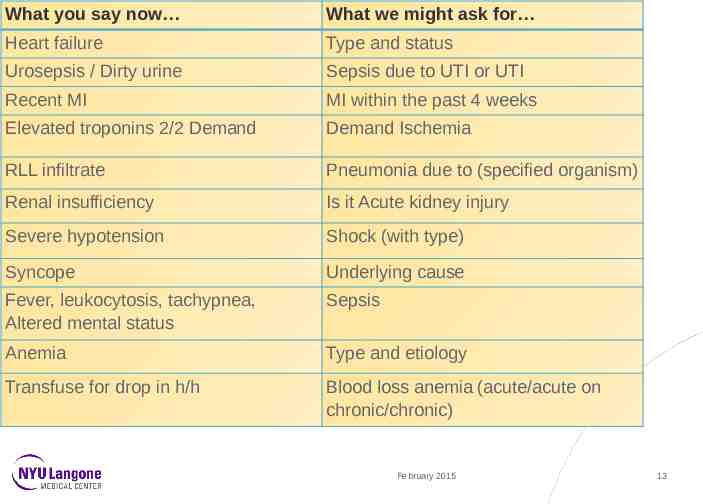
What you say now What we might ask for Heart failure Type and status Urosepsis / Dirty urine Sepsis due to UTI or UTI Recent MI MI within the past 4 weeks Elevated troponins 2/2 Demand Demand Ischemia RLL infiltrate Pneumonia due to (specified organism) Renal insufficiency Is it Acute kidney injury Severe hypotension Shock (with type) Syncope Underlying cause Fever, leukocytosis, tachypnea, Altered mental status Sepsis Anemia Type and etiology Transfuse for drop in h/h Blood loss anemia (acute/acute on chronic/chronic) February 2015 13
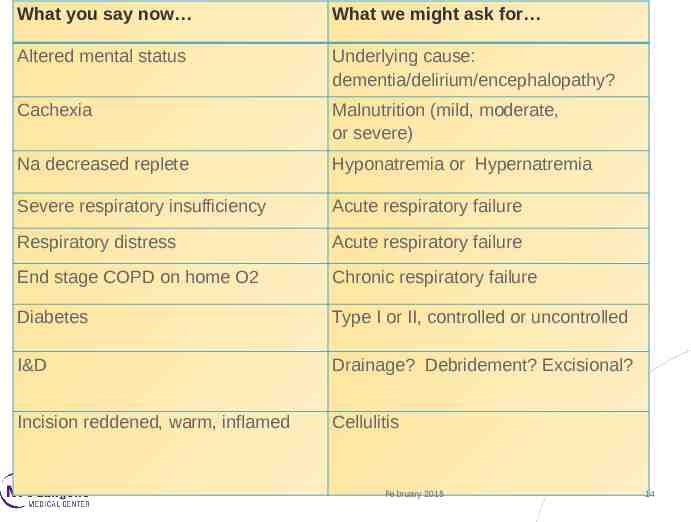
What you say now What we might ask for Altered mental status Underlying cause: dementia/delirium/encephalopathy? Cachexia Malnutrition (mild, moderate, or severe) Na decreased replete Hyponatremia or Hypernatremia Severe respiratory insufficiency Acute respiratory failure Respiratory distress Acute respiratory failure End stage COPD on home O2 Chronic respiratory failure Diabetes Type I or II, controlled or uncontrolled I&D Drainage? Debridement? Excisional? Incision reddened, warm, inflamed Cellulitis February 2015 14
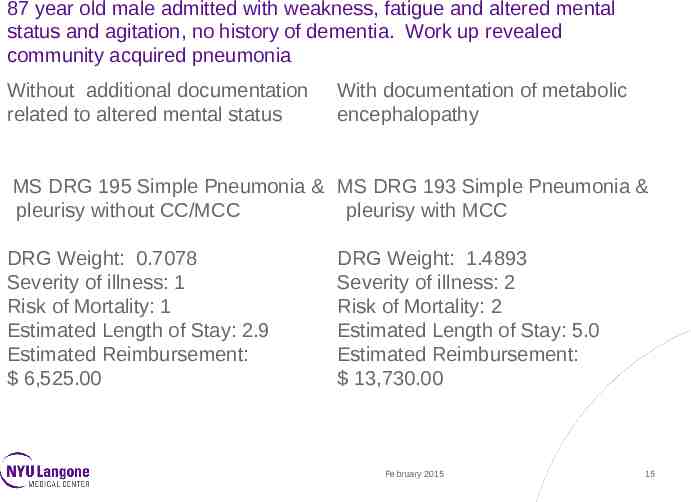
87 year old male admitted with weakness, fatigue and altered mental status and agitation, no history of dementia. Work up revealed community acquired pneumonia Without additional documentation related to altered mental status With documentation of metabolic encephalopathy MS DRG 195 Simple Pneumonia & MS DRG 193 Simple Pneumonia & pleurisy without CC/MCC pleurisy with MCC DRG Weight: 0.7078 Severity of illness: 1 Risk of Mortality: 1 Estimated Length of Stay: 2.9 Estimated Reimbursement: 6,525.00 DRG Weight: 1.4893 Severity of illness: 2 Risk of Mortality: 2 Estimated Length of Stay: 5.0 Estimated Reimbursement: 13,730.00 February 2015 15
