WINTER PARK FIRE DEPARTMENT Medical Director’s Meeting AUGUST
50 Slides6.74 MB

WINTER PARK FIRE DEPARTMENT Medical Director’s Meeting AUGUST – SEPTEMBER 2021
Disclosures TeamHealth medical director/physician Winter Park FD medical director City College medical director Care-A-Medix medical director Jacob Medical Advisors ceo MDM Capital Ventures ceo Nova Southeastern University associate clinical professor
This presentation is a Patient Safety Work Product Keep It Confidential!
“ Better prehospital care Better hospital outcomes ” Mission Statement
II CHEST PAIN / CARDIOLOGY I CHEST PAIN/DYSPNEA GENERAL APPROACH TO THE PATIENT II ACUTE CORONARY SYNDROMES SUDDEN CARDIAC DEATH ACUTE PULMONARY EDEMA III ARRYTHMIAS
TIPS FOR ASCULTATION Listen to every patient Bare skin Proper orientation of the earpieces A decent stethoscope helps
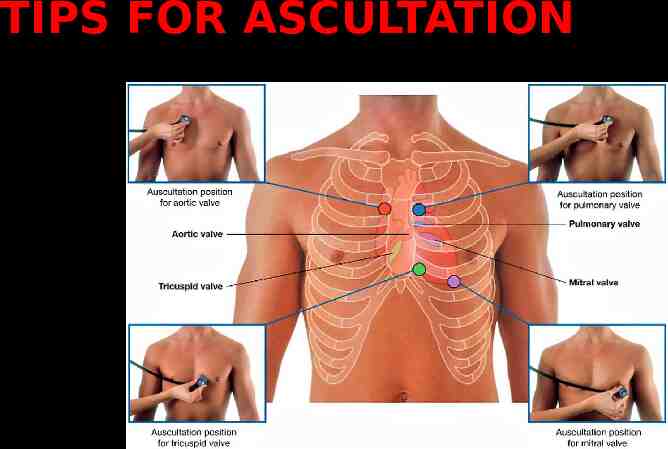
TIPS FOR ASCULTATION
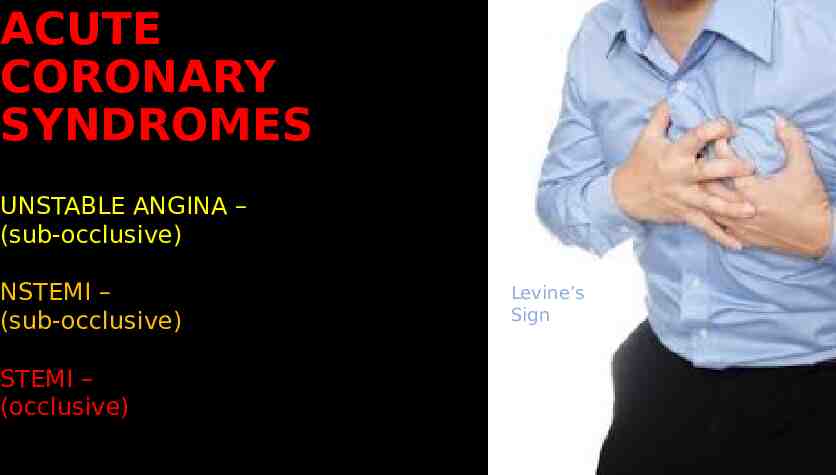
ACUTE CORONARY SYNDROMES UNSTABLE ANGINA – (sub-occlusive) NSTEMI – (sub-occlusive) STEMI – (occlusive) Levine’s Sign
ACUTE CORONARY SYNDROMES Epidemiology Cardiovascular disease is the leading cause of death in the USA Cardiac Arrest Biggest gains in survival come from bystander CPR/AED use If initial EMS rhythm is asystole, meaningful survival is essentially nil Dispatch directives are key to survival Signs and Symptoms Site, nature, nausea and diaphoresis DO NOT accurately predict AMI/ACS
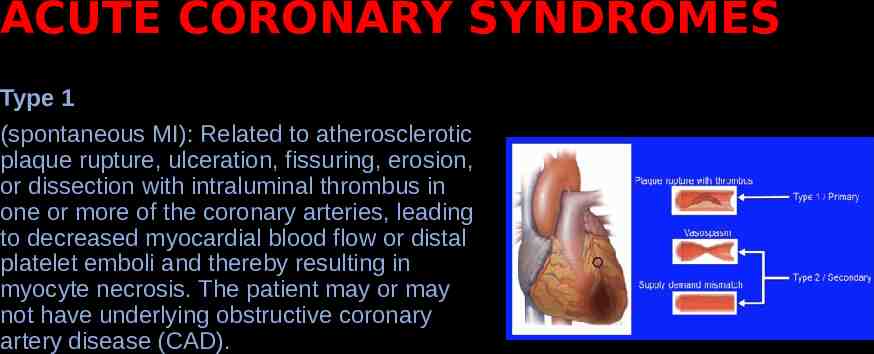
ACUTE CORONARY SYNDROMES Type 1 (spontaneous MI): Related to atherosclerotic plaque rupture, ulceration, fissuring, erosion, or dissection with intraluminal thrombus in one or more of the coronary arteries, leading to decreased myocardial blood flow or distal platelet emboli and thereby resulting in myocyte necrosis. The patient may or may not have underlying obstructive coronary artery disease (CAD).
