SIGNAL TRANSDUCTION BY ADRENERGIC AND CHOLINERGIC RECEPTORS
47 Slides1.52 MB
SIGNAL TRANSDUCTION BY ADRENERGIC AND CHOLINERGIC RECEPTORS Andy Catling Ph.D. Department of Pharmacology Room 5238 [email protected] 568-4740
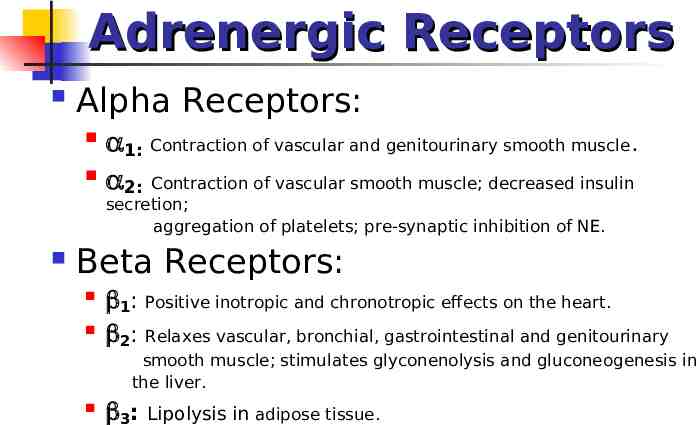
Adrenergic Receptors Alpha Receptors: 1: Contraction of vascular and genitourinary smooth muscle. 2: Contraction of vascular smooth muscle; decreased insulin secretion; aggregation of platelets; pre-synaptic inhibition of NE. Beta Receptors: 1: Positive inotropic and chronotropic effects on the heart. 2: Relaxes vascular, bronchial, gastrointestinal and genitourinary smooth muscle; stimulates glyconenolysis and gluconeogenesis in the liver. 3: Lipolysis in adipose tissue.
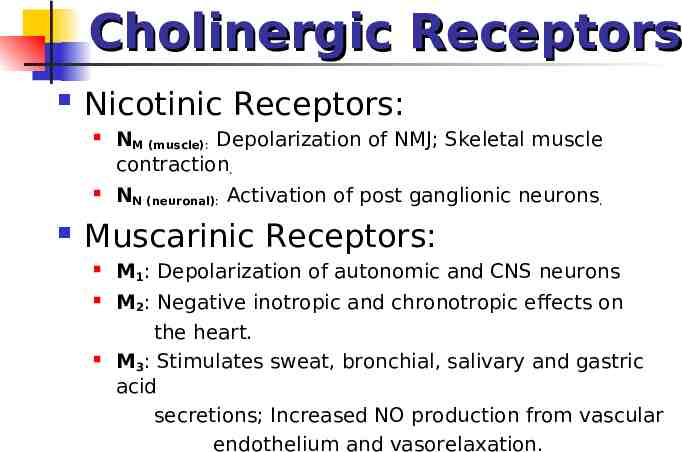
Cholinergic Receptors Nicotinic Receptors: NM (muscle): Depolarization of NMJ; Skeletal muscle contraction. NN (neuronal): Activation of post ganglionic neurons. Muscarinic Receptors: M1: Depolarization of autonomic and CNS neurons M2: Negative inotropic and chronotropic effects on the heart. M3: Stimulates sweat, bronchial, salivary and gastric acid secretions; Increased NO production from vascular endothelium and vasorelaxation.
How does this work? Different receptors can have reinforcing or opposing functions: e.g. 1 adrenergic receptors stimulate contraction of vascular smooth muscle whereas 2 adrenergic and muscarinic M3 receptors both cause relaxation. e.g. 1 adrenergic receptors stimulate contraction of heart muscle, whereas muscarinic M2 receptors inhibit myocardial contraction. Goal of these lectures: begin to understand the signal transduction mechanisms by which specificity is established. Note that this is still a work-in-progress: the human body is complex (!) and there are both gaps in our knowledge and exceptions to general rules
Components of Signal Transduction Signal transduction within cells is accomplished by combinations of: 1st Messenger (extracellular signals e.g. epinephrine, acetylcholine) Receptor Effectors (e.g. adenylyl cyclase, phospholipases, kinases, ion channels etc) 2nd messengers (cAMP, cGMP, inositol triphosphate, diacylgycerol, Ca2 etc) Downstream effectors required for specific functional outputs (e.g. muscle contraction, secretion)
