Provider Training: Claims Operations October 1, 2021 1
20 Slides4.44 MB
Provider Training: Claims Operations October 1, 2021 1

Claims Submissions Benefit Plan **Reminder: Participating providers should review the contractual agreements with MetroPlusHealth for timely filing guidelines as they may vary. Claim Submission Deadline (days following date of service/ discharge) Medicare, Medicaid, and Family Health Plus 90 days MetroPlus Gold and Child Health Plus 120 days 30 days following MetroPlusHealth’s request to the IPA or IPA Provider as applicable, for additional Information 60 days following receipt of an explanation of benefits from a primary payer if MetroPlusHealth is secondary 2

Claims Submissions, Cont. Providers can submit all 837 EDI claims via the below Trading Partners for all members using MetroPlus Receiver ID# 13265 Relay Health please use submitter ID#: 910842999 Emdeon please use submitter ID# 133052274 Paper claims must be submitted on CMS 1500 or UB-04 forms Send paper claims for Medicaid, CHP, EP, SNP, MetroPlus Gold, Send paper claims for Managed Long-Term Care (MLTC), MetroPlus MetroPlus MedicareEnhanced to: (HARP) and QHP (Exchange) to: MetroPlus Health Plan MetroPlus Health Plan P.O. Box 381508 P.O. Box 830480 Birmingham, AL 35238Birmingham, AL 35283-0480 1508

Claims Submissions & Status Providers may not balance bill members above allowed co-pays, deductibles, or co-insurance for any covered services. Balance billing is prohibited. If provider seeks payment from a member for any covered service, contractor may be subject to termination as a participating provider. Provider is required to educate their staff and affiliated providers concerning this requirement. Check Claim Status MetroPlus Provider Portal: http://providers.metroplus.org MetroPlus Customer Services: 800-303-9626 4

Did You Remember to ? Include the correct rate and service code/modifier combination Determine if prior auth is required for the service being rendered Use the appropriate NPI/taxonomy code combination for Behavioral Health (BH) services Apply rate codes only to the UB04 and not the CMS 1500 Bill in accordance with the Provider’s contract and licensure 5

HARP: Home & Community Based Services (HCBS) for Adults 21 Years & Older HCBS services are only available to HARP enrollees who have been qualified through the assessment process and HARP eligible individuals enrolled in HIV-SNPs and assessed as HCBS eligible Providers must submit claims on 837i or UB-04 ‘Facility’ claim forms. Providers should submit one rate code per claim, and use revenue codes 0513,0520,0900 & 0914 The Level of Service Determination authorizes three visits within 14 days for providers to complete the Individual Service Plan and submit a request for the full frequency, scope, and duration of HCBS services. Providers submit claims for these visits using the corresponding coding combinations that are designated for the HCBS service being assessed. A minimum of eight minutes must be provided to bill for one 15-minute unit. Partial units totaling less than eight minutes may not be billed. Units totaling more than eight minutes may be rounded up and billed as one unit. 6

Allowable Service Combinations Only Certain Combinations of HCBS & State Plan Services Are Allowed by Medicaid within an Individual’s Current Treatment Plan. The Grid Below Shows the Allowable Service Combinations. Plan Services HCBS Services OMH Clinic/OLP OASAS Clinic OASAS Opioid Treatment Program OMH ACT OMH PROS OMH IPRT/CDT OMH Partial Hospital OASAS Outpatient Rehab PSR Yes Yes Yes No No No Yes No CPST No No No No No No Yes No Habilitation Yes Yes Yes No No No Yes No Family Support and Training Yes Yes Yes No No Yes Yes Yes Education Support Services Yes Yes Yes No Yes Yes Yes Yes Peer Support Services Yes Yes Yes No Yes Yes Yes Yes Employment Services Yes Yes Yes No No Yes Yes Yes 7