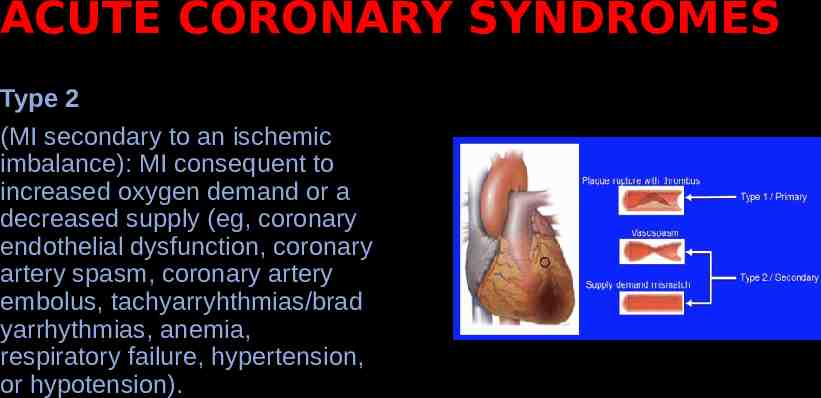
ACUTE CORONARY SYNDROMES Type 2 (MI secondary to an ischemic imbalance): MI consequent to increased oxygen demand or a decreased supply (eg, coronary endothelial dysfunction, coronary artery spasm, coronary artery embolus, tachyarryhthmias/brad yarrhythmias, anemia, respiratory failure, hypertension, or hypotension).
ACUTE CORONARY SYNDROMES Type 3 (MI resulting in death when biomarker values are unavailable): Sudden, unexpected cardiac death before blood samples for biomarkers could be drawn or before their appearance in the circulation.
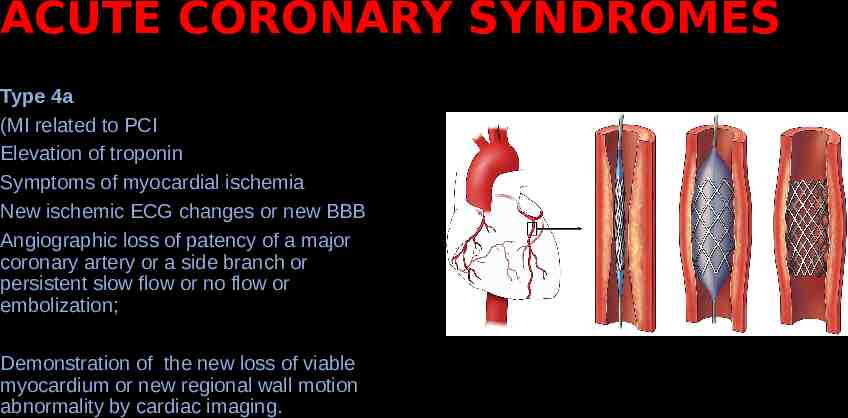
ACUTE CORONARY SYNDROMES Type 4a (MI related to PCI Elevation of troponin Symptoms of myocardial ischemia New ischemic ECG changes or new BBB Angiographic loss of patency of a major coronary artery or a side branch or persistent slow flow or no flow or embolization; Demonstration of the new loss of viable myocardium or new regional wall motion abnormality by cardiac imaging.
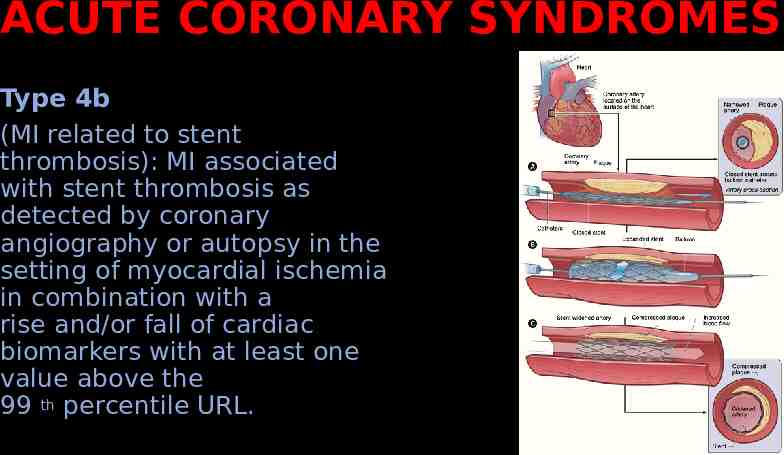
ACUTE CORONARY SYNDROMES Type 4b (MI related to stent thrombosis): MI associated with stent thrombosis as detected by coronary angiography or autopsy in the setting of myocardial ischemia in combination with a rise and/or fall of cardiac biomarkers with at least one value above the 99 th percentile URL.