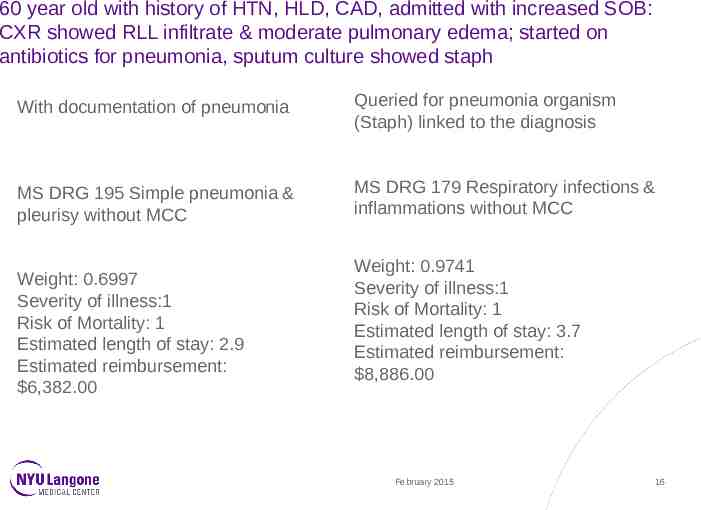
60 year old with history of HTN, HLD, CAD, admitted with increased SOB: CXR showed RLL infiltrate & moderate pulmonary edema; started on antibiotics for pneumonia, sputum culture showed staph With documentation of pneumonia Queried for pneumonia organism (Staph) linked to the diagnosis MS DRG 195 Simple pneumonia & pleurisy without MCC MS DRG 179 Respiratory infections & inflammations without MCC Weight: 0.6997 Severity of illness:1 Risk of Mortality: 1 Estimated length of stay: 2.9 Estimated reimbursement: 6,382.00 Weight: 0.9741 Severity of illness:1 Risk of Mortality: 1 Estimated length of stay: 3.7 Estimated reimbursement: 8,886.00 February 2015 16
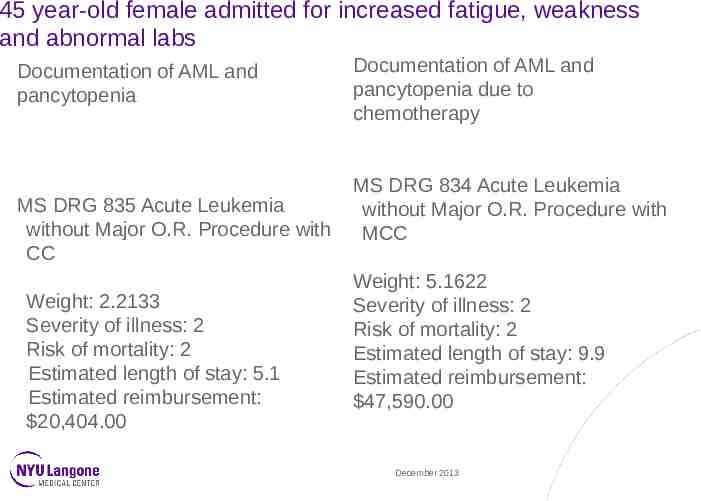
45 year-old female admitted for increased fatigue, weakness and abnormal labs Documentation of AML and pancytopenia MS DRG 835 Acute Leukemia without Major O.R. Procedure with CC Weight: 2.2133 Severity of illness: 2 Risk of mortality: 2 Estimated length of stay: 5.1 Estimated reimbursement: 20,404.00 Documentation of AML and pancytopenia due to chemotherapy MS DRG 834 Acute Leukemia without Major O.R. Procedure with MCC Weight: 5.1622 Severity of illness: 2 Risk of mortality: 2 Estimated length of stay: 9.9 Estimated reimbursement: 47,590.00 December 2013
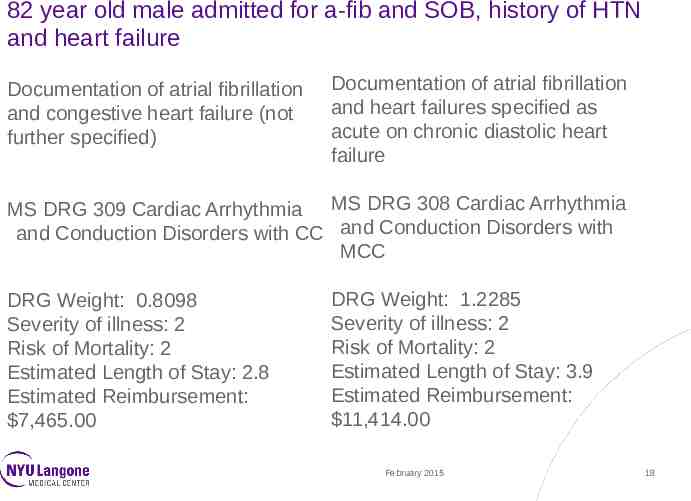