How does this work? Specificity results from: Differential expression and localization (junctional vs extra junctional) of receptors Different receptors couple to different signal transducers Signal transducers/2nd messengers couple to different effectors in different tissues Integration of reinforcing and antagonistic signals
Adrenergic Receptors receptors differ in their location and sensitivity to Epinephrine and Norepinephrine (simplified!): 1 Myocardium E NE 2 Smooth muscle E (essentially no affinity for NE) 3 Adipose tissue NE E i.e. tissue response to agonist is governed by expression of receptor subtypes and ligand present All three adrenergic receptors function through a major class of signal transducer: G-proteins G-proteins couple adrenergic receptors to adenylyl cyclase: agonists increase intracellular cyclic AMP levels and protein kinase A activity, which in turn regulate downstream effectors
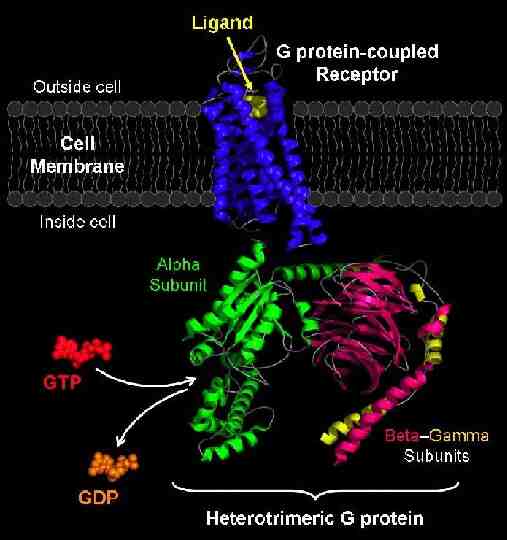
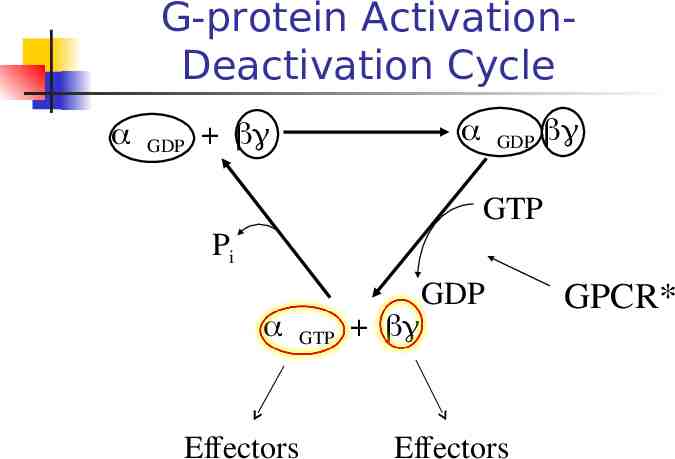
G-protein ActivationDeactivation Cycle GDP GDP GTP Pi GTP Effectors GDP Effectors GPCR*
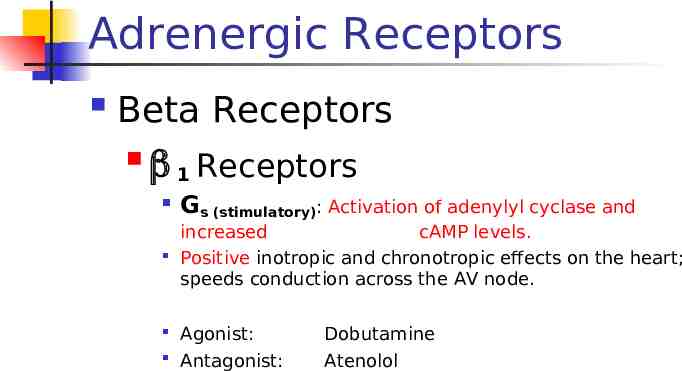
Adrenergic Receptors Beta Receptors 1 Receptors Gs (stimulatory): Activation of adenylyl cyclase and increased cAMP levels. Positive inotropic and chronotropic effects on the heart; speeds conduction across the AV node. Agonist: Antagonist: Dobutamine Atenolol
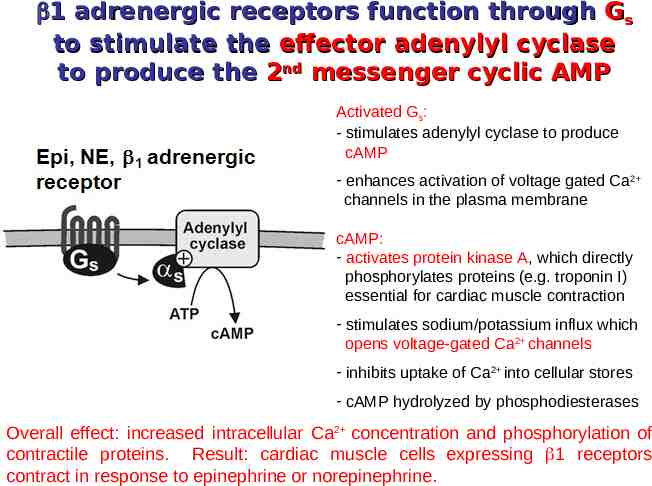
1 adrenergic receptors function through Gs to stimulate the effector adenylyl cyclase to produce the 2nd messenger cyclic AMP Activated Gs: - stimulates adenylyl cyclase to produce cAMP - enhances activation of voltage gated Ca2 channels in the plasma membrane cAMP: - activates protein kinase A, which directly phosphorylates proteins (e.g. troponin I) essential for cardiac muscle contraction - stimulates sodium/potassium influx which opens voltage-gated Ca2 channels - inhibits uptake of Ca2 into cellular stores - cAMP hydrolyzed by phosphodiesterases Overall effect: increased intracellular Ca2 concentration and phosphorylation of contractile proteins. Result: cardiac muscle cells expressing 1 receptors contract in response to epinephrine or norepinephrine.