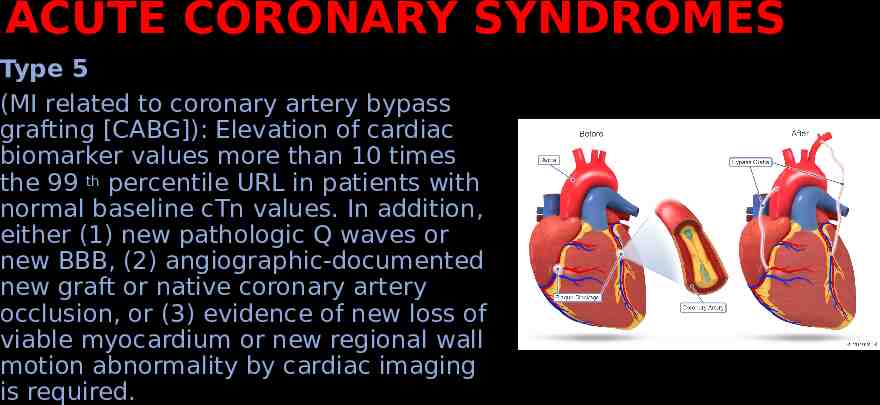
ACUTE CORONARY SYNDROMES Type 5 (MI related to coronary artery bypass grafting [CABG]): Elevation of cardiac biomarker values more than 10 times the 99 th percentile URL in patients with normal baseline cTn values. In addition, either (1) new pathologic Q waves or new BBB, (2) angiographic-documented new graft or native coronary artery occlusion, or (3) evidence of new loss of viable myocardium or new regional wall motion abnormality by cardiac imaging is required.
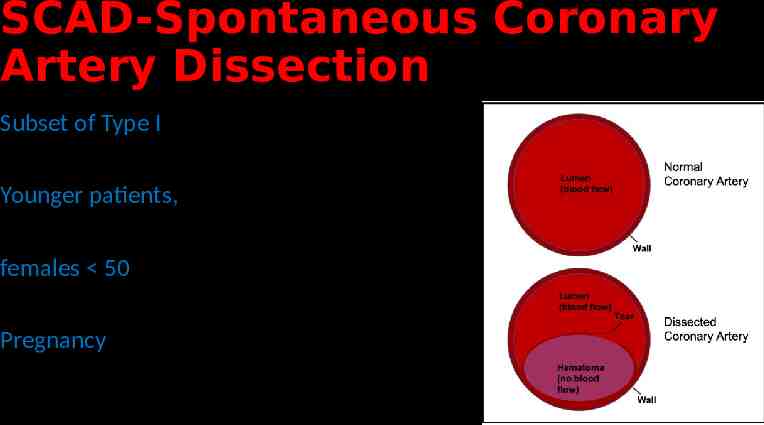
SCAD-Spontaneous Coronary Artery Dissection Subset of Type I Younger patients, females 50 Pregnancy
ACUTE CORONARY SYNDROMES Management Transport Decision to STEMI center- first contact to balloon 90 minutes Aspirin – give asap- (only contraindication is anaphylaxis, active GI bleed) Oxygen - oxygen saturation 90% Nitroglycerin –ask about ED drugs Morphine Pads Placed – (6% risk VT VF)
