What you need to know about NALOXONE Naloxone Administration
34 Slides7.43 MB
What you need to know about NALOXONE Naloxone Administration Training Yenh Long, Pharm.D., BCACP Prescription Monitoring Program (PMP) Administrator Nevada Board of Pharmacy
2 Learning Objectives Understand pain and how opioids work in the body Explain how to recognize and respond to an opioid overdose Understand the role of naloxone in an opioid overdose and how it can prevent an overdose death Demonstrate how to use the various formulations of naloxone
3 Good Samaritan Drug Overdose Act Senate Bill 459 Signed into law May 5, 2015 Effective October 1, 2015
4 Good Samaritan Drug Overdose Act Established 4 channels a patient may obtain/receive naloxone 1. Law enforcement officers may possess and administer naloxone 2. Prescribers may prescribe naloxone to a person other than the patient such as a family member/friend/other person 3. Unlicensed person or entity may store and/or dispense naloxone without charge or compensation under a standing order from an authorized prescriber 4. Pharmacists may dispense naloxone under a pharmacy standardized procedure or physician written protocol without RX
5 Good Samaritan Drug Overdose Act Built-in protection from liability A person who, acting in good faith and with reasonable care, prescribes, dispenses, or administers naloxone pursuant is not subject to any criminal or civil liability or any professional disciplinary action for: (a) Such prescribing or dispensing; or (b) Any outcomes that result from the eventual administration of naloxone. 5
