By: Darryl Jamison Macon County EMS Training Coordinator
27 Slides1,017.50 KB
By: Darryl Jamison Macon County EMS Training Coordinator
Describe fetal-maternal blood flow and the role of the placenta. Identify the details of the history that should be obtained from an obstetrical patient. Discuss the effects of pregnancy on pre-existing conditions such as diabetes, HTN, and cardiac problems. Define the following terms: – Spontaneous abortion; criminal abortion; therapeutic abortion
Describe the pathophysiology and management of the following conditions: – Ectopic pregnancy – Abruptio placenta – Placenta previa
Objectives cont. Distinguish between pregnancy-induced hypertension, preeclampsia, eclampsia. Describe management of prolapsed cord. Describe management of breech presentation Describe management of multiple-birth presentation Describe the pathophysiology and management of the following conditions: – Postpartum hemorrhage – Uterine inversion – Uterine rupture
Fetal-Maternal Blood flow Blood flows from the placenta in through the umbilical vein which connects to the inferior vena cava then to the heart Routed around the lungs through the ductus arteriosus, into the aorta and then throughout the baby. Deoxygenated blood is filtered by the liver and then transported to the mother
Role of the placenta Provides for exchange of respiratory gases. Transport of the nutrients Excretion of wastes Transfer of heat The placenta becomes an active endocrine gland, producing several important hormones
History Should include: – Gravidity—number of pregnancies – Para—number of viable fetus delivered – Length of gestation – Estimated date of confinement – Previous complications with pregnancies – When did pain start – Sudden or slow in onset – Duration, location, radiation – Is it regular – Spotting – Proper prenatal care – If active labor, question push or bowel movement
Diabetes – Patients have to be placed on insulin— medication will pass to the fetus – Effects on baby—tend to be larger in size – Tend to have trouble maintaining body temp. And subject to hypoglycemia
Hypertension Generally speaking bp is lower in pregnancy than non-pregnancy Preexisting hypertension is exacerbated Persistent HTN adversely affects placental size Leading to compromise of fetus and placing mother at risk for CVA or renal failure
Cardiac During pregnancy, cardiac output increases up to 30% Can lead to CHF from preexisting
Spontaneous Abortion Commonly called a miscarriage Occurs of its own accord Occur before the 12th week of pregnancy Many occur within 2 weeks after conception, being mistaken for menstrual cycle
Criminal Abortion Attempt to destroy fetus by one whom is not licensed to do so Amateurs Without aseptic techniques Leads to other complications