ACUTE CORONARY SYNDROMES Nitrogylcerin use Contraindications Black Box warning! Ask if the patient is taking erectile dysfunction medications before giving nitroglycerin For sublingual Nitroglycerin- if they take Viagra (sildenafil) or Levitra (vardenafil), it must be 24 hours before you can give SL nitroglycerin. If they take Cialis (tadafil) it must be 48 hours before you can give SL nitroglycerin. For IV Nitroglycerin- it is a relative contraindication if they have taken a PDE-5 medication the last 48 hours. The provider must weight the risk- benefit based on the patient’s condition. Inferior Wall MI – Nitroglycerin is a low-risk intervention
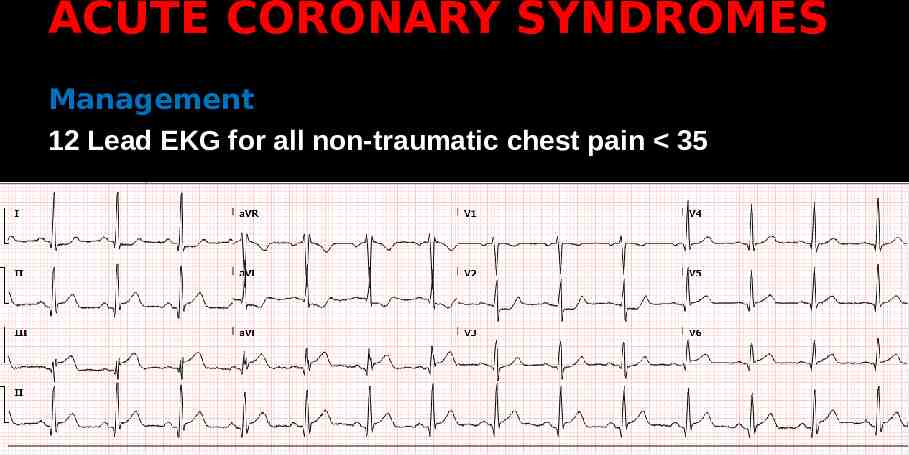
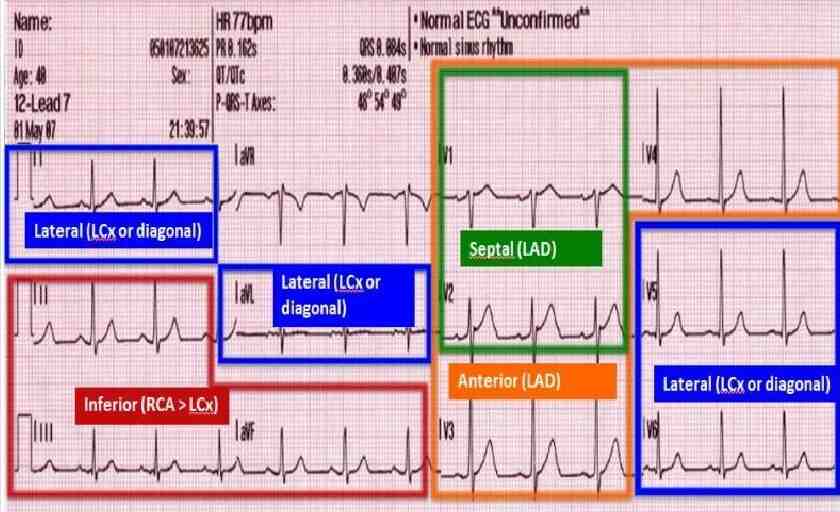
ACUTE CORONARY SYNDROMES Management 12 Lead EKG for all non-traumatic chest pain 35
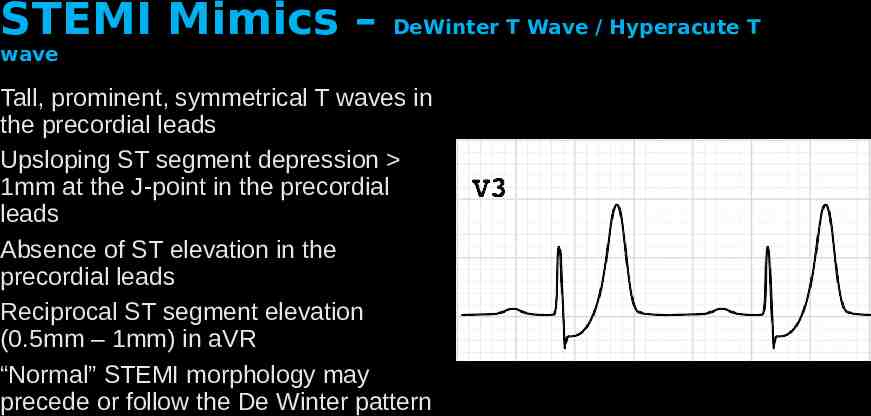
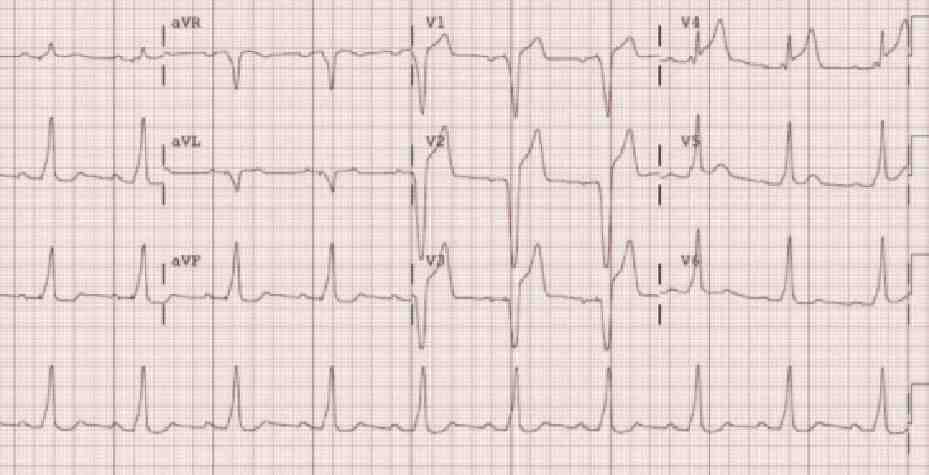
STEMI Mimics – DeWinter T Wave / Hyperacute T wave Tall, prominent, symmetrical T waves in the precordial leads Upsloping ST segment depression 1mm at the J-point in the precordial leads Absence of ST elevation in the precordial leads Reciprocal ST segment elevation (0.5mm – 1mm) in aVR “Normal” STEMI morphology may precede or follow the De Winter pattern