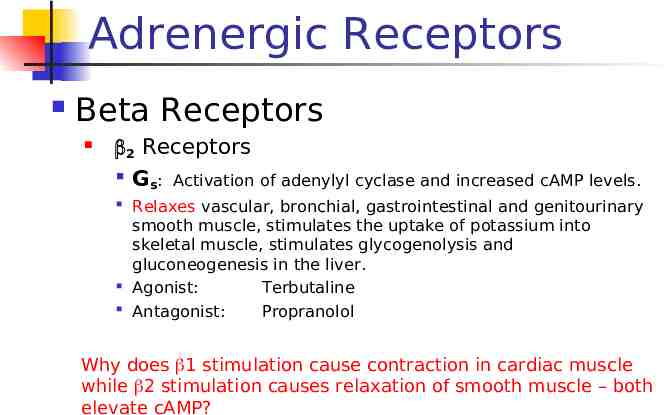
Adrenergic Receptors Beta Receptors 2 Receptors Gs: Activation of adenylyl cyclase and increased cAMP levels. Relaxes vascular, bronchial, gastrointestinal and genitourinary smooth muscle, stimulates the uptake of potassium into skeletal muscle, stimulates glycogenolysis and gluconeogenesis in the liver. Agonist: Terbutaline Antagonist: Propranolol Why does 1 stimulation cause contraction in cardiac muscle while 2 stimulation causes relaxation of smooth muscle – both elevate cAMP?
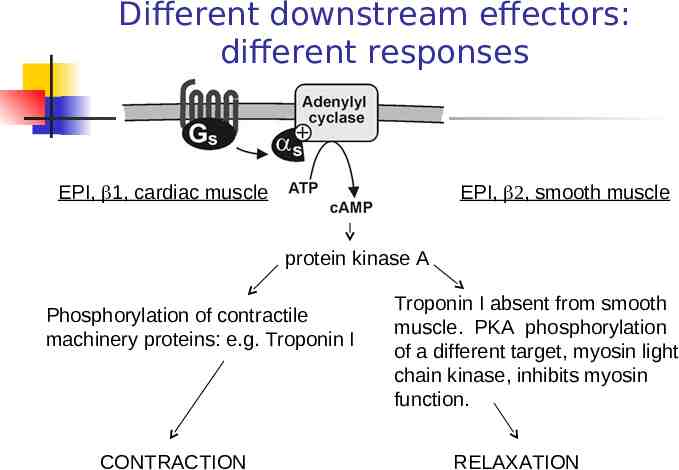
Different downstream effectors: different responses EPI, 1, cardiac muscle EPI, , smooth muscle protein kinase A Phosphorylation of contractile machinery proteins: e.g. Troponin I CONTRACTION Troponin I absent from smooth muscle. PKA phosphorylation of a different target, myosin light chain kinase, inhibits myosin function. RELAXATION
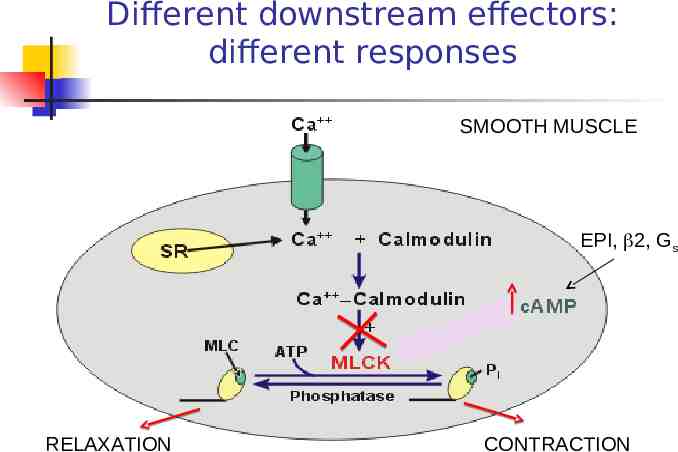
Different downstream effectors: different responses SMOOTH MUSCLE EPI, 2, Gs RELAXATION CONTRACTION
Adrenergic Receptors Beta Receptors 3 Receptors Activate Gs protein, stimulates adenylate cyclase and increases cAMP levels. cAMP activates PKA which stimulates the lipase activity i.e. another context-specific effector Adipose tissue: Lipolysis.
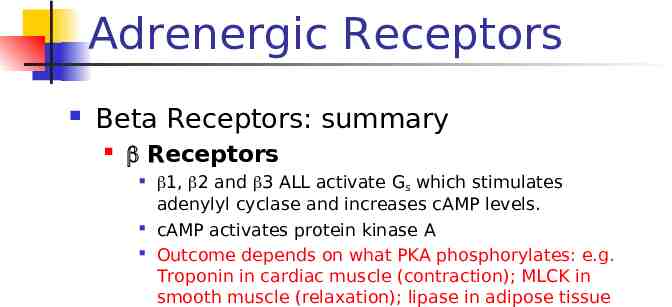
Adrenergic Receptors Beta Receptors: summary Receptors 1, 2 and 3 ALL activate Gs which stimulates adenylyl cyclase and increases cAMP levels. cAMP activates protein kinase A Outcome depends on what PKA phosphorylates: e.g. Troponin in cardiac muscle (contraction); MLCK in smooth muscle (relaxation); lipase in adipose tissue
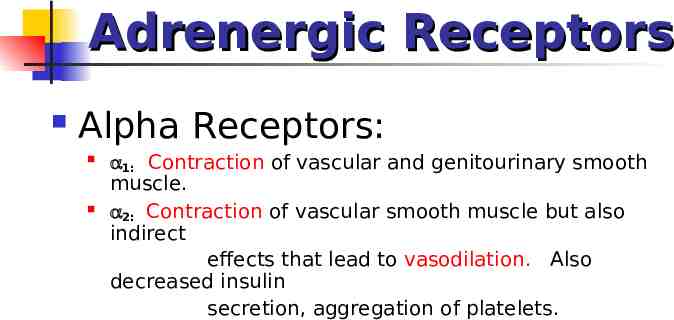
Adrenergic Receptors Alpha Receptors: 1: Contraction of vascular and genitourinary smooth muscle. 2: Contraction of vascular smooth muscle but also indirect effects that lead to vasodilation. Also decreased insulin secretion, aggregation of platelets.