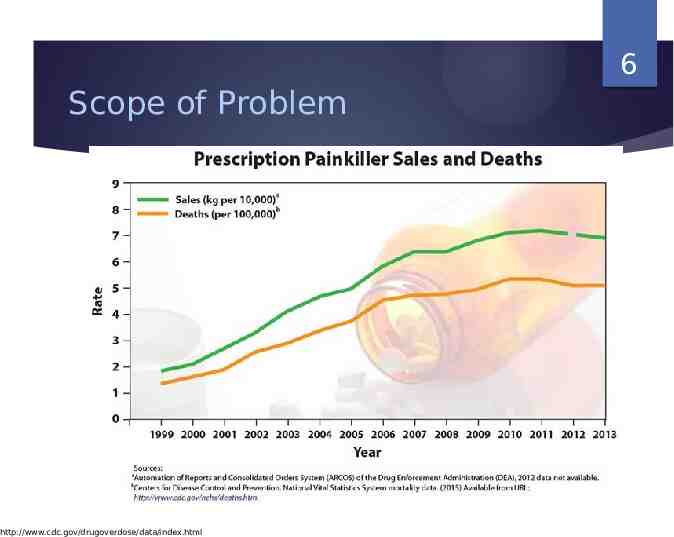
6 Scope of Problem http://www.cdc.gov/drugoverdose/data/index.html
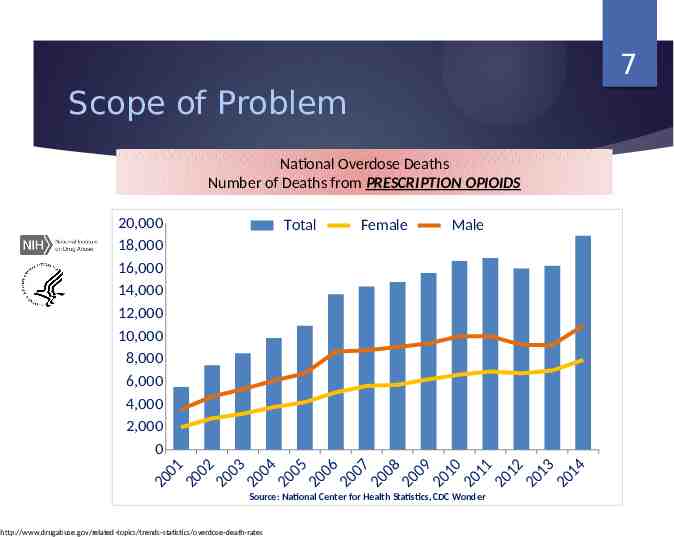
7 Scope of Problem National Overdose Deaths Number of Deaths from PRESCRIPTION OPIOIDS 20,000 18,000 16,000 14,000 12,000 10,000 8,000 6,000 4,000 2,000 0 Total Female Male 0 1 00 2 00 3 0 0 4 00 5 00 6 0 07 0 0 8 0 0 9 01 0 0 11 0 12 0 1 3 0 14 0 2 2 2 2 2 2 2 2 2 2 2 2 2 2 Source: National Center for Health Statistics, CDC Wonder http://www.drugabuse.gov/related-topics/trends-statistics/overdose-death-rates
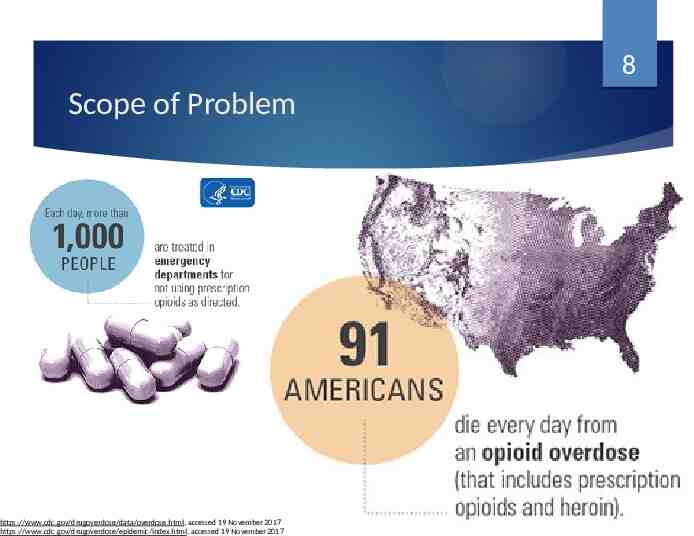
8 Scope of Problem https://www.cdc.gov/drugoverdose/data/overdose.html, accessed 19 November 2017 https://www.cdc.gov/drugoverdose/epidemic/index.html, accessed 19 November 2017
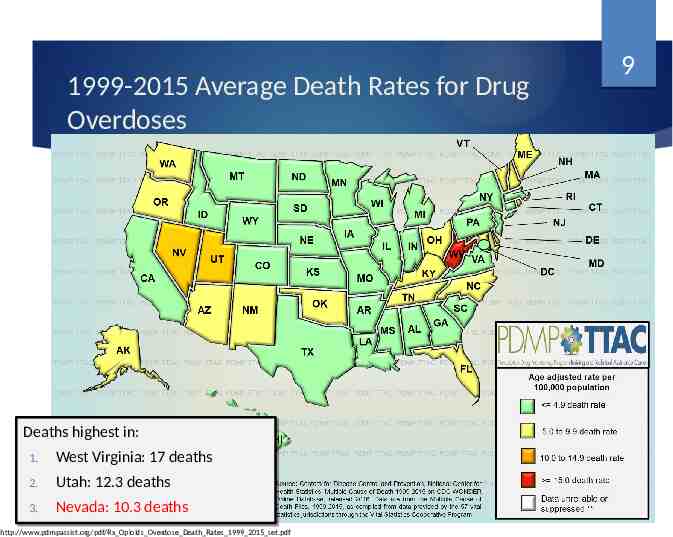
1999-2015 Average Death Rates for Drug Overdoses Deaths Deaths highest highest in: in: 1. 1. West West Virginia: Virginia: 17 17 deaths deaths 2. 2. 3. 3. Utah: Utah: 12.3 12.3 deaths deaths Nevada: Nevada: 10.3 10.3 deaths deaths http://www.pdmpassist.org/pdf/Rx Opioids Overdose Death Rates 1999 2015 set.pdf 9
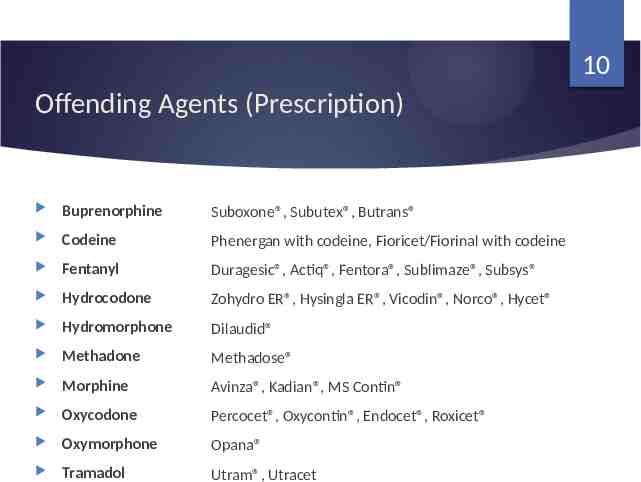
10 Offending Agents (Prescription) Buprenorphine Suboxone , Subutex , Butrans Codeine Phenergan with codeine, Fioricet/Fiorinal with codeine Fentanyl Duragesic , Actiq , Fentora , Sublimaze , Subsys Hydrocodone Zohydro ER , Hysingla ER , Vicodin , Norco , Hycet Hydromorphone Dilaudid Methadone Methadose Morphine Avinza , Kadian , MS Contin Oxycodone Percocet , Oxycontin , Endocet , Roxicet Oxymorphone Opana Tramadol Utram , Utracet