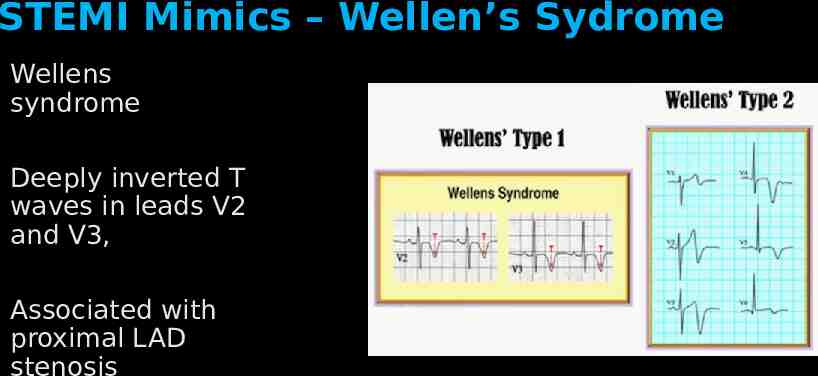
STEMI Mimics – Wellen’s Sydrome Wellens syndrome Deeply inverted T waves in leads V2 and V3, Associated with proximal LAD stenosis
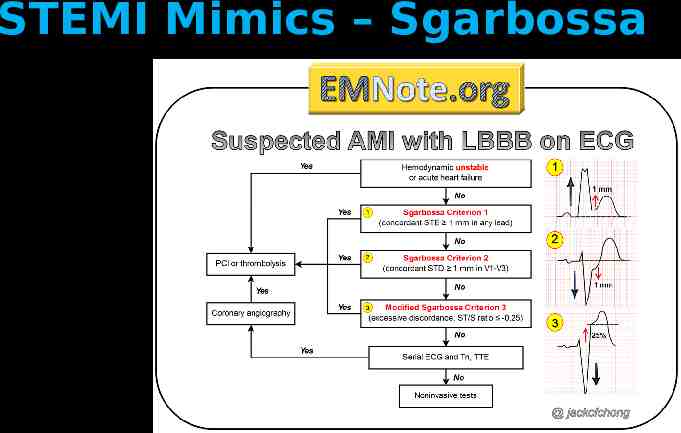
STEMI Mimics – Sgarbossa Elena Sgarbossa, MD Described in 1996 Criteria for diagnosing A myocardial infarction with the presence of a left bundle branch block
STEMI Mimics – Sgarbossa
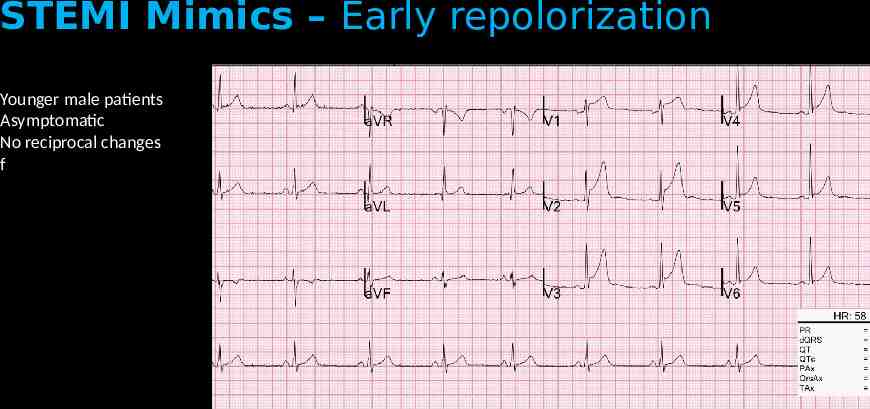
STEMI Mimics – Early repolorization Younger male patients Asymptomatic No reciprocal changes f
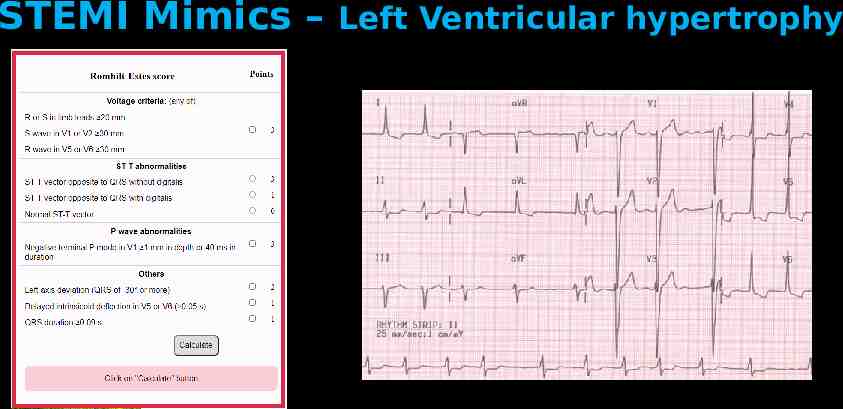
STEMI Mimics – Left Ventricular hypertrophy
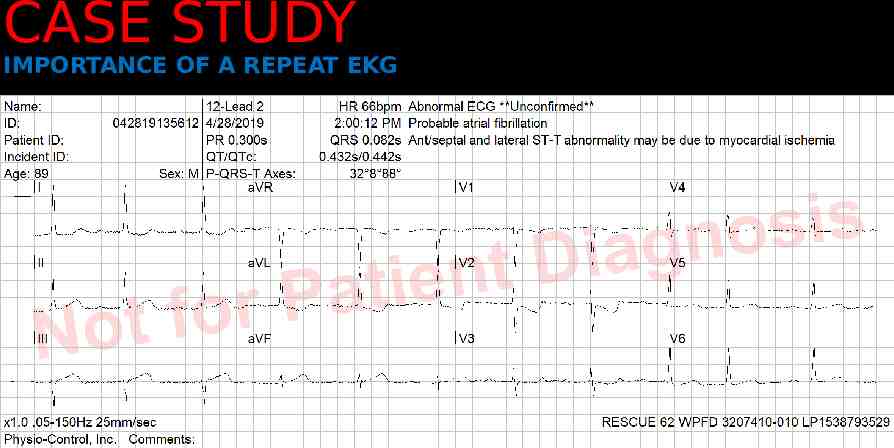
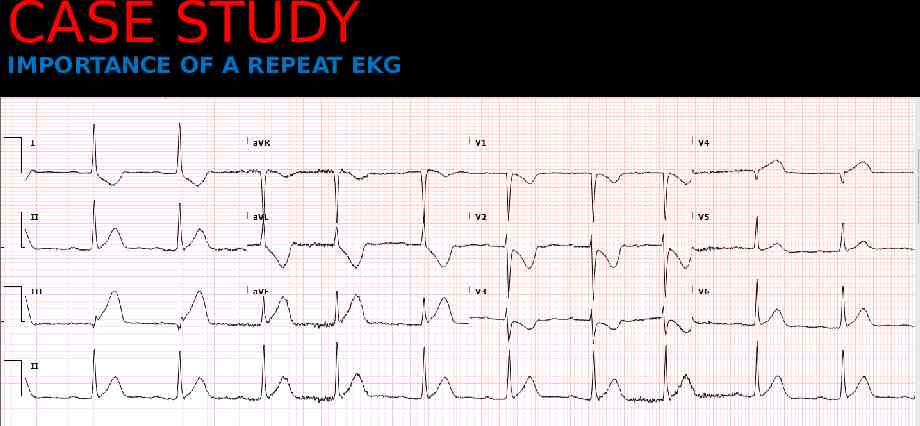
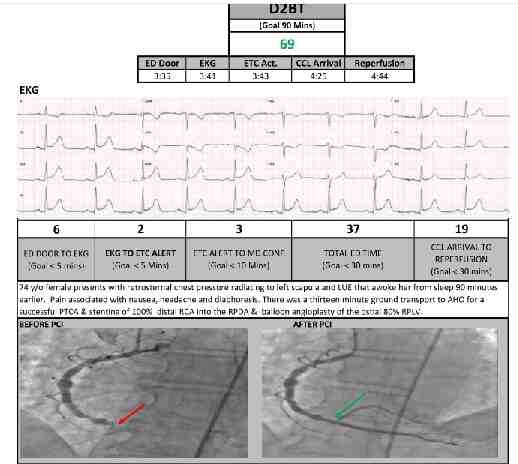
CASE STUDY IMPORTANCE OF A REPEAT EKG
CASE STUDY IMPORTANCE OF A REPEAT EKG
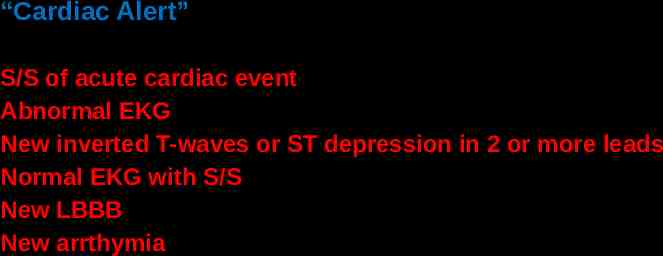
“Cardiac Alert” S/S of acute cardiac event Abnormal EKG New inverted T-waves or ST depression in 2 or more leads Normal EKG with S/S New LBBB New arrthymia