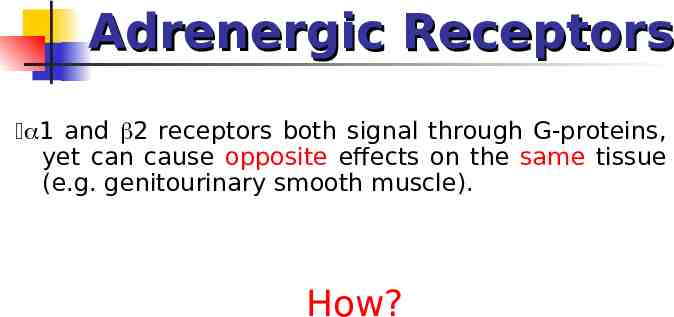
Adrenergic Receptors 1 and 2 receptors both signal through G-proteins, yet can cause opposite effects on the same tissue (e.g. genitourinary smooth muscle). How?
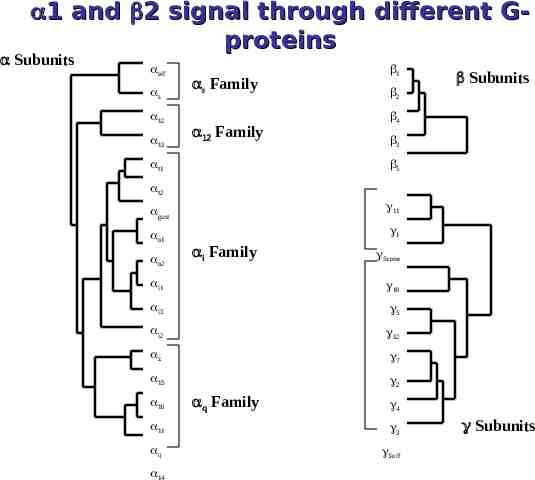
1 and 2 signal through different Gproteins Subunits olf s 12 13 s Family Family t1 1 Subunits 2 4 3 5 t2 gust 11 o1 1 o2 i Family Scone i1 10 i3 5 i2 12 z 7 15 2 16 q Family 4 11 3 q Solf 14 Subunits
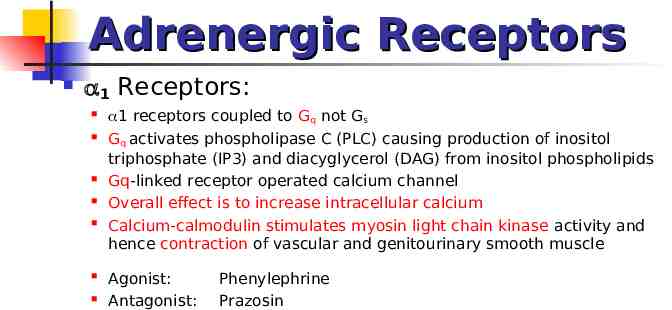
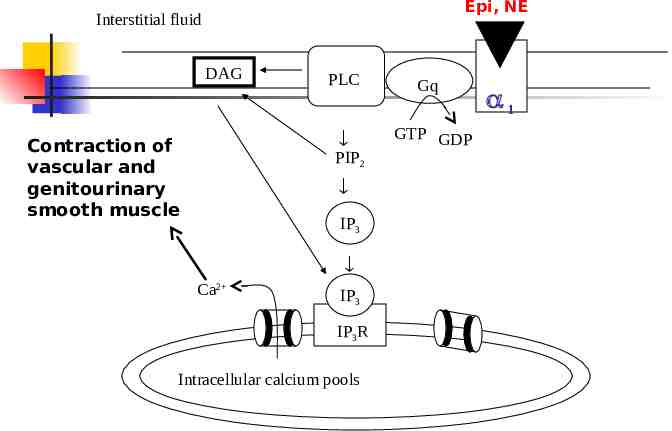
Adrenergic Receptors 1 Receptors: 1 receptors coupled to Gq not Gs Gq activates phospholipase C (PLC) causing production of inositol triphosphate (IP3) and diacyglycerol (DAG) from inositol phospholipids Gq-linked receptor operated calcium channel Overall effect is to increase intracellular calcium Calcium-calmodulin stimulates myosin light chain kinase activity and hence contraction of vascular and genitourinary smooth muscle Agonist: Antagonist: Phenylephrine Prazosin
Epi, NE Interstitial fluid DAG Contraction of vascular and genitourinary smooth muscle PLC Gq GTP GDP PIP2 IP3 Ca2 IP3 IP3R Intracellular calcium pools 1
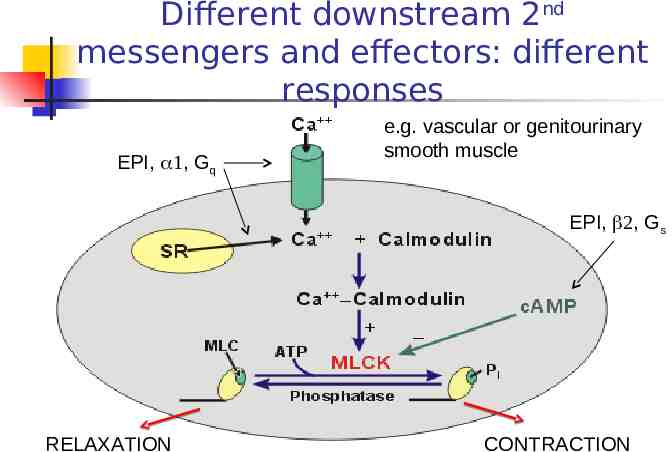
Different downstream 2nd messengers and effectors: different responses EPI, , Gq e.g. vascular or genitourinary smooth muscle EPI, , Gs RELAXATION CONTRACTION
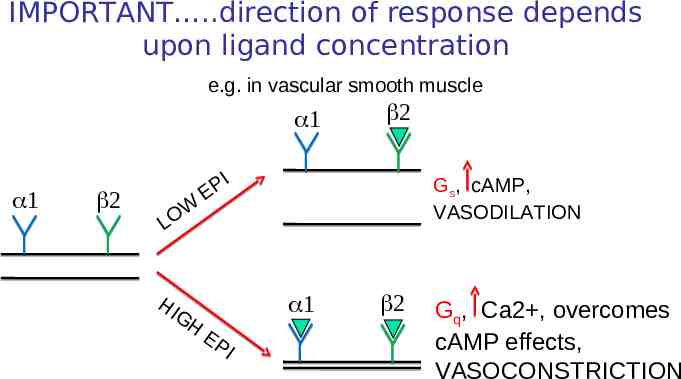
IMPORTANT .direction of response depends upon ligand concentration e.g. in vascular smooth muscle W O L HI GH I P E Gs, cAMP, VASODILATION EP I Gq, Ca2 , overcomes cAMP effects, VASOCONSTRICTION