HARP HCBCS Services: Psychosocial Rehabilitation (PSR) · Community Psychiatric Support and Treatment (CPST) · Habilitation/Residential Support Services · Family Support and Training · Short-term Crisis Respite · Intensive Crisis Respite · Education Support Services · Empowerment Services – Peer Supports · Pre-Vocational Services · Transitional Employment · Intensive Supported Employment (ISE) · Ongoing Supported Employment · Staff Transportation · Non-Medical Patient Transportation BH HCBS Coding Guide Rate Code Rate Code Description CPT Code CPT Code Description Modifier(s) Unit Measure Unit Range Notes 7784 Psychosocial Rehab Individual - on-site H2017 Psychosocial rehabilitation services; per 15 minutes U1 Per 15 min 1-8 On-site rate code. Use U1 modifier. Do not bill transportation supplement. 7785 Psychosocial Rehab Individual - off-site H2017 Psychosocial rehabilitation services; per 15 minutes U2 Per 15 min 1-8 Off-site rate code. Use U2 modifier. Bill transportation supplement as appropriate. 7786 Psychosocial Rehab Group 2-3 H2017 Psychosocial rehabilitation services; per 15 minutes UN or UP Per 15 min 1-4 On-site or off-site. Use appropriate modifier. Bill staff transportation supplement as appropriate (but only for a single recipient). 7787 Psychosocial Rehab Group 4-5 H2017 Psychosocial rehabilitation services; per 15 minutes UQ or UR Per 15 min 1-4 On-site or off-site. Use appropriate modifier. Bill staff transportation supplement as appropriate (but only for a single recipient). 8

BH HCBS Coding Guide, Cont. Rate Code Rate Code Description CPT Code CPT Code Description 7788 Psychosocial Rehab Group 6-10 H2017 7789 Psychosocial Rehab Individual - Per Diem 7800 Modifier(s) Unit Measure Unit Range Notes Psychosocial rehabilitation US services; per 15 minutes Per 15 min 1-4 On-site or off-site. Use appropriate modifier. Bill staff transportation supplement as appropriate (but only for a single recipient). Maximum group size is 10. H2018 Psychosocial Rehabilitation; per diem Per diem 1 On-site or off-site. Bill transportation supplement as appropriate. Minimum of 3 hours. Family Support / Training (group of 2 or 3) H2014 Skills training and development; per 15 minutes Per 15 min 1-6 On-site or off-site. Bill transportation supplement as appropriate. Use modifiers. 7801 Pre-vocational T2015 Habilitation prevocational, waiver; per hour Per hour 1-2 Service must be one-to-one. Bill transportation supplement as appropriate. Must comply with VP/IDEA restrictions. 7802 Transitional Employment T2019 Habilitation, supported employment, waiver; per 15 minutes Per 15 min 1-12 Service must be one-to-one. Bill transportation supplement as appropriate. Must comply with VP/IDEA restrictions. HR or HS, UN or UP 9

BH HCBS Coding Guide, Cont. Rate Code Rate Code Description CPT Code CPT Code Description Modifier(s) Unit Measure Unit Range Notes 7803 Intensive Supported Employment H2023 Supported Employment TG Per 15 min 1-12 Service must be one-to-one. Bill transportation supplement as appropriate. Must comply with VP/IDEA restrictions. 7804 On-going Supported Employment H2025 Ongoing support to maintain employment, Per 15 min 1-12 Service must be one-to-one. Bill transportation supplement as 7805 Education Support Services T2013 Habilitation educational, waiver Per hour 1-2 Service must be one-to-one. Bill transportation supplement as appropriate. Must comply with VP/IDEA restrictions. 10