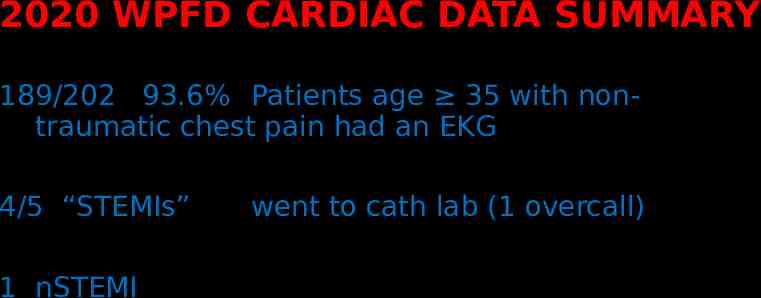
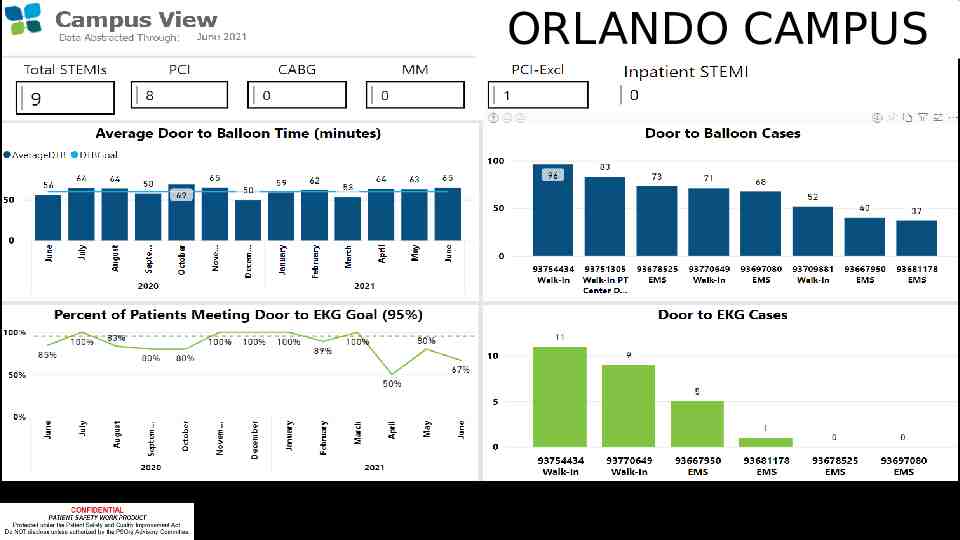
WPFD CARDIAC DATA 2020
2020 WPFD CARDIAC DATA SUMMARY 189/202 93.6% Patients age 35 with nontraumatic chest pain had an EKG 4/5 “STEMIs” 1 nSTEMI went to cath lab (1 overcall)
ORLANDO CAMPUS
SUDDEN CARDIAC DEATH

SUDDEN CARDIAC DEATH Cardiovascular Collapse Loss of effective perfusion (benign or catastrophic) Cardiovacular Arrest Abrupt cessation of cardiac mechanical function Sudden Cardiac Death Irreversible cessation of biological functions
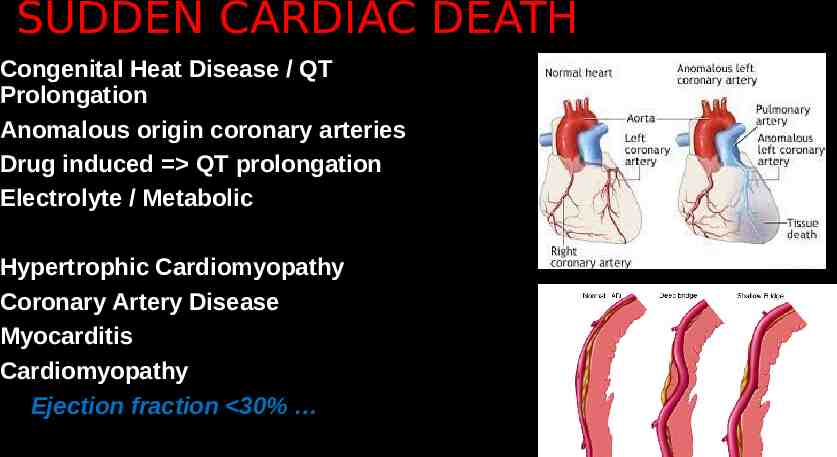
SUDDEN CARDIAC DEATH Congenital Heat Disease / QT Prolongation Anomalous origin coronary arteries Drug induced QT prolongation Electrolyte / Metabolic Hypertrophic Cardiomyopathy Coronary Artery Disease Myocarditis Cardiomyopathy Ejection fraction 30%
UTSTEIN STYLE A set of guidelines for uniform reporting of cardiac arrest. First proposed for emergency medical services in 1991. Examples of cardiac arrest registries based on the Utstein Style include the Cardiac Arrest Registry to Enhance Survival,