Adrenergic Receptors adrenergic receptors on vascular smooth muscle cause contraction How?
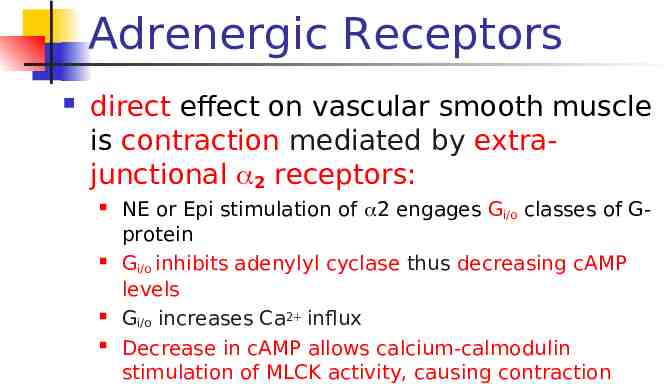
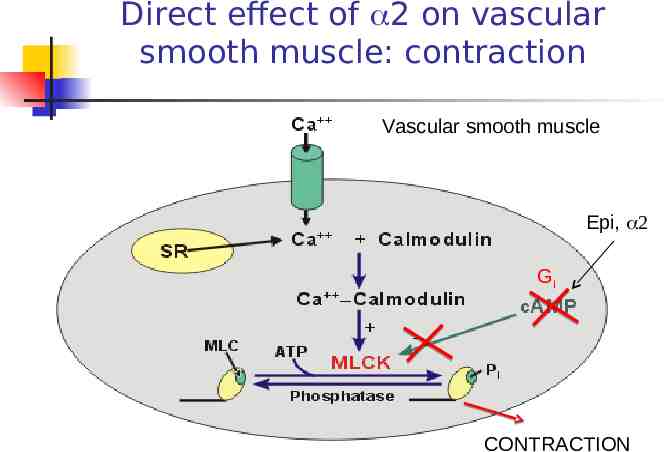
Adrenergic Receptors direct effect on vascular smooth muscle is contraction mediated by extrajunctional 2 receptors: NE or Epi stimulation of 2 engages Gi/o classes of Gprotein Gi/o inhibits adenylyl cyclase thus decreasing cAMP levels Gi/o increases Ca2 influx Decrease in cAMP allows calcium-calmodulin stimulation of MLCK activity, causing contraction
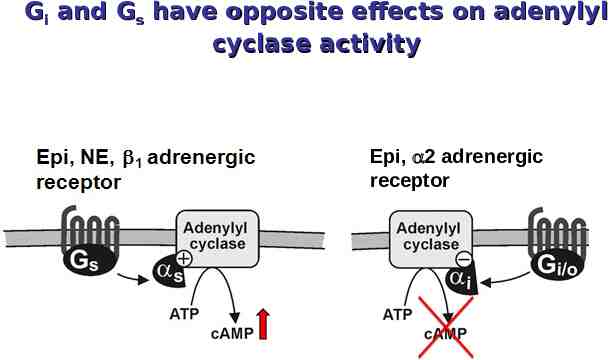
Gi and Gs have opposite effects on adenylyl cyclase activity Epi, 2 adrenergic receptor
Direct effect of 2 on vascular smooth muscle: contraction Vascular smooth muscle Epi, Gi CONTRACTION
Adrenergic Receptors BUT adrenergic vasodilationon receptors How? also can cause
Indirect effect of 2 on vascular smooth muscle: relaxation and vasodilation Presynaptic Receptors (Autoreceptors )
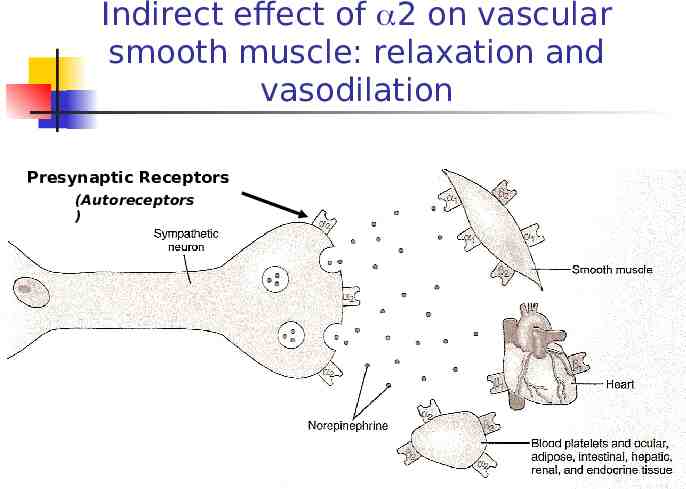
Adrenergic Receptors Pre-synaptic 2 receptors: indirectly cause vasodilation stimulation of pre-synaptic 2 receptors by NE or EPI inhibits release of NE at the synapse NE concentration in the adrenergic synapse is reduced decreasing stimulation of post-synaptic 1 receptors Less post-synaptic 1/Gq activation, translates into less calcium-calmodulin stimulation of MLCK Relaxation