82 year old male admitted for a-fib and SOB, history of HTN and heart failure Documentation of atrial fibrillation and congestive heart failure (not further specified) Documentation of atrial fibrillation and heart failures specified as acute on chronic diastolic heart failure MS DRG 309 Cardiac Arrhythmia MS DRG 308 Cardiac Arrhythmia and Conduction Disorders with CC and Conduction Disorders with MCC DRG Weight: 0.8098 Severity of illness: 2 Risk of Mortality: 2 Estimated Length of Stay: 2.8 Estimated Reimbursement: 7,465.00 DRG Weight: 1.2285 Severity of illness: 2 Risk of Mortality: 2 Estimated Length of Stay: 3.9 Estimated Reimbursement: 11,414.00 February 2015 18
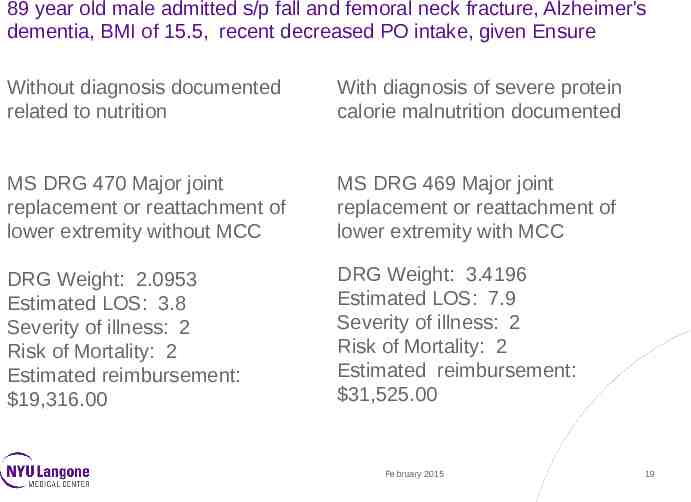
89 year old male admitted s/p fall and femoral neck fracture, Alzheimer's dementia, BMI of 15.5, recent decreased PO intake, given Ensure Without diagnosis documented related to nutrition With diagnosis of severe protein calorie malnutrition documented MS DRG 470 Major joint replacement or reattachment of lower extremity without MCC MS DRG 469 Major joint replacement or reattachment of lower extremity with MCC DRG Weight: 2.0953 Estimated LOS: 3.8 Severity of illness: 2 Risk of Mortality: 2 Estimated reimbursement: 19,316.00 DRG Weight: 3.4196 Estimated LOS: 7.9 Severity of illness: 2 Risk of Mortality: 2 Estimated reimbursement: 31,525.00 February 2015 19
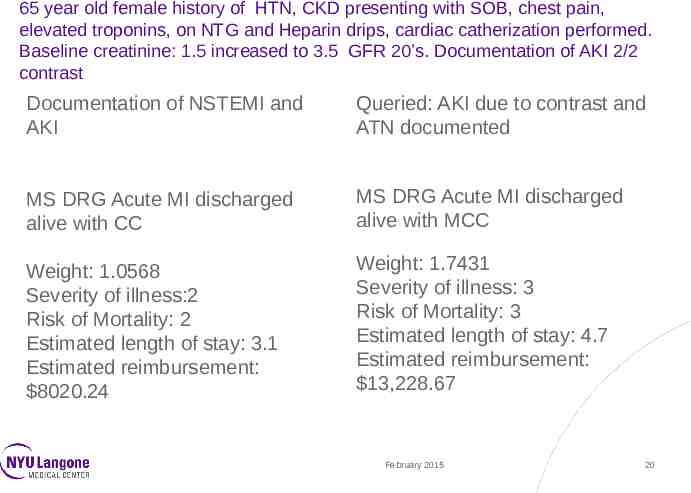
65 year old female history of HTN, CKD presenting with SOB, chest pain, elevated troponins, on NTG and Heparin drips, cardiac catherization performed. Baseline creatinine: 1.5 increased to 3.5 GFR 20’s. Documentation of AKI 2/2 contrast Documentation of NSTEMI and AKI Queried: AKI due to contrast and ATN documented MS DRG Acute MI discharged alive with CC MS DRG Acute MI discharged alive with MCC Weight: 1.0568 Severity of illness:2 Risk of Mortality: 2 Estimated length of stay: 3.1 Estimated reimbursement: 8020.24 Weight: 1.7431 Severity of illness: 3 Risk of Mortality: 3 Estimated length of stay: 4.7 Estimated reimbursement: 13,228.67 February 2015 20