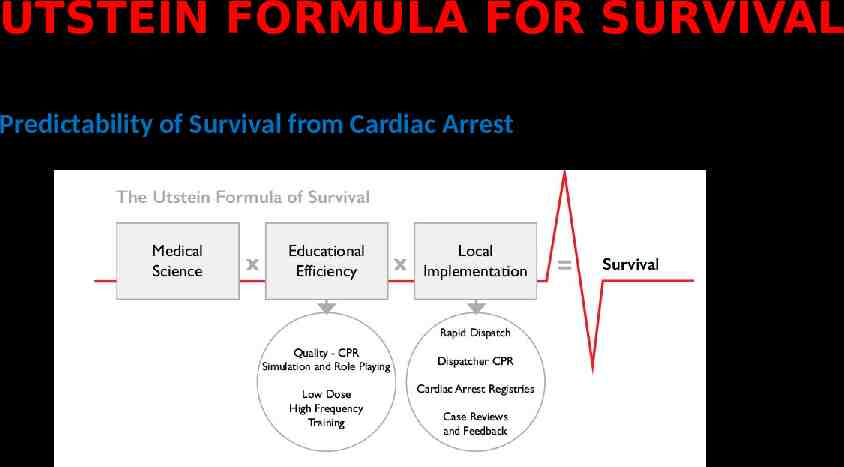
UTSTEIN FORMULA FOR SURVIVAL Predictability of Survival from Cardiac Arrest
Congestive Heart Failure (CHF) Epidemiology Leading cause of admission for age 65 Signs and Symptoms Dyspnea Volume overload / edema Hypertension (frequently, not always) JVD Fatigue Dyspnea on exertion Orthopnea
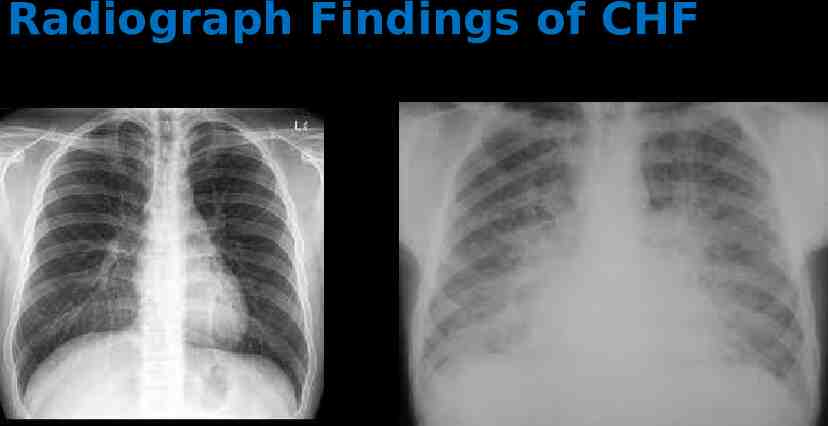
Radiograph Findings of CHF
Congestive Heart Failure (CHF) Cardiac Dysfunction (A change in structure or function) Hypertension Arrythmia (atrial fibrillation) Ischemic / Myocardial Infarction Cardiomyopathy ((ischemic, post viral, chemotherapy ) Myocarditis Valvular Takotsubo’s Backward Failure pulmonary edema Forward Failure renal insufficiency, fatigue
Critical Care Command & Control Survival for patients with an initially shockable rhythm decreases 10% for every minute delay in defibrillation. Dispatcher directed, “hands-only” bystander CPR can approximately double survival. 