11 Offending Agents (Illicit) Heroin Common street names used by dealers and addicts to describe heroin in its various forms (cut with cocaine, marijuana, Fentanyl, MDMA, methamphetamine) http://heroin.net/about/street-names-for-heroin/
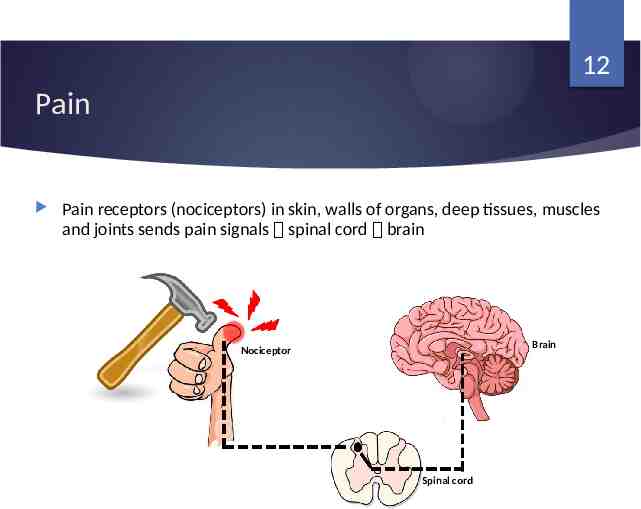
12 Pain Pain receptors (nociceptors) in skin, walls of organs, deep tissues, muscles and joints sends pain signals spinal cord brain Brain Nociceptor Spinal cord
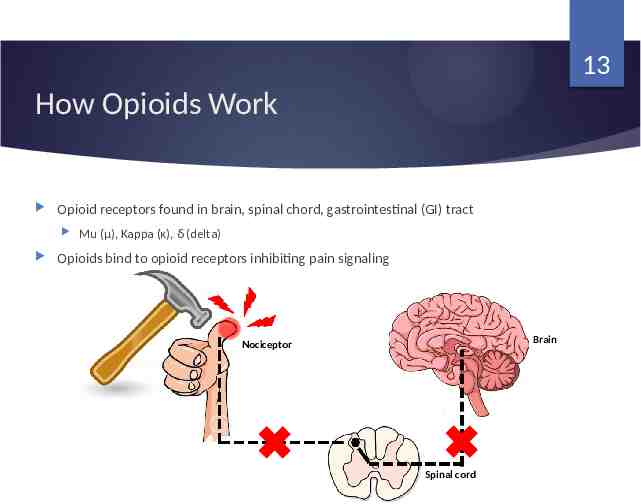
13 How Opioids Work Opioid receptors found in brain, spinal chord, gastrointestinal (GI) tract Mu (μ), Kappa (κ), δ (delta) Opioids bind to opioid receptors inhibiting pain signaling Brain Nociceptor Spinal cord
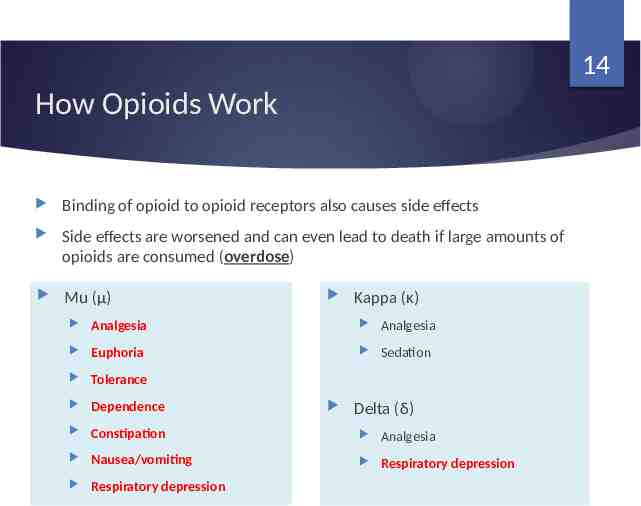
14 How Opioids Work Binding of opioid to opioid receptors also causes side effects Side effects are worsened and can even lead to death if large amounts of opioids are consumed (overdose) Mu (μ) Kappa (κ) Analgesia Analgesia Euphoria Sedation Tolerance Dependence Constipation Analgesia Nausea/vomiting Respiratory depression Respiratory depression Delta (δ)
15 Risk Factors for Opioid Overdose High-dose opioid prescription Decreased kidney, liver function Substance use disorder History of overdose Using opioids with other central nervous system depressants Reduced tolerance Benzodiazepine Muscle relaxants Alcohol Sleep aids Detoxification from hospital Release from incarceration Mental Health Disorder Changes in quality or purity of street heroin and fentanyl