Cholinergic Receptors Muscarinic Receptors: M1: Depolarization of autonomic and CNS neurons M2: Negative inotropic and chronotropic effect on the heart. M3: Smooth muscle contraction with ONE EXCEPTION: cause vascular smooth muscle relaxation and vasodilation; Glandular secretion Also M4 and M5. Nicotinic Receptors: NM (muscle): Depolarization of NMJ; Skeletal muscle contraction . NN (neuronal): Activation of post ganglionic neurons .
Multiple acetylcholine-mediated effects: how? Different subtypes of cholinergic receptors in different tissues.
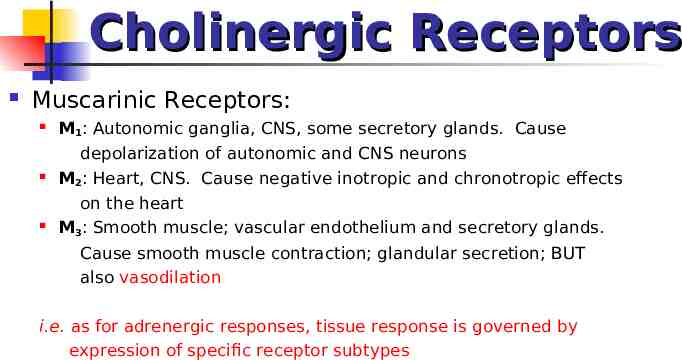
Cholinergic Receptors Muscarinic Receptors: M1: Autonomic ganglia, CNS, some secretory glands. Cause depolarization of autonomic and CNS neurons M2: Heart, CNS. Cause negative inotropic and chronotropic effects on the heart M3: Smooth muscle; vascular endothelium and secretory glands. Cause smooth muscle contraction; glandular secretion; BUT also vasodilation i.e. as for adrenergic responses, tissue response is governed by expression of specific receptor subtypes
What accounts for the differences in Acetylcholine-mediated effects? Different subtypes of cholinergic receptors in different tissues. Different receptors are coupled to different Gproteins and hence different effectors.
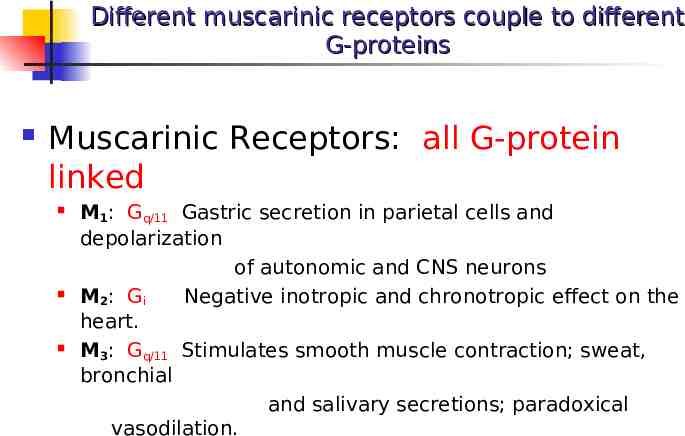
Different muscarinic receptors couple to different G-proteins Muscarinic Receptors: all G-protein linked M1: Gq/11 Gastric secretion in parietal cells and depolarization of autonomic and CNS neurons M2: Gi Negative inotropic and chronotropic effect on the heart. M3: Gq/11 Stimulates smooth muscle contraction; sweat, bronchial and salivary secretions; paradoxical vasodilation.
