St. Joseph Mercy Health System Keystone ICU Collaborative: Making
56 Slides4.46 MB
St. Joseph Mercy Health System Keystone ICU Collaborative: Making your ICUs safer The secret ingredients are culture and team Pat Posa RN, BSN, MSA System Performance Improvement Leader St. Joseph Mercy Health System Ann Arbor, MI [email protected]

Statewide initiative-75 Hospitals, 127 ICUs In Collaboration with Johns Hopkins’Quality and Research Institute Reduce errors and improve patient outcomes in ICUs Combination of evidence based medicine and quality improvement 5 interventions implemented over a 2 year Grant funded period Still going strong after 7 years!!!!

Science of Safety(CUSP) BSI VAP Daily Goals Sepsis Oral Care Delirium and Progressive mobility Partnership between Johns Hopkins University and MHA Initiated with AHRQ Matching Grant Sustained with participant fees in 2005 and 2006

St. Joseph Mercy Hospital Story CUSP in the ICU and beyond Building on CUSP and CLABSI/CAUTI for other work Technical (evidence based practices) Adaptive (communication and teamwork) HAI infection prevention MDR with daily goals Sepsis identification and management Morning briefings/pre-procedure briefings Intra-abdominal HTN Learn from defects Delirium Huddles Progressive mobility Crucial Conversations training Just Culture training

Start with: Keystone ICU Team Denise Harrison RN, MSN, Director of Critical Care Christine Curran, MD, medical director, MICU Mary-Anne Purtill MD, medical director SICU Pat Posa RN, MSA, system performance improvement leader Marco Hoesel MD, surgical resident Amy Heeg RN, BSN CCU-Livingston Brian Kurylo RN, CCU Cathy Stewart RN, BSN, CCRN Resourse Pool Toy Bartley, RN, Clinical nurse leader, MICU Diane Jones PA, cardiac surgery David Holmes, cardiac surgery Sondra RN CCU-Livingston Andreea Sandu RN, MICU Nancy Payne RN, MICU Laura Buwalde, RN, SICU Emily McGee, RN, Clinical Nurse Leader, SICU Shikha Kapila, Pharm. D Cheryl Morrin MPH, infection control Chris Kiser, Pharmacy, Livingston Beverly Bay-Jones, RRT, Resp Therapy Tahnee Thibodeau., RD, MICU dietitican Wendy Nieman RN, Project Impact

The “Secret Ingredient” Comprehensive Unit-Based Patient Safety Program Pre-CUSP work Form a unit CUSP team Measure unit culture 1.Educate staff on Science of Safety 2.Identify defects using the Staff Safety Assessment; prioritize defects 3.Executive adopts the unit 4.Learn from one defect per quarter 5.Implement team/communication tools Keep focus on this throughout the journey!!!

What is a Culture? That’s not the way we do it here!!! Represents a set of shared attitudes, values, goals, practice & behaviors that makes one unit distinct from the next Measure culture at the unit level Pronovost, PJ et al. Clin Chest Med, 2009;30:169-179

Unit CUSP team/Culture measurement and action plan Unit teams meeting at least monthly? What are your challenges? What strategies have been successful? Developed action plan from culture survey result? What are some of interventions you have implemented?

Understand system determines performance Use strategies to improve system performance Standardize Create Independent checks for key process Learn from Mistakes Apply strategies to both technical work and team work. Recognize that teams make wise decisions with diverse and independent input How we do this: Educate all personnel in all the ICU—RN, RT, residents, PA/NP Educate the attending---difficult but important Part of orientation

Medical errors most often result from a complex interplay of multiple factors. Only rarely Are they due to the carelessness or misconduct of single individuals Lucien L. Leape, MD Harvard School of Public Health

Why do mistakes happen “Every system is perfectly designed to achieve the results it gets”

Why Mistakes Happen? Variable input (diff pts) Inconsistency/variation Complexity Too many/complicated steps Human intervention Tight time constraints Hierarchical culture Fatigue Inattention/distraction Unfamiliar situations/new problem Using past solutions Equipment design flaws Communications errors Mislabeling/inadequate instructions Process Factors People Factors