79% of initial documented cardiac arrest rhythms are shockable when an AED is applied by a bystander, but only 35% of initial rhythms are shockable when no AED is applied and the first cardiac arrest rhythm is recorded after EMS arrives and applies a monitor/defibrillator. Bystander-delivered shocks using an AED before EMS arrival triple survival (34 vs.12%)
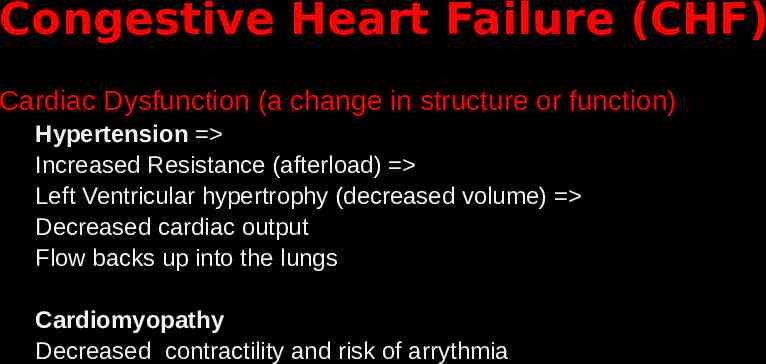
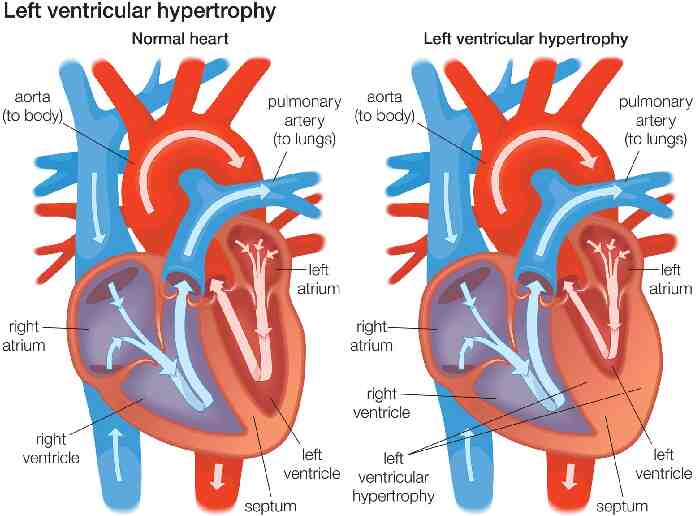
Congestive Heart Failure (CHF) Cardiac Dysfunction (a change in structure or function) Hypertension Increased Resistance (afterload) Left Ventricular hypertrophy (decreased volume) Decreased cardiac output Flow backs up into the lungs Cardiomyopathy Decreased contractility and risk of arrythmia
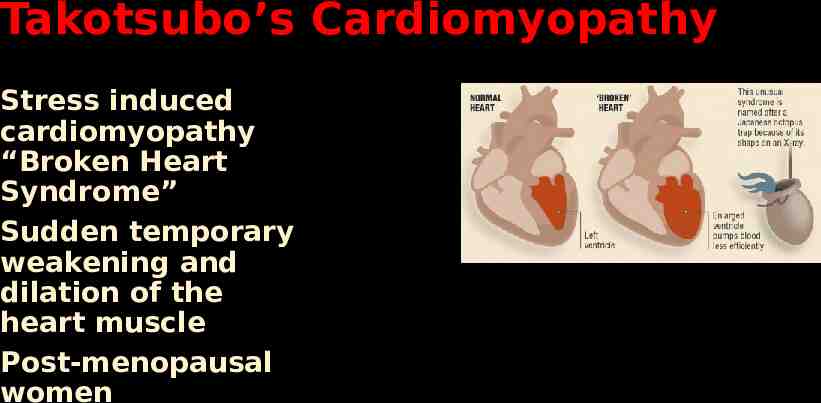
Takotsubo’s Cardiomyopathy Stress induced cardiomyopathy “Broken Heart Syndrome” Sudden temporary weakening and dilation of the heart muscle Post-menopausal women
Congestive Heart Failure (CHF) Management Oxygen Positioning Nitroglycerin Lasix Bipap Morphine? (out of favor )
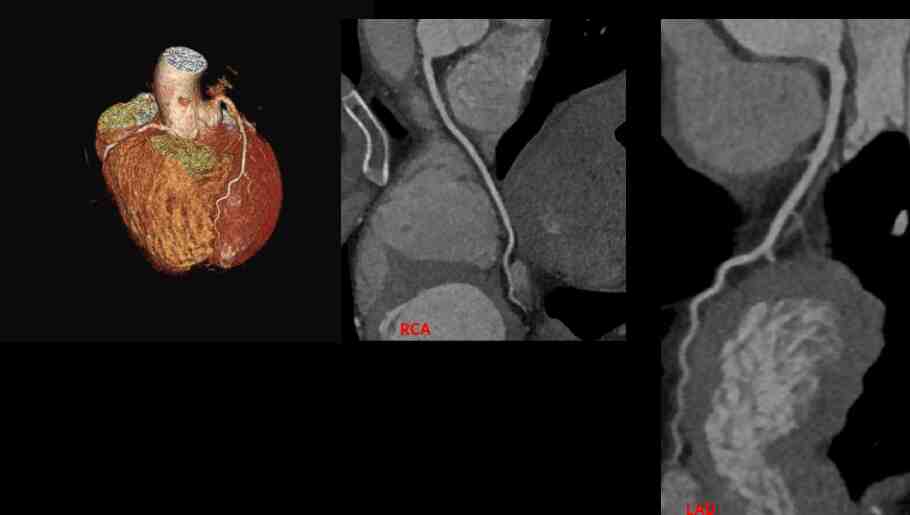
RCA LAD