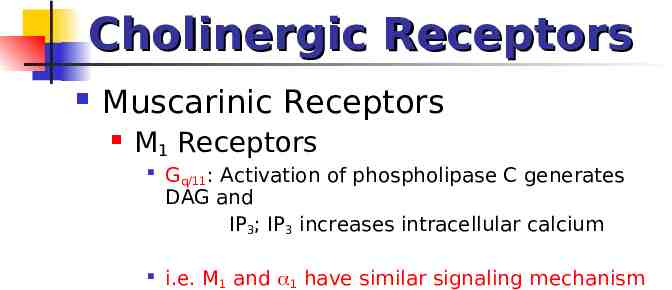
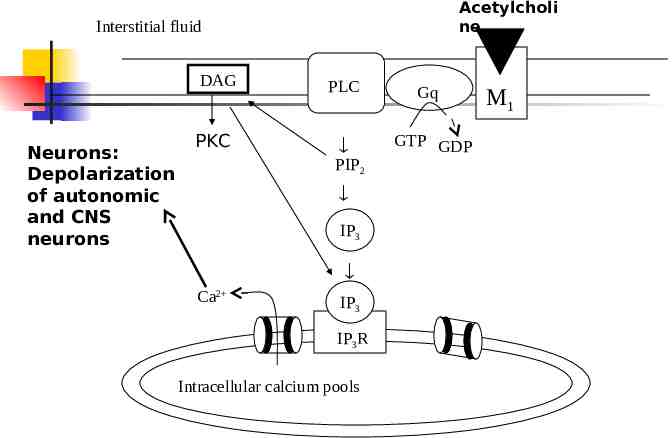
Cholinergic Receptors Muscarinic Receptors M1 Receptors Gq/11: Activation of phospholipase C generates DAG and IP3; IP3 increases intracellular calcium i.e. M1 and 1 have similar signaling mechanism
Acetylcholi ne Interstitial fluid DAG Neurons: Depolarization of autonomic and CNS neurons PKC PLC Gq GTP GDP PIP2 IP3 Ca2 IP3 IP3R Intracellular calcium pools M1
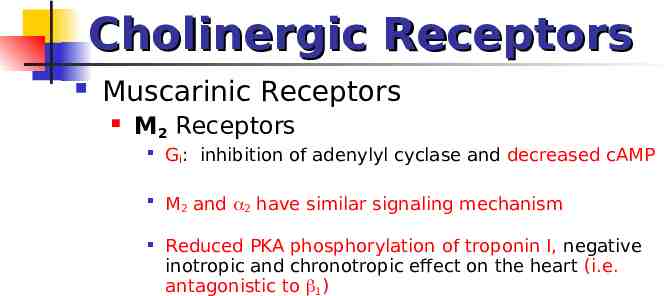
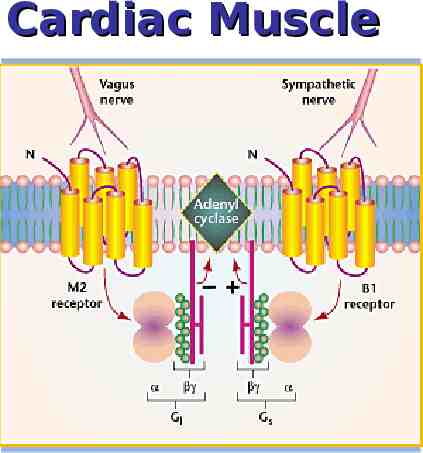
Cholinergic Receptors Muscarinic Receptors M2 Receptors Gi: inhibition of adenylyl cyclase and decreased cAMP M2 and 2 have similar signaling mechanism Reduced PKA phosphorylation of troponin I, negative inotropic and chronotropic effect on the heart (i.e. antagonistic to 1)
Cardiac Muscle
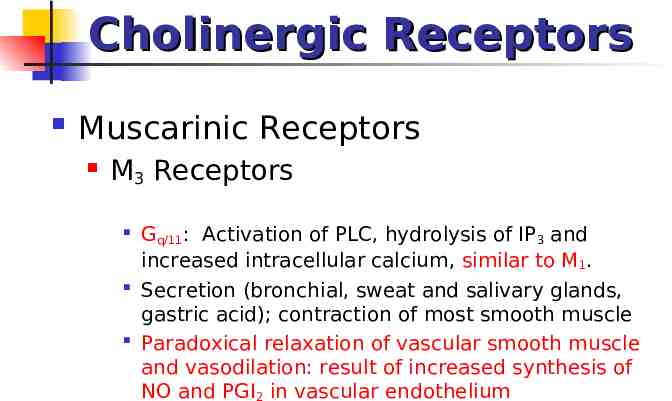
Cholinergic Receptors Muscarinic Receptors M3 Receptors Gq/11: Activation of PLC, hydrolysis of IP3 and increased intracellular calcium, similar to M1. Secretion (bronchial, sweat and salivary glands, gastric acid); contraction of most smooth muscle Paradoxical relaxation of vascular smooth muscle and vasodilation: result of increased synthesis of NO and PGI2 in vascular endothelium