Communication is Key Effective communication amongst caregivers is essential for a functioning team The Joint Commission reports that ineffective communication is the most commonly cited cause for a sentinel event Observations of ICU teams have shown errors in the ICU to be concentrated after communication events (shift change, handoffs, ect) 30% of errors are associated with communication between nurses and physicians Reader, CCM 2009 Vol 37 No 5; Donchin CCM 1995 Vol 23

Effective Teamwork and Communication Requires: Structured Communication Assertion/Critical Language SBAR, structured handoffs Key words, the ability to speak up and stop the show An environment of respect Psychological Safety Effective Leadership Flat hierarchy, sharing the plan, continuously inviting other team members into the conversation, explicitly asking people to share questions or concerns, using people’s names

Safety Issues Survey 1. 2. 3. Tell us about the last patient who would have been harmed without your intervention. How will the next patient be harmed? What steps can you do to prevent this harm? by either preventing the mistake, making the mistake visible or mitigating the harm should it occur This is a very important tool. Use this to identify some of the ‘whys’ mistakes are happening and what is impacting culture Taking an identified patient safety issue from the frontline staff and create an action plan to resolve this is an early win for this program and staff buy-in
Science of Safety Education/Staff Safety Assessment Challenging to educate attending physicians What strategies have you used? Staff safety assessment is very important tool How many have done this- once? 1 times? Have you utilized the LFD tool to help resolve issues identified?
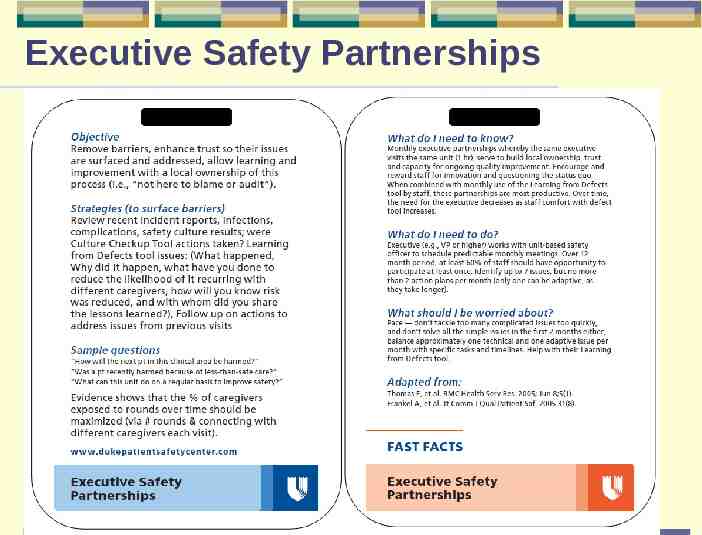
Executive Safety Partnerships Page 17

Best Practices: Humble Curiosity Help your staff to feel heard – unheard staff find an ear elsewhere, at your expense Remember your role as a leader isn’t always to solve problems, it is, at times to listen to staff and learn from them while you empathize Show curiosity in staff feedback – – Don’t be defensive: defensive leaders have defensive followers if you are defensive: “Why was that so low ,” they will be defensive and not engage instead engage “Teach me, what can be done to remove barriers so that your concerns are addressed?” 18

Learn from a Defect Tool Designed to rigorously analyze the various components and conditions that contributed to an adverse event and is likely to be successful in the elimination of future occurrences. Tool can serve to organize factors that may have contributed to the defect and provides a logical approach to breaking down faulty system issues.

Learning from Defects Tool Page 20

Finding Defects to Learn From Staff feedback/issues identified on unit Event reporting Quality and safety measures Gaps in application of the evidence Have staff complete short 3 question survey

Mistakes and near misses are defects Have each ICU present learning from a defect each quarter----now doing monthly NG placed in the lungs Missed respiratory treatments Delay in radiology tests for ICU pts Non-compliance with contact precautions This is very hard to continue to do, we did it first for the first year. We didn’t keep it up----but are now doing this almost daily through our huddles, The biggest challenge is following up on each action plan giving the feedback to the staff.