16 Signs and symptoms of an Opioid Overdose If someone is making unfamiliar sounds while “sleeping” it is worth trying to wake him/her up. Many think this person is snoring, when in fact the person is overdosing. Vast majority of opioid overdoses are accidental and result from taking inappropriate doses of opioids or mixing with other substances. These poisonings typically take 45-90 minutes to turn fatal, creating an opportunity to intervene. http://harmreduction.org/issues/overdose-prevention/overview/overdose-basics/recognizing-opioid-overdose/ http://www.fraserhealth.ca/health-info/health-topics/harm-reduction/overdose-prevention-and-response/recognizing-an-overdose/recognizing-an-overdose

17 http://harmreduction.org/issues/overdose-prevention/overview/overdose-basics/responding-to-opioid-overdose/assessment-stimulation/
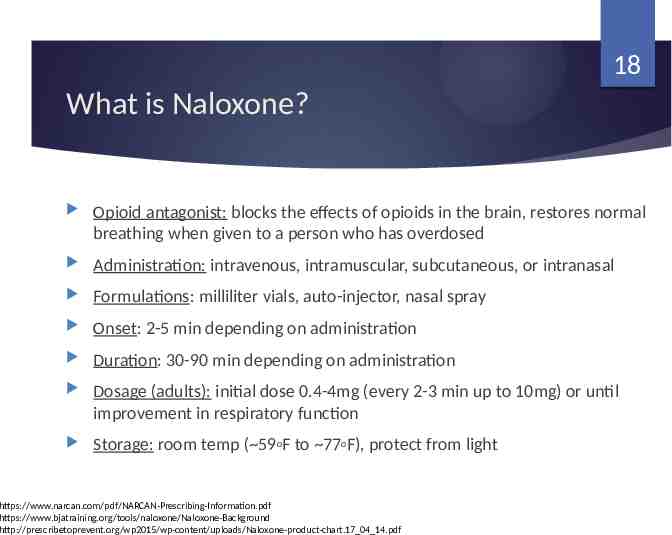
18 What is Naloxone? Opioid antagonist: blocks the effects of opioids in the brain, restores normal breathing when given to a person who has overdosed Administration: intravenous, intramuscular, subcutaneous, or intranasal Formulations: milliliter vials, auto-injector, nasal spray Onset: 2-5 min depending on administration Duration: 30-90 min depending on administration Dosage (adults): initial dose 0.4-4mg (every 2-3 min up to 10mg) or until improvement in respiratory function Storage: room temp ( 59oF to 77oF), protect from light 18 https://www.narcan.com/pdf/NARCAN-Prescribing-Information.pdf https://www.bjatraining.org/tools/naloxone/Naloxone-Background http://prescribetoprevent.org/wp2015/wp-content/uploads/Naloxone-product-chart.17 04 14.pdf