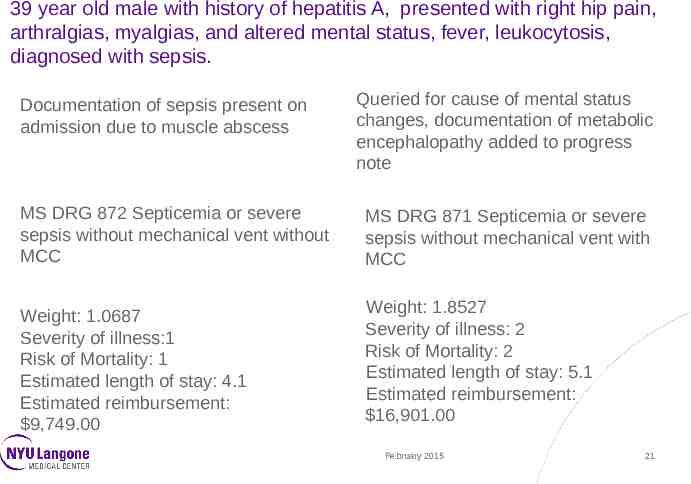
39 year old male with history of hepatitis A, presented with right hip pain, arthralgias, myalgias, and altered mental status, fever, leukocytosis, diagnosed with sepsis. Documentation of sepsis present on admission due to muscle abscess Queried for cause of mental status changes, documentation of metabolic encephalopathy added to progress note MS DRG 872 Septicemia or severe sepsis without mechanical vent without MCC MS DRG 871 Septicemia or severe sepsis without mechanical vent with MCC Weight: 1.0687 Severity of illness:1 Risk of Mortality: 1 Estimated length of stay: 4.1 Estimated reimbursement: 9,749.00 Weight: 1.8527 Severity of illness: 2 Risk of Mortality: 2 Estimated length of stay: 5.1 Estimated reimbursement: 16,901.00 February 2015 21
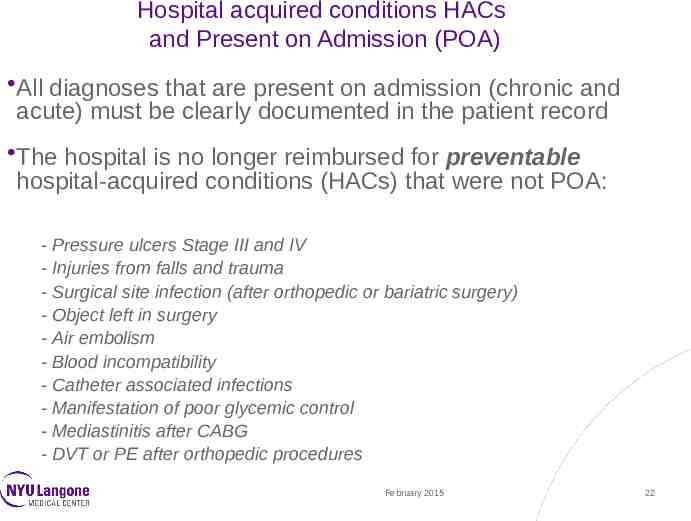
Hospital acquired conditions HACs and Present on Admission (POA) All diagnoses that are present on admission (chronic and acute) must be clearly documented in the patient record The hospital is no longer reimbursed for preventable hospital-acquired conditions (HACs) that were not POA: - Pressure ulcers Stage III and IV - Injuries from falls and trauma - Surgical site infection (after orthopedic or bariatric surgery) - Object left in surgery - Air embolism - Blood incompatibility - Catheter associated infections - Manifestation of poor glycemic control - Mediastinitis after CABG - DVT or PE after orthopedic procedures February 2015 22