Learn from Defect How many are doing this on the unit— quarterly? Monthly? How are you sharing the learnings with the unit staff and beyond?

Daily rounds/goals Pre-procedure briefing Morning briefing Huddles Learn from a defect Executive Safety Rounds Standardize handoffs Simulation Crucial Conversations

Interdisciplinary rounds with daily goals Purpose: Improve communication among care team and family members regarding the patient’s plan of care Goals should be specific and measurable Documented where all care team members have access Checklist used during rounds prompts caregivers to focus on what needs to be accomplished that day to safely move the patient closer to transfer out of the ICU or discharge home Measure effectiveness of rounds—team dynamics, communication

MDR with DG Action Plan Task Obtain executive buy-in Define members of rounds and their roles Define time of day and frequency Structure of rounds: Review of systems (or major issues) Define components of checklist Time for each patient Documentation: What is documented in medical record daily goal—where is it documented? Educating staff Define metrics and evaluation process 26 Responsibility Due Date

Interdisciplinary rounds with daily goals--Challenges and Opportunities Hardest initiative to implement, especially if you have an open unit and/or no intensivists and on floors without dedicated physician team assigned to unit We had each unit create their own daily goal checklists---each unit culture and process is different. Changed this form multiple times---and in two units we gave up. Focused first on create a daily goal and recording those either on the white board in the room or on a sheet of paper Two years ago: closed our MICU and started intensivist program in the SICU Relooked at this again, and focused on team dynamics and created a defined role for the nurse: survey and observation

Nursing Card VAP Delirium Sepsis 28

MDR with Daily Goals Anyone done this successfully in an open ICU or in a non-ICU unit (without dedicated physician staff)? What strategies did you use that lead to your success?

Pre-procedure briefing Make introductions Discuss patient information and procedure Agree upon a time for line insertion Review best practice for line insertion (if necessary) Nurse defines their role to physician: provide equipment, monitor patient, provide patient comfort, observe for compliance with best practices and STOP procedure if sterile process compromised Establish communication expectation for sterile procedure breaks Examples include: your sleeve has touched the IV pole, the guidewire touched the headboard Identify any special supply or procedural needs Discuss any special patient issues (IE: patient confused, patient awake) Answer any additional questions TIME OUT: RIGHT PATIENT---RIGHT PROCEDURE Used this when rolled out CLABSI bundle to non-ICU

Morning Briefing Purpose: Increase communication between physicians and nursing staff while efficiently prioritizing patient care delivery and ICU admissions and discharges What is it? A morning briefing is a dialogue between 2 or more persons using concise and relevant information to promote effective communication prior to rounds Have used this for a long time between charge nurses from shift to shift. Since we have closed the units, now this also occurs with charge nurse and intensivist.

Morning Briefing Tool: answer following questions What happened overnight that I need to know about? Where should I begin rounds? (patient that requires immediate attention based on acuity) Which patients do you believe will be transferring out of the unit today? Who has discharge orders written? How many admissions are planned today? What time is the first admission?

Huddles Enable teams to have frequent but short briefings so that they can stay informed, review work, make plans, and move ahead rapidly. Allow fuller participation of front-line staff and bedside caregivers, who often find it impossible to get away for the conventional hour-long improvement team meetings. They keep momentum going, as teams are able to meet more frequently. Improve staff’s situational awareness Beginning to use this strategy to begin to recovery immediately from defects--IE: falls, sepsis

Components Components Metric 1: Quality/Safety Metric 2: Patient Satisfaction Metric 3: Operations Daily Critical Communications Information Ideas in Motion How to do it? Beginning or mid shift 5-10 minutes Lead by member of unit leadership team 34

Structured Huddles Action Plan Task Obtain executive buy-in Order Huddle board Select Huddle metrics for first board: operational, quality/safety and patient satisfaction Define huddle process: Define time of day and frequency Who will lead huddle Expectations of staff—who will attend Create agenda (in first huddles include overview of purpose of huddles and huddle process) Hang huddle board and fill in metrics Identify when huddles will begin Define process for changing huddle metrics Create evaluation process: how will I know if huddles are successful? 35 Responsibility Due Date

SICU Huddle Board 36

Surgical Unit Huddle Board

Medical Unit Huddle Board

Safety Climate-Michigan ICUs Sexton, CCM 2011 39

100 % of respondents within an ICU reporting good teamwork climate 90 80 70 Teamwork Climate Across Michigan ICUs The strongest predictor of clinical excellence: caregivers feel comfortable speaking up if they perceive a problem with patient care 60 50 40 30 20 10 No BSI 5 months or more w/ zero No BSI 21% No BSI 31% No BSI 44% 0 Health Services Research, 2006;41(4 Part 40 II):1599.