19 What is Naloxone? Adults/Pediatrics/Geriatric/Pregnant: Adults and pediatrics over age one year: use as instructed Geriatric over age 65 years: clinical experience has not identified differences in responses between the elderly and younger patients. Pregnant: limited data on naloxone use in pregnant women. Naloxone crosses placenta, may cause withdrawal to the fetus. Consider benefits to mother and risk to fetus before administration. Pediatrics less than one year: neonatal opioid withdrawal syndrome, unlike opioid withdrawal syndrome in adults, may be life-threatening. Consider use of an naloxone product that can be dosed according to weight and titrated to effect. 19 https://www.narcan.com/pdf/NARCAN-Prescribing-Information.pdf https://www.bjatraining.org/tools/naloxone/Naloxone-Background http://prescribetoprevent.org/wp2015/wp-content/uploads/Naloxone-product-chart.17 04 14.pdf
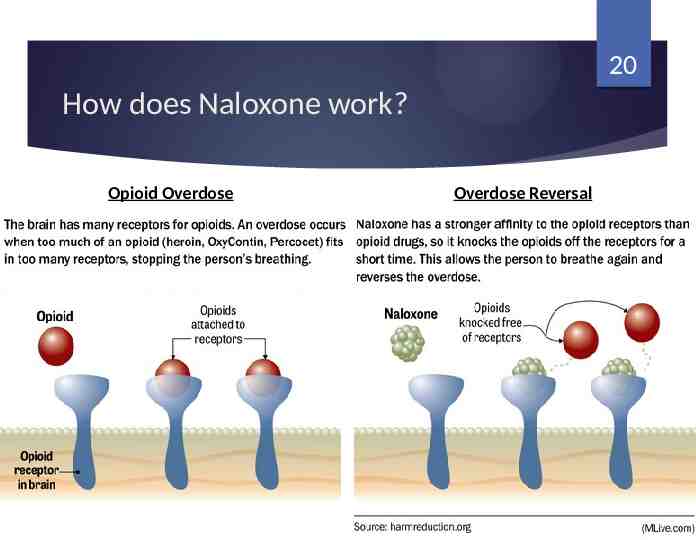
20 How does Naloxone work? Opioid Overdose Overdose Reversal
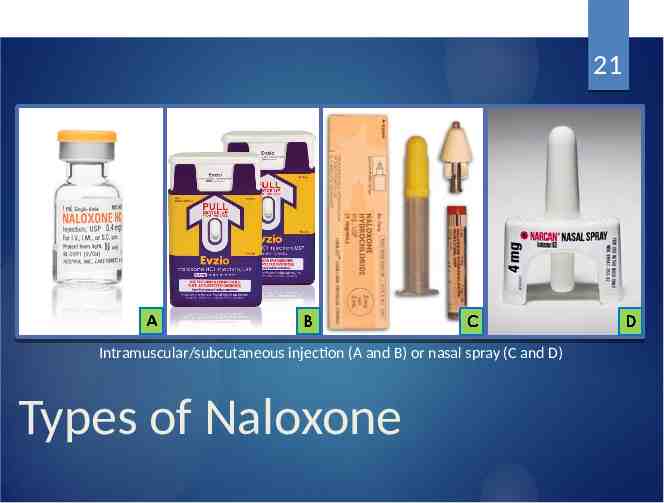
21 Intramuscular/subcutaneous injection (A and B) or nasal spray (C and D) Types of Naloxone
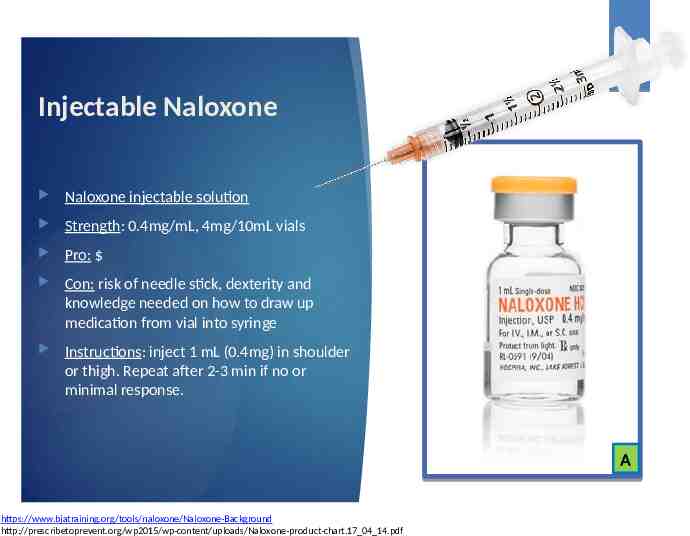
22 Injectable Naloxone Naloxone injectable solution Strength: 0.4mg/mL, 4mg/10mL vials Pro: Con: risk of needle stick, dexterity and knowledge needed on how to draw up medication from vial into syringe Instructions: inject 1 mL (0.4mg) in shoulder or thigh. Repeat after 2-3 min if no or minimal response. A https://www.bjatraining.org/tools/naloxone/Naloxone-Background http://prescribetoprevent.org/wp2015/wp-content/uploads/Naloxone-product-chart.17 04 14.pdf