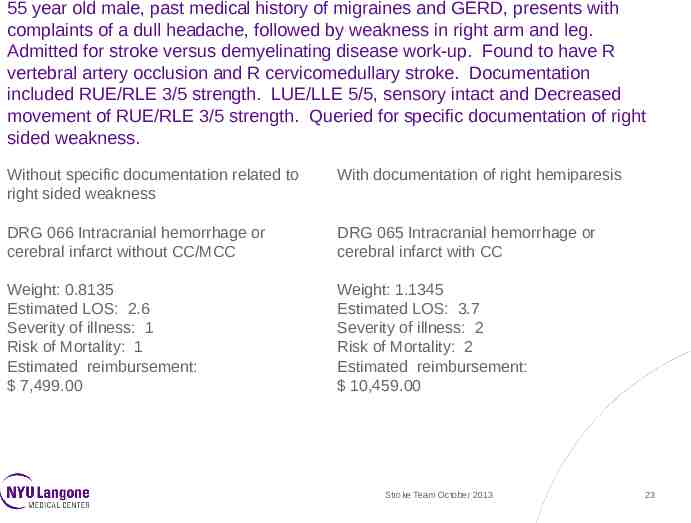
55 year old male, past medical history of migraines and GERD, presents with complaints of a dull headache, followed by weakness in right arm and leg. Admitted for stroke versus demyelinating disease work-up. Found to have R vertebral artery occlusion and R cervicomedullary stroke. Documentation included RUE/RLE 3/5 strength. LUE/LLE 5/5, sensory intact and Decreased movement of RUE/RLE 3/5 strength. Queried for specific documentation of right sided weakness. Without specific documentation related to right sided weakness With documentation of right hemiparesis DRG 066 Intracranial hemorrhage or cerebral infarct without CC/MCC DRG 065 Intracranial hemorrhage or cerebral infarct with CC Weight: 0.8135 Estimated LOS: 2.6 Severity of illness: 1 Risk of Mortality: 1 Estimated reimbursement: 7,499.00 Weight: 1.1345 Estimated LOS: 3.7 Severity of illness: 2 Risk of Mortality: 2 Estimated reimbursement: 10,459.00 Stroke Team October 2013 23
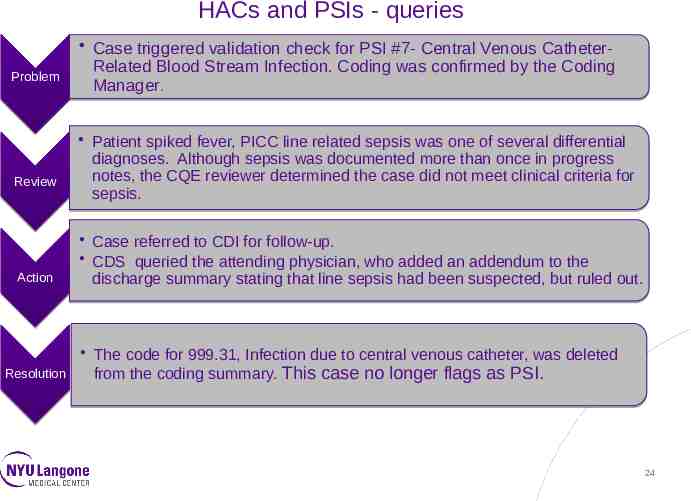
HACs and PSIs - queries Problem Review Action Case triggered validation check for PSI #7- Central Venous CatheterRelated Blood Stream Infection. Coding was confirmed by the Coding Manager. Patient spiked fever, PICC line related sepsis was one of several differential diagnoses. Although sepsis was documented more than once in progress notes, the CQE reviewer determined the case did not meet clinical criteria for sepsis. Case referred to CDI for follow-up. CDS queried the attending physician, who added an addendum to the discharge summary stating that line sepsis had been suspected, but ruled out. The code for 999.31, Infection due to central venous catheter, was deleted from the coding summary. This case no longer flags as PSI. Resolution 24