100 Teamwork Climate & Annual Nurse Turnover % reporting positive teamwork climate 90 80 70 60 50 40 30 20 High Turnover 10 16.0% Mid Turnover 10.8% Low Turnover 7.9% 0 RN Teamwork Climate Staff Physician Teamwork Climate 41

“Needs Improvement” Statewide Michigan CUSP ICU Results “Needs Improvement” means less than 60% of respondents reported good safety climate Statewide in 2004 84% needed improvement, in 2007 23% Safety Climate item that drives improvement: “I am encouraged by my colleagues to report any patient safety concerns I may have” 42
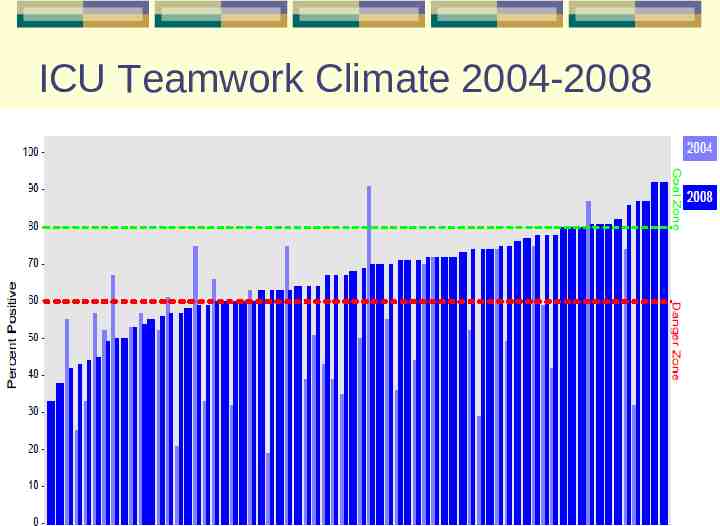
ICU Teamwork Climate 2004-2008

ICU Safety Climate 2004 - 2008

Impact of a statewide intensive care unit quality improvement initiative on hospital mortality and length of stay BMJ, February 2011 Method Retrospective comparative analysis Study period: October 2001 to December 2006 Study sample: all hospital admissions with an ICU stay for adults age 65 or older at hospitals with 50 or more acute care beds and 200 or more admissions to the ICU during that time period 95 study hospitals in Michigan compared with 364 hospitals in surrounding Midwest region Look at hospital mortality and length of hospital stay
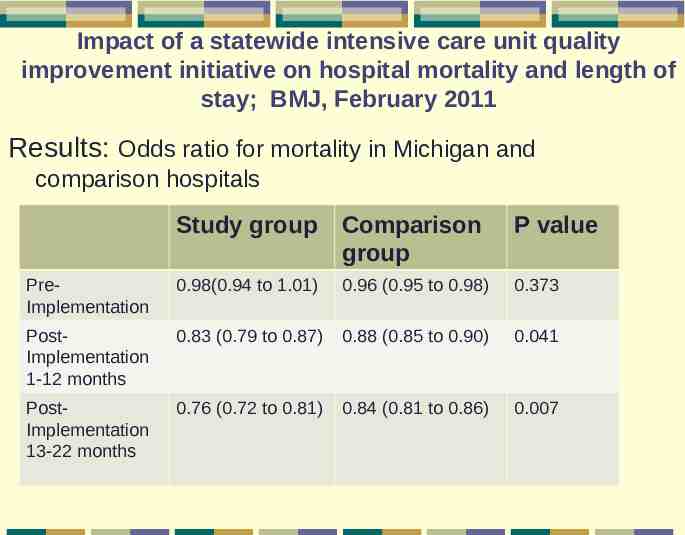
Impact of a statewide intensive care unit quality improvement initiative on hospital mortality and length of stay; BMJ, February 2011 Results: Odds ratio for mortality in Michigan and comparison hospitals Study group Comparison group P value PreImplementation 0.98(0.94 to 1.01) 0.96 (0.95 to 0.98) 0.373 PostImplementation 1-12 months 0.83 (0.79 to 0.87) 0.88 (0.85 to 0.90) 0.041 PostImplementation 13-22 months 0.76 (0.72 to 0.81) 0.84 (0.81 to 0.86) 0.007