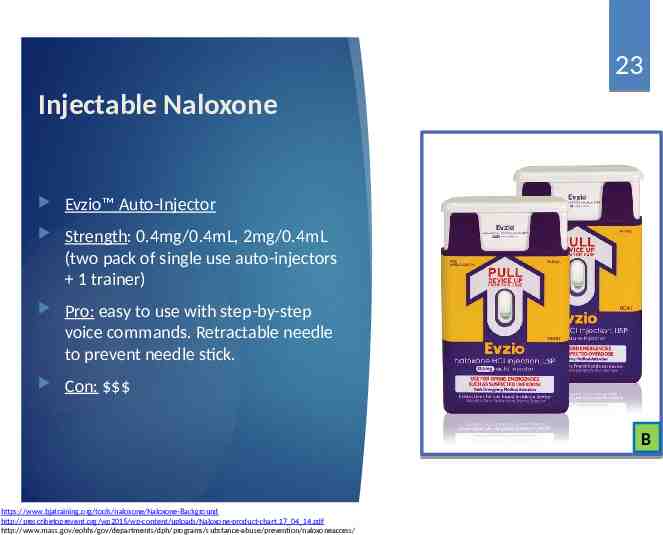
23 Injectable Naloxone Evzio Auto-Injector Strength: 0.4mg/0.4mL, 2mg/0.4mL (two pack of single use auto-injectors 1 trainer) Pro: easy to use with step-by-step voice commands. Retractable needle to prevent needle stick. Con: B https://www.bjatraining.org/tools/naloxone/Naloxone-Background http://prescribetoprevent.org/wp2015/wp-content/uploads/Naloxone-product-chart.17 04 14.pdf http://www.mass.gov/eohhs/gov/departments/dph/programs/substance-abuse/prevention/naloxoneaccess/
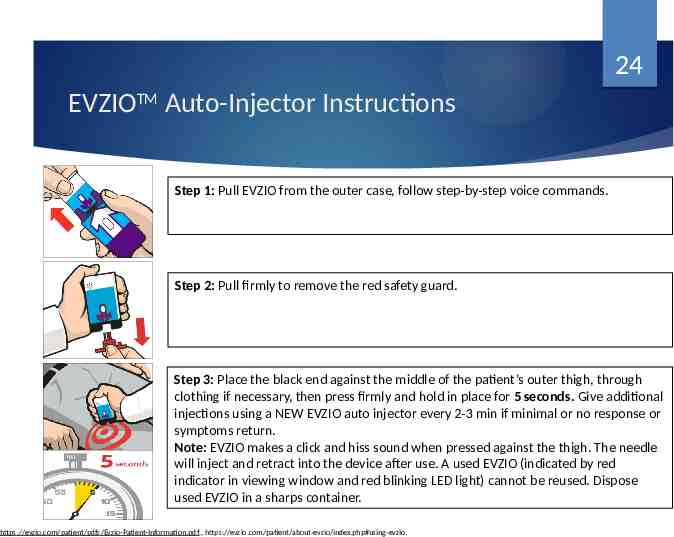
24 EVZIOTM Auto-Injector Instructions Step 1: Pull EVZIO from the outer case, follow step-by-step voice commands. Step 2: Pull firmly to remove the red safety guard. Step 3: Place the black end against the middle of the patient’s outer thigh, through clothing if necessary, then press firmly and hold in place for 5 seconds. Give additional injections using a NEW EVZIO auto injector every 2-3 min if minimal or no response or symptoms return. Note: EVZIO makes a click and hiss sound when pressed against the thigh. The needle will inject and retract into the device after use. A used EVZIO (indicated by red indicator in viewing window and red blinking LED light) cannot be reused. Dispose used EVZIO in a sharps container. https://evzio.com/patient/pdfs/Evzio-Patient-Information.pdf., https://evzio.com/patient/about-evzio/index.php#using-evzio.