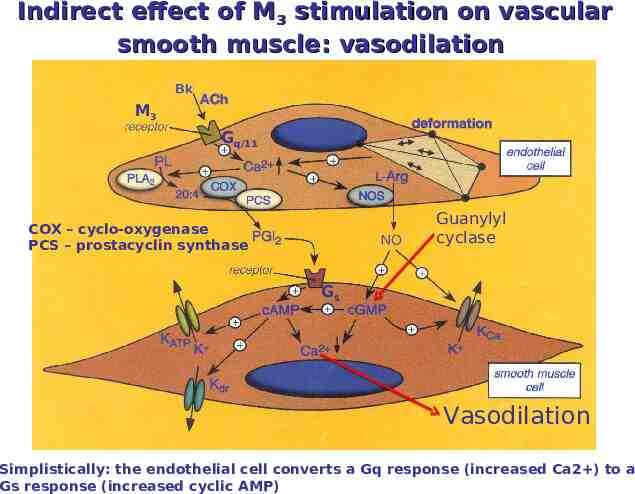
Indirect effect of M3 stimulation on vascular smooth muscle: vasodilation M3 Gq/11 Guanylyl cyclase COX – cyclo-oxygenase PCS – prostacyclin synthase Gs Vasodilation Simplistically: the endothelial cell converts a Gq response (increased Ca2 ) to a Gs response (increased cyclic AMP)
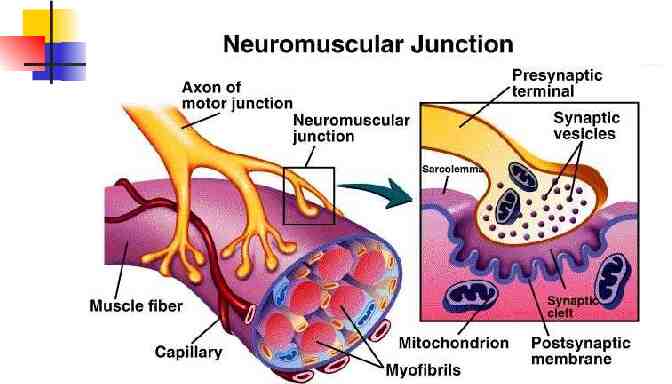
Cholinergic Receptors Nicotinic Receptors: Cation Channels NM: Depolarization of NMJ; Skeletal muscle contraction. NN: Activation of post ganglionic neurons.

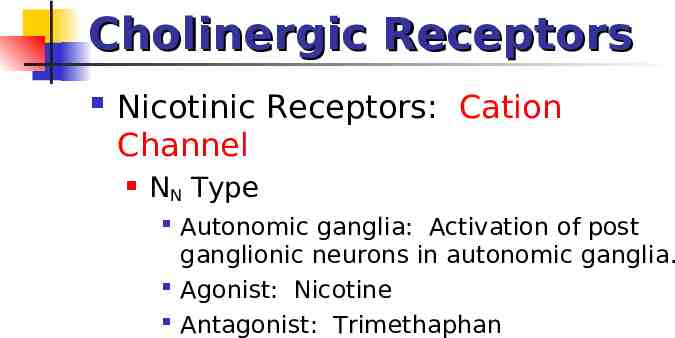
Cholinergic Receptors Nicotinic Receptors: Cation Channel NN Type Autonomic ganglia: Activation of post ganglionic neurons in autonomic ganglia. Agonist: Nicotine Antagonist: Trimethaphan
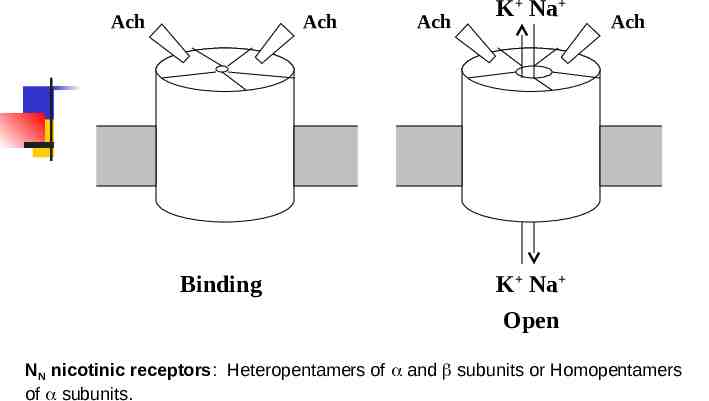
Ach Ach Binding Ach K Na Ach K Na Open NN nicotinic receptors: Heteropentamers of and subunits or Homopentamers of subunits.
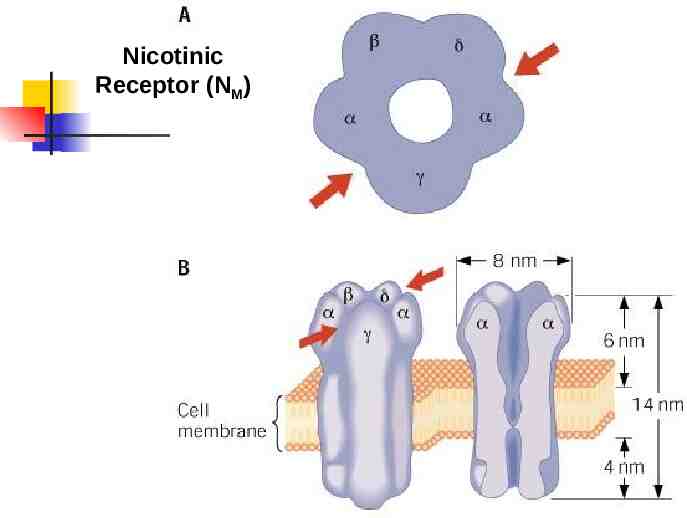
Cholinergic Receptors Nicotinic Receptors: Cation channel NM Type Neuromuscular Junction: Depolarization of NMJ; Skeletal muscle contraction. Heteropentamers of and subunits Agonist: Acetylcholine Antagonist: Tubocurarine
Nicotinic Receptor (NM)