Why Crucial Conversations? 2005 study by AACN and Vital Smarts: Silence Kills 1,700 nurses, physicians, clinical care staff and administrators More than 50% witnessed their co-workers breaking rules, making mistakes, failing to support others, demonstrating incompetence, showing poor teamwork, acting disrespectfully and micromanaging Despite the risk to patients, less than 10% of physicians, nurses, and other clinical staff directly confronted their colleagues about their concerns 195,000 deaths per year in US hospitals because of medical mistakes

Why Crucial Conversations? 2010 Silent Treatment Study—AACN, AORN and Vital Smarts Healthcare has made great strides over past 5 years to improve systems to prevent errors Safety tools are an essential part of the formula for solving avoidable medical errors caused by poor communication. Silent Treatment study of 6,500 nurses and nurse managers reveals that safety tools fail to address a second category of communication breakdowns---undiscussables. Tools don’t create safety—people do In study—85% of respondents had been in a situation where a safety tool warned them of a problem----BUT 58% had also been in situations where they felt unsafe to speak up about the problems or were not able to get others to listen Staff need the tools to know how to effectively speak up!

Principles of Crucial Conversations Start with Heart How to stay focused on what you really want. Learn to Look How to notice when safety is at risk. Make it Safe How to Make it Safe to Talk about Almost Anything. How to create mutual purpose.

Principles of Crucial Conversations Master my Stories How to stay in dialogue when you’re angry, scared, or hurt How to Master Emotions and return to dialogue STATE my Path How to speak persuasively, not abrasively Explore others Path How to listen when others blow up or clam up Seek First to Understand Then to be Understood Move to Action How to turn crucial conversations into action and results

Teamwork/Communication Tools Anyone implemented any team tools? Morning briefings? Pre-procedure briefings? Structured huddles? Crucial Conversations? What are some of your successes/challenges?

CUSP-Challenges and Strategies Issues Strategies Engaging frontline staff (including off-shifts) owning this work Part of team(especially night shift staff), bulletin boards, newsletters, huddles Timely follow through with identified defects or safety issues and strategies to resolve Manager shares updates/status at staff meetings, communication at huddles, created huddle book Continued engagement of the executive MHA Keystone letters to executive, locally at each hospital—through one on one conversations Implementing strategies and tools to Learn from a defect, MDR with focus help improve culture and teamwork on communication, survey team members on perception of communication, morning briefings, debriefings, huddles, crucial conversations Continual learning from defects Have each unit learn from a defect monthly and share at meetings

Lessons Learned Spend sufficient time on CUSP before moving on to implementing practice changes CUSP is the foundation and needs to be a continued focus----forever!!!! Must work on culture and team improvement strategies throughout the journey CUSP must be unit based. Culture is different on each unit, therefore opportunities for improvement and strategies might be different Define at beginning a communication plan that includes all levels of the organization This work must be the responsibility of everyone, but important to have someone who’s job is to focus and drive this daily

Can Can we we change change practice practice through through process process improvement improvement alone? alone? or Will Will successful successful change change require require an an altering altering of of the the value value structure structure within within the the unit? unit?

A Healthcare Imperative “In medicine, as in any profession, we must grapple with systems, resources, circumstances, people-and our own shortcomings, as well. We face obstacles of seemingly endless variety. Yet somehow we must advance, we must refine, we must improve.” Atul Gawande, Better: A Surgeon’s Notes on Performance

QUESTIONS ?