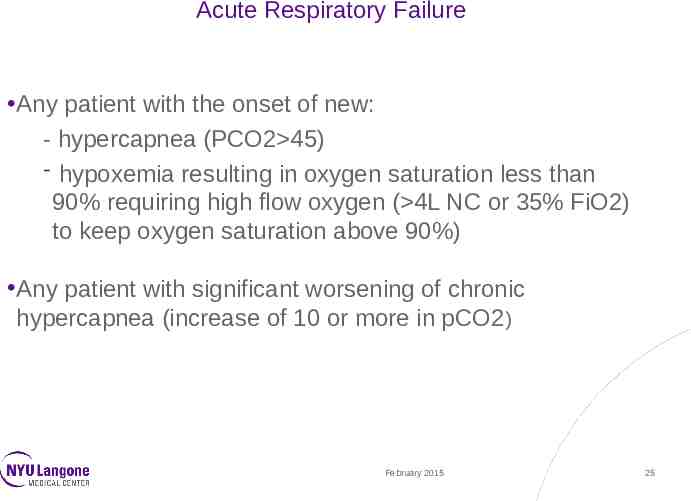
Acute Respiratory Failure Any patient with the onset of new: - hypercapnea (PCO2 45) - hypoxemia resulting in oxygen saturation less than 90% requiring high flow oxygen ( 4L NC or 35% FiO2) to keep oxygen saturation above 90%) Any patient with significant worsening of chronic hypercapnea (increase of 10 or more in pCO2) February 2015 25
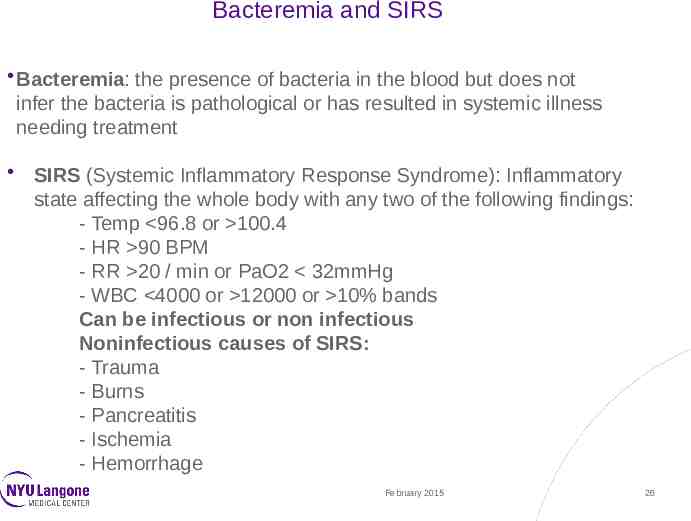
Bacteremia and SIRS Bacteremia: the presence of bacteria in the blood but does not infer the bacteria is pathological or has resulted in systemic illness needing treatment SIRS (Systemic Inflammatory Response Syndrome): Inflammatory state affecting the whole body with any two of the following findings: - Temp 96.8 or 100.4 - HR 90 BPM - RR 20 / min or PaO2 32mmHg - WBC 4000 or 12000 or 10% bands Can be infectious or non infectious Noninfectious causes of SIRS: - Trauma - Burns - Pancreatitis - Ischemia - Hemorrhage February 2015 26
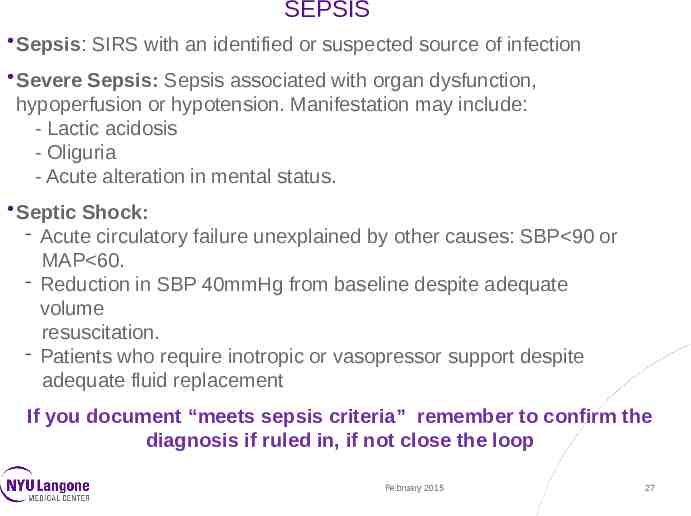
SEPSIS Sepsis: SIRS with an identified or suspected source of infection Severe Sepsis: Sepsis associated with organ dysfunction, hypoperfusion or hypotension. Manifestation may include: - Lactic acidosis - Oliguria - Acute alteration in mental status. Septic Shock: - Acute circulatory failure unexplained by other causes: SBP 90 or MAP 60. - Reduction in SBP 40mmHg from baseline despite adequate volume resuscitation. - Patients who require inotropic or vasopressor support despite adequate fluid replacement If you document “meets sepsis criteria” remember to confirm the diagnosis if ruled in, if not close the loop February 2015 27