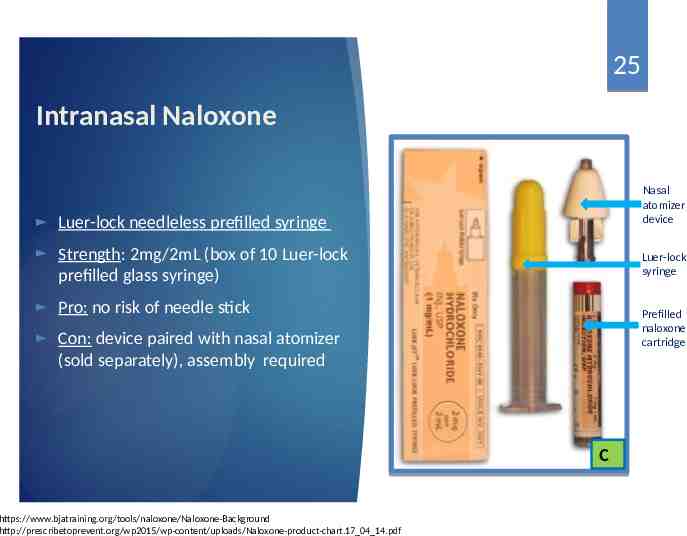
25 Intranasal Naloxone Luer-lock needleless prefilled syringe Strength: 2mg/2mL (box of 10 Luer-lock prefilled glass syringe) Pro: no risk of needle stick Con: device paired with nasal atomizer (sold separately), assembly required Nasal atomizer device Luer-lock syringe Prefilled naloxone cartridge C https://www.bjatraining.org/tools/naloxone/Naloxone-Background http://prescribetoprevent.org/wp2015/wp-content/uploads/Naloxone-product-chart.17 04 14.pdf
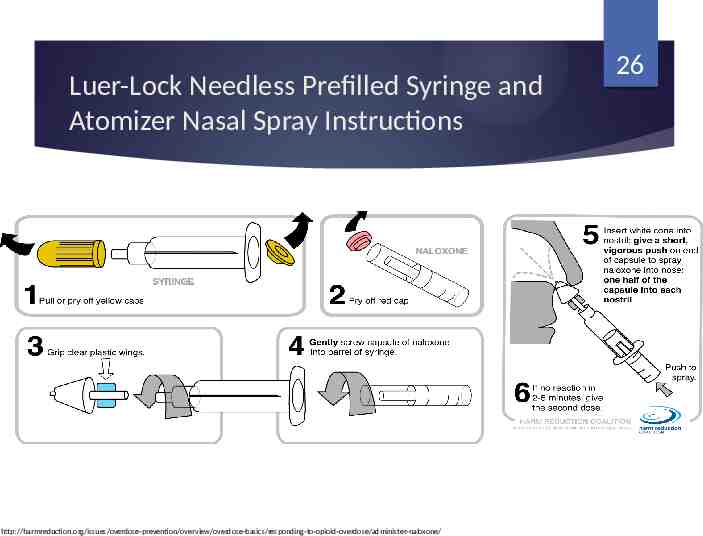
Luer-Lock Needless Prefilled Syringe and Atomizer Nasal Spray Instructions http://harmreduction.org/issues/overdose-prevention/overview/overdose-basics/responding-to-opioid-overdose/administer-naloxone/ 26
27 Intranasal Naloxone Narcan Nasal Spray Strength: 4mg/0.1mL, 2mg/0.1ml (two-pack of single use intranasal device) Pro: no risk of needle stick Con: n/a D Image: https://www.bjatraining.org/naloxone/narcan-naloxone-nasal-spray-approved-usfood-and-drug-administration https://www.narcan.com/pdf/NARCAN-Prescribing-Information.pdf
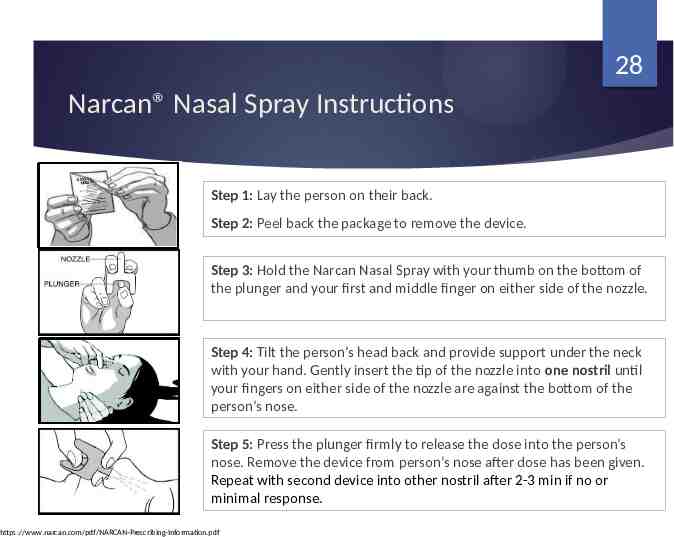
28 Narcan Nasal Spray Instructions Step 1: Lay the person on their back. Step 2: Peel back the package to remove the device. Step 3: Hold the Narcan Nasal Spray with your thumb on the bottom of the plunger and your first and middle finger on either side of the nozzle. Step 4: Tilt the person’s head back and provide support under the neck with your hand. Gently insert the tip of the nozzle into one nostril until your fingers on either side of the nozzle are against the bottom of the person’s nose. Step 5: Press the plunger firmly to release the dose into the person’s nose. Remove the device from person’s nose after dose has been given. Repeat with second device into other nostril after 2-3 min if no or minimal response. https://www.narcan.com/pdf/NARCAN-Prescribing-Information.pdf
29 Naloxone Side Effects Sudden opioid withdrawal symptoms Acute pain Sweating Body aches Nausea and vomiting Diarrhea Nervousness, anxiety Increased heart rate Restlessness or irritability Fever Shivering or trembling Runny nose Stomach cramping Sneezing Weakness Goose bumps Increased blood pressure https://www.narcan.com/pdf/NARCAN-Prescribing-Information.pdf