Children’s Home & Community Based Services (CHCBS) Children & Family Treatment & Support Services (CFTSS) - Children and Youth Under Age 21 What are children’s Home & Community Based Services (HCBS), also called children’s HCBS? Enrolled or eligible to enroll in New York State Medicaid; and Have physical and/or mental health needs or have a developmental disability and live-in foster care that put them at risk of needing care in places like a long-term health care facility, or hospital for mental health care. Medicaid services that can be provided at home or in the community - wherever children/ youth and their families are most comfortable. Allowable Service Combinations: Respite Children and Family Treatments and Support Services (CFTSS) Other Licensed Practitioners (OLP) Community Psychiatric Support and Treatment (CPST) Psychosocial Rehabilitation (PSR) Family Peer Support (FPS) Youth Peer Support Services (YPSS) 11
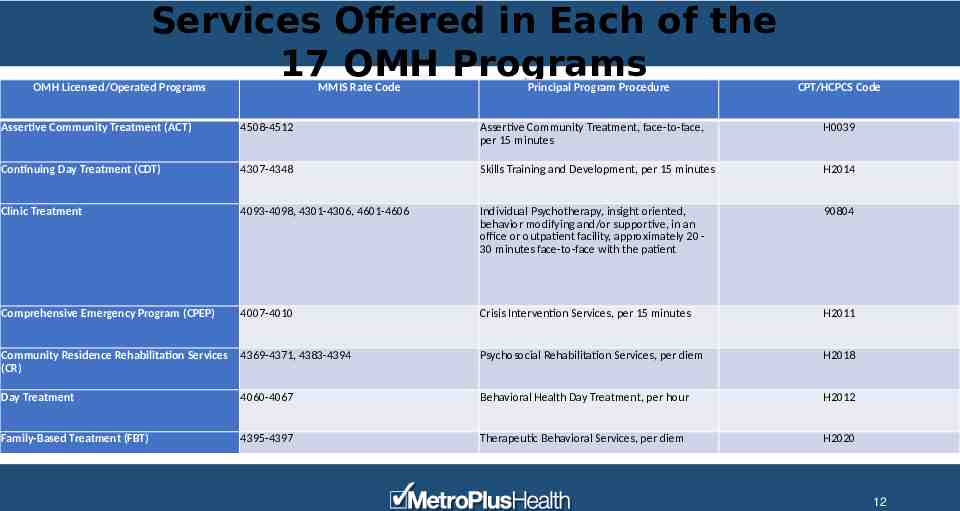
Services Offered in Each of the 17 OMH Programs OMH Licensed/Operated Programs MMIS Rate Code Principal Program Procedure CPT/HCPCS Code Assertive Community Treatment (ACT) 4508-4512 Assertive Community Treatment, face-to-face, per 15 minutes H0039 Continuing Day Treatment (CDT) 4307-4348 Skills Training and Development, per 15 minutes H2014 Clinic Treatment 4093-4098, 4301-4306, 4601-4606 Individual Psychotherapy, insight oriented, behavior modifying and/or supportive, in an office or outpatient facility, approximately 20 30 minutes face-to-face with the patient 90804 Comprehensive Emergency Program (CPEP) 4007-4010 Crisis Intervention Services, per 15 minutes H2011 Community Residence Rehabilitation Services (CR) 4369-4371, 4383-4394 Psychosocial Rehabilitation Services, per diem H2018 Day Treatment 4060-4067 Behavioral Health Day Treatment, per hour H2012 Family-Based Treatment (FBT) 4395-4397 Therapeutic Behavioral Services, per diem H2020 12

Services Offered in Each of the 17 OMH Programs, Cont. OMH Licensed/Operated Programs MMIS Rate Code Principal Program Procedure CPT/HCPCS Code Home and Community Based Waiver Services (HCBWS) 4650-4670 Case Management, per month T2022 Intensive Case Management (ICM) Supportive Case Management (SCM) Blended Case Management (BCM) 5200, 5203-5206, 5251-5259 Targeted Case Management, each 15 minutes T1017 Intensive Psychiatric Rehabilitation Services (IPRT) 4364-4368 Psychosocial Rehabilitation Services, per 15 minutes H2017 Partial Hospitalization (PH) 4349-4363 MH Partial Hospitalization Treatment, Less than 24 Hours H0035 Pre-Paid Mental Health Plan (PMHP) 2340 MH Service Plan Development by Non-Physician H0032 13