Heart Failure All heart failure diagnoses if known must be specified as: Acute Systolic and /or Diastolic heart failure Chronic Systolic and/or Diastolic heart failure Acute on Chronic Systolic and/or Diastolic heart failure Commonly documented indicators for acute episode: Elevated BNP/Troponin CXR : pleural effusion, pulmonary congestion/edema SOB/DOE Presence of edema Administration of diuretics Echo: systolic, diastolic dysfunction, and low EF February 2015 28
Chronic Kidney Disease Stage I: normal GFR (reported as eGFR 60 cc/min) with either structural renal disease (e.g. polycystic kidney disease, one kidney) or proteinuria III Moderate decrease in GFR 30-59 IV Severe decrease in GFR 15-29 V Kidney failure 15 (or dialysis) February 2015 29
Acute Kidney Injury/ Acute Renal Failure Criteria for diagnosis: If Baseline creatinine 2.0 mg/dl rise in creatinine of 0.3 mg/dl or more If Baseline creatinine 2.0 mg/dl-4.9 mg/dl rise in creatinine 1.0 mg/dl or more If Baseline creatinine 4.9 mg/dl rise in creatinine of 1.5 mg/dl or more Urine output of 600 cc/24h Any form of renal replacement therapy (Hemodialysis or continuous renal replacement therapy) February 2015 30
Malnutrition Document physical findings and link to specific diagnosis New criteria was developed by NYU Nutrition Department (handout) Consider: Decreased intake % weight loss Time frame over which weight was lost Muscle mass Grip strength Temporal wasting Note: serum proteins (albumin and pre-albumin) are not included in the diagnostic criteria for malnutrition as recent evidence shows that these acute phase proteins do not change in response to nutrient intake February 2015 31