Therapeutic Abortion The pregnancy posed a threat to maternal well-being Judged to medically indicated
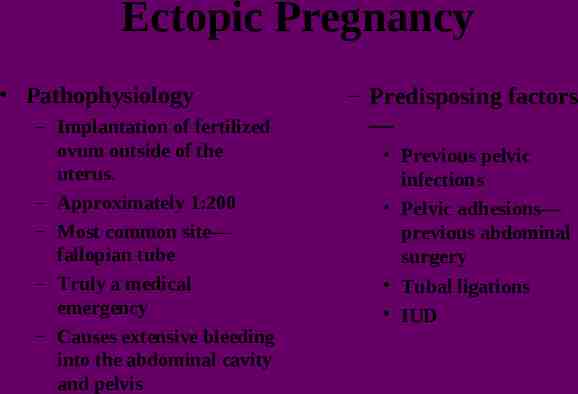
Ectopic Pregnancy Pathophysiology – Implantation of fertilized ovum outside of the uterus. – Approximately 1:200 – Most common site— fallopian tube – Truly a medical emergency – Causes extensive bleeding into the abdominal cavity and pelvis – Predisposing factors — Previous pelvic infections Pelvic adhesions— previous abdominal surgery Tubal ligations IUD
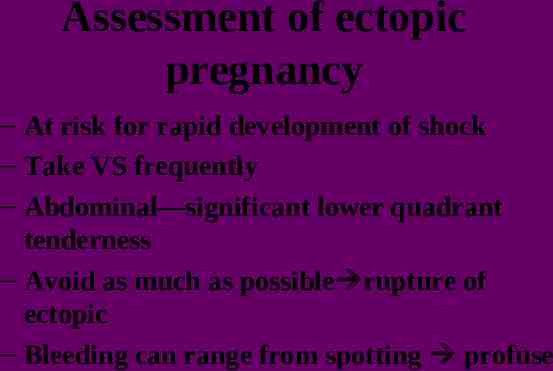
Assessment of ectopic pregnancy – At risk for rapid development of shock – Take VS frequently – Abdominal—significant lower quadrant tenderness – Avoid as much as possible rupture of ectopic – Bleeding can range from spotting profuse
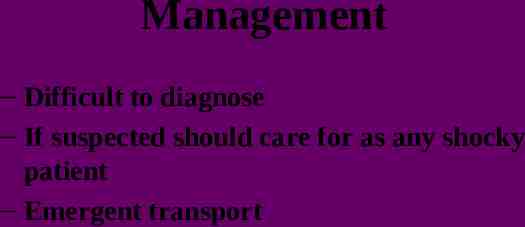
Management – Difficult to diagnose – If suspected should care for as any shocky patient – Emergent transport
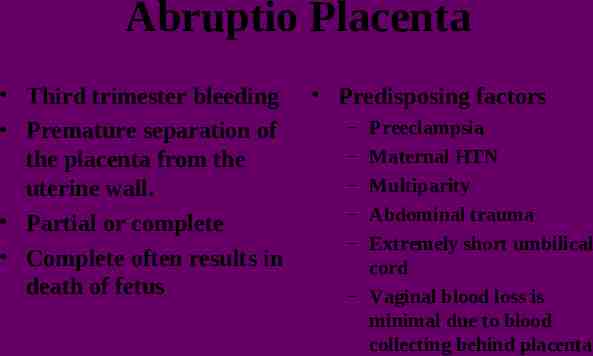
Abruptio Placenta Third trimester bleeding Premature separation of the placenta from the uterine wall. Partial or complete Complete often results in death of fetus Predisposing factors – – – – – Preeclampsia Maternal HTN Multiparity Abdominal trauma Extremely short umbilical cord – Vaginal blood loss is minimal due to blood collecting behind placenta
Assessment – – – – – Have constant, severe abdominal pain Feels like something is “tearing” Abdomen is very tender Bleeding will be dark in color PMH—abruptio placenta
Management COMI Large bore IV’s Rapid transport
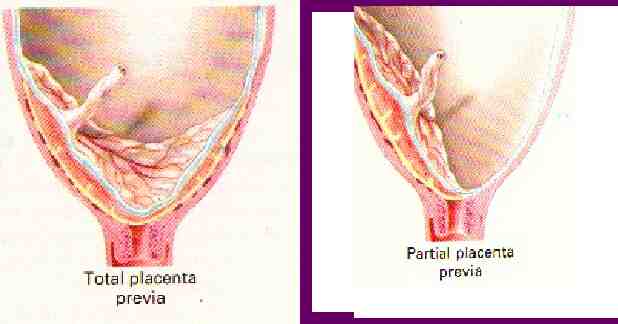
Placenta Previa – Attachment of the placenta that partially or completely covers the internal cervix – Begins to bleed as the cervix thins out, spreading the placenta until it tears – Precipitated by sexual intercourse or digital vaginal examination
Assessment – Usually multigravida – Third trimester – Most common— painless, bright red bleeding – Uterus is soft – Management— COMI High flow O2 Large bore IV’s Rapid transport
PIH Bp of 140/90 Early stage of disease process Bp is normally low so 130/80 maybe high

Preeclampsia Characterized by: – – – – – – – HTN Abnormal weight gain Edema Headache Protein in urine Epigastric pain Visual disturbances
Eclampsia Characterized by the same as pre but includes seizures
Supine Hypotensive Syndrome Occurs in the third trimester Marked decrease in blood flow to the heart due to increase mass in abdominal cavity Compresses on the inferior vena cava thus decreasing the blood flow back to the heart Assessment—be aware of signs of shock and verify previous problems with same Management—place in LLR, treat for shock if other signs of shock are present.