30 Additional Naloxone Education Naloxone not a substitute for emergency medical treatment Naloxone will not harm anyone who is not on opioids Depending on extent of overdose, more than one naloxone dose may be needed Duration of naloxone is generally shorter than opioids, repeat dosing is likely required after naloxone wears off in 30-90 min if patient does not seek emergency medical treatment Naloxone has a shelf life ranging from 18-24 months depending on the formulation
31 Success Stories Quincy, MA, Police Department launched its overdose reversal program in 2010. They trained patrol officers how to recognize and reverse opioid overdoses, and equipped them with naloxone. As of October 2015, they have reversed over 436 opioid overdoses. Suffolk County (NY) Police Department, May 2012, began a Narcan Pilot program. They Initially trained 400 officers. In the first five months there were 32 opioid overdose reversals. Because of the successes, the program was expanded. As of October 2015, more than 1,300 officers are trained and there have been 390 successful opioid overdose reversals. Lummi Nation Police Department (WA) in response to the increase in the number of overdose deaths on tribal lands and 20-minute ambulance response times, the Lummi Nation Police Department (WA) requested permission to participate in the overdose prevention program sponsored by the Lummi Nation Tribe. The program trained 20 officers. In the first six weeks of the program, Lummi officers successfully reversed three overdoses. https://www.bjatraining.org/tools/naloxone/Law-Enforcement-and-Naloxone
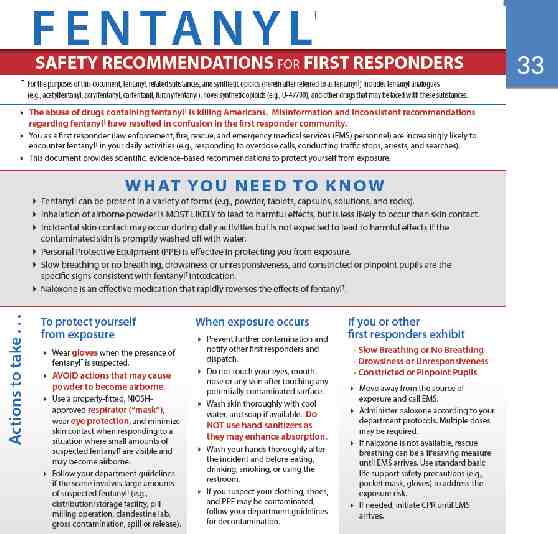
32 Resources Bureau of Justice Assistance (BJA) Law Enforcement Naloxone Toolkit https://www.bjatraining.org/tools/naloxone/Naloxone%2BBackground Resources to help LE agencies establish a naloxone program Answers to frequent questions about naloxone Downloadable sample documents/templates (data collection forms, standard operating procedures, training materials) November 1, 2017, White House released Fentanyl Safety Recommendations for First Responders. Provide first responders with information on how to protect themselves when the presence of fentanyl is suspected. https://www.bjatraining.org/tools/naloxone/Law-Enforcement-and-Naloxone
33
34 Contact Information Email: [email protected] Board tele: (775) 850-1440 PMP tele: (775) 687-5694