Functional Quadriplegia Complete inability to move due to a severe disability or frailty caused by another medical condition without physician injury or damage to the brain or spinal cord Patients usually do not have the mental ability to move themselves and require “total care” Common causes/ Advanced neurological degeneration from: Dementia / Alzheimer’s disease Hypoxic injury ALS Huntington’s disease MS February 2015 32
Documentation requirements for DVT Acute or Chronic Specify vein: if unspecified vein of leg, specify distal or proximal leg Specify laterality: e.g. Right, Left, bilateral Specify if patient is on anticoagulants for chronic DVT or prevention If no longer present, and patient is on anticoagulation to prevent recurrence- document “no longer present” rather than “ history of” Specify if present upon admission ( POA) or not February 2015 33
.DX PHRASES .dxAcuteKidneyFailure .dxHeartFailure .dxAcuteRespiratoryFailure .dxHypertension .dxArrhythmia .dxMyocardialInfarction .dxbmiwt .dxPelvicInflammatoryDisease .dxBurn .dxPhlebitis .dxChronicKidneyDisease .dxRheumatoidArthiritis .dxCOPD .dxStroke .dxDementia .dxTransportInjury .dxDiabetes .dxVaricoseVeins .dxEntericUlcer .dxVaricoseVeins .dxHeadache .dxWithdrawal .dxHeartDisease February 2015 34
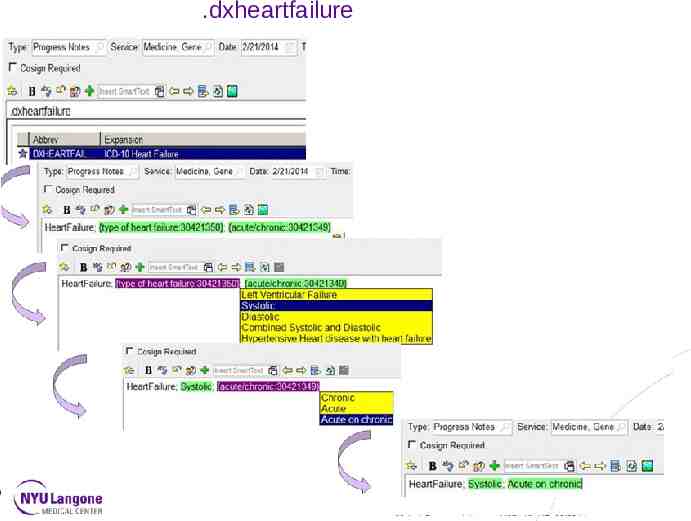
.dxheartfailure February 2015 35

.dxstroke Hospitalist April 2014
THANK YOU! Questions? This presentation was created by the NYU Langone Medical Center HIM Department. It should not be copied or distributed without permission. February 2015 37