Services Offered in Each of the 17 OMH Programs, Cont. OMH Licensed/Operated Programs MMIS Rate Code Principal Program Procedure CPT/HCPCS Code Personalized Recovery Oriented Services (PROS) - Clinic Treatment Component 4525 Pharmacologic management, including prescription, use, and review of medication with no more than minimal medical psychotherapy 90862 Personalized Recovery Oriented Services (PROS) - Community Rehabilitation and Support/ Base Component 4520-4524 Comprehensive Community Support Services, per diem H2016 Personalized Recovery Oriented Services (PROS) - Intensive Rehabilitation Component 4526, 4528 Therapeutic Behavioral Services, per 15 minutes H2019 Personalized Recovery Oriented Services (PROS) - Ongoing Rehabilitation Support Component 4527, 4529 Supported Employment, per diem H2024 Residential Treatment Facility (RTF) 1212, 1222-1225 Health and Behavior Assessment/Intervention, each 15 minutes 96150 14

Helpful References Links for Billing Practices Useful links below: harp-mainstream-billing-manual.pdf (ny.gov) harp-mainstream-billing-manual.pdf (ctacny.org) https://www.health.ny.gov/health care/medicaid/redesign/behavioral health/children/billing m anual.htm# bookmark34 What Do You Need to Know (ny.gov)/ Office of Mental Health (OMH) Clinic Rates Codes (ny.gov) https://omh.ny.gov/omhweb/bho/docs/childrens discussion qa.pdf/ https://omh.ny.gov/omhweb/bho/docs/hcbs cftss services.pdf/ Childrens HCBS Brochure (ny.gov) https://omh.ny.gov/omhweb/bho/docs/hcbs cftss services.pdf/ Childrens HCBS Brochure (ny.gov) 15

Helpful Hints: Claims Service Center Our Claims Service Center will be available to support, the Provider Customer Service Center with complex claim related inquiries. This occurs via a warm transfer into the Claims Service Center to a qualified Service Representative Please have your claim number, member information, date of service in question and the total charges of claim, for faster service. If the Claims Service Representative instructs you to submit additional documentation by use of our internal fax queue or you are following up on the status of a previously submitted facsimile, please ensure to have the date of submission and, the fax number that the item (s) was sent from. This enables the rep to expedite the retrieval of your documentation for follow up and/or resolution. The CSR will be able to assist with three (3) claims per call. If you have more than 3, please submit via our provider portal or the Claim Reconsideration address, noted on prior slides. 16

Submitting Claim Inquiries Via the Portal If you are not registered to access our Provider Portal and are a participating provider, please visit www.MetroPlus.org Check the status of submitted claims 17

Claim Reconsideration/Appeal If you disagree with a claim payment determination, you have the right to appeal. You must explain the reason for the appeal and include all pertinent information as well as a copy of the original claim. Claims must be submitted in writing within 45 calendar days of the date of the original check or denial notification. ** Only Non-participating providers have the right to appeal for the Medicare line of business In writing: MetroPlus Health Plan P.O. Box 830480 Birmingham, AL 35283-0480 By Certified Mail: 50 Water Street, 7th Floor New York, NY 10004 By phone: 800-303-9626 By fax: 212-908-8789 Medical By fax: 212-908-3314 Behavioral Health (BH) 18

Provider Services Is Here to Help You Behavioral Health Provider Service Representatives are assigned by region and serve as a direct liaison between network providers and MetroPlusHealth. They can be reached at: [email protected] Region: Brooklyn/ Staten Island Marya Abbas, BH Provider Service Representative Mobile: 347-852-4446 Email: [email protected] Relationship Manager: Sheila Charles Mobile: 646-296-4768 Office: 212-908-8469 Region: Manhattan Tina Amechand, BH Provider Service Representative Mobile: 347-640-2525 Email: [email protected] Relationship Manager: Kenya McCall Mobile: 917-567-1305 Office: 212-908-8681

Provider Services Is Here to Help You, Cont. Region: Bronx/Westchester Madeline Franklin-Herlihy, BH Provider Service Representative Mobile: 917-242-0980 Email: [email protected] Relationship Manager: April Fowler Mobile: 347-446-5050 Office: 212-908-3724 Region: Queens/Long Island Alexis Medina, BH Provider Service Representative Mobile: 646-734-8811 Email: [email protected] Relationship Manager: Reginald LeGagneur Mobile:347-996-6638 Office: 212-908-8805