RESPIRATORY COMPROMISE GUIDELINES
10 Slides1.05 MB
RESPIRATORY COMPROMISE GUIDELINES
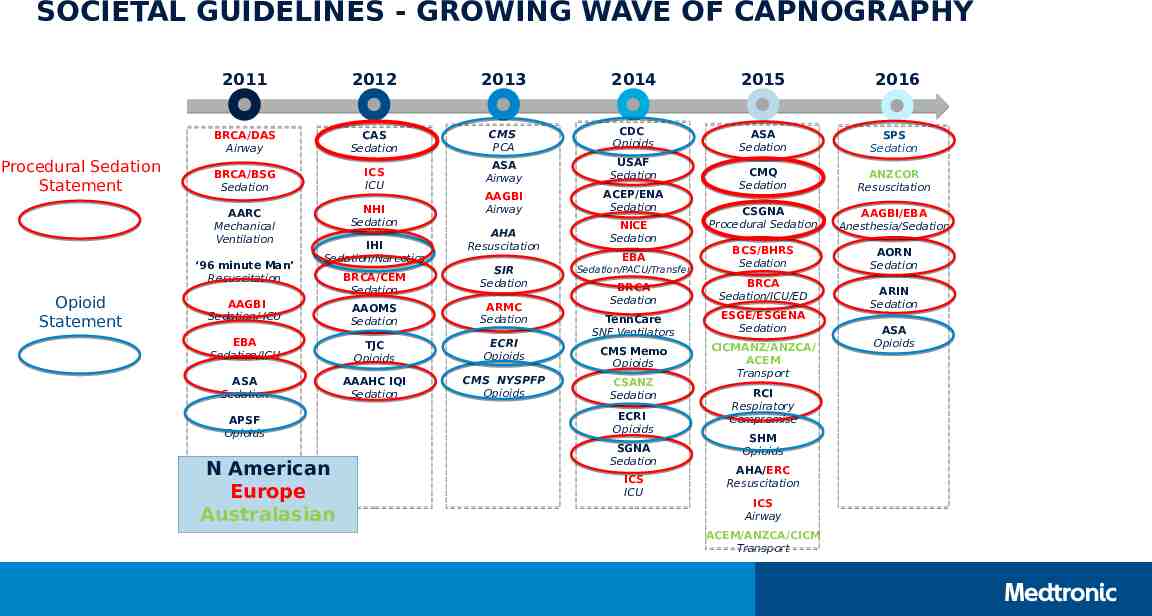
SOCIETAL GUIDELINES - GROWING WAVE OF CAPNOGRAPHY Procedural Sedation Statement 2011 2012 2013 2014 2015 2016 BRCA/DAS Airway CAS Sedation CMS PCA CDC Opioids ASA Sedation SPS Sedation BRCA/BSG Sedation ICS ICU ASA Airway USAF Sedation NHI Sedation ACEP/ENA Sedation ANZCOR Resuscitation AARC Mechanical Ventilation AAGBI Airway CMQ Sedation CSGNA Procedural Sedation AAGBI/EBA Anesthesia/Sedation BCS/BHRS Sedation AORN Sedation ‘96 minute Man’ Resuscitation Opioid Statement IHI Sedation/Narcotics AAGBI Sedation/ ICU BRCA/CEM Sedation AHA Resuscitation SIR Sedation AAOMS Sedation ARMC Sedation EBA Sedation/ICU TJC Opioids ECRI Opioids ASA Sedation AAAHC IQI Sedation CMS NYSPFP Opioids APSF Opioids N American Europe Australasian NICE Sedation EBA Sedation/PACU/Transfer BRCA Sedation BRCA Sedation/ICU/ED TennCare SNF Ventilators ESGE/ESGENA Sedation CMS Memo Opioids CICMANZ/ANZCA/ ACEM Transport CSANZ Sedation ECRI Opioids SGNA Sedation ICS ICU RCI Respiratory Compromise SHM Opioids AHA/ERC Resuscitation ICS Airway ACEM/ANZCA/CICM Transport ARIN Sedation ASA Opioids
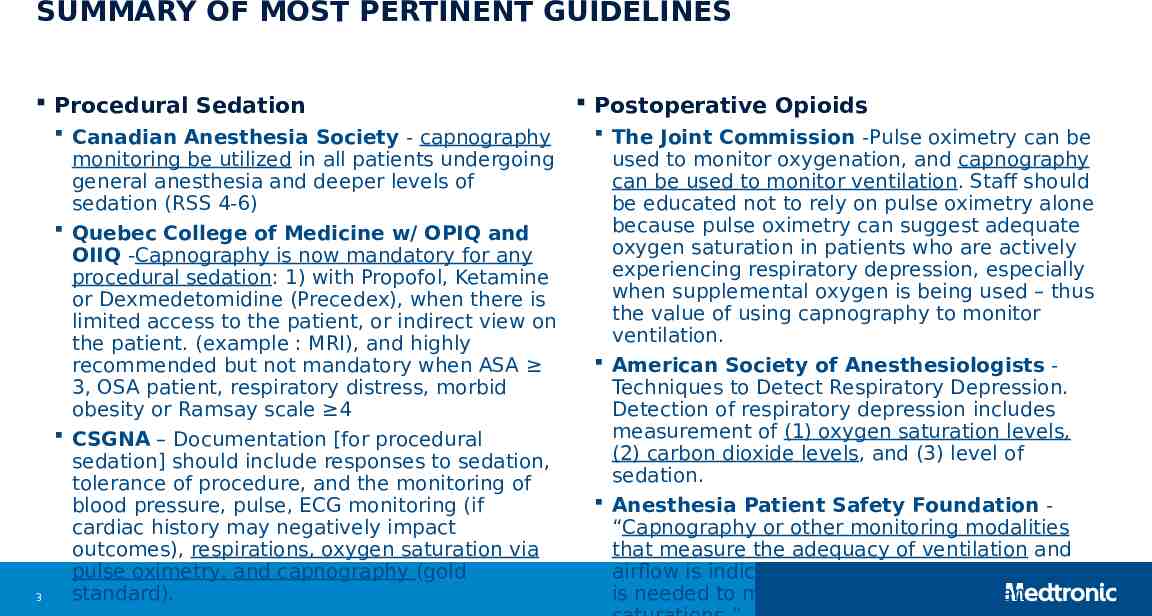
SUMMARY OF MOST PERTINENT GUIDELINES Procedural Sedation 3 Canadian Anesthesia Society - capnography monitoring be utilized in all patients undergoing general anesthesia and deeper levels of sedation (RSS 4-6) Quebec College of Medicine w/ OPIQ and OIIQ -Capnography is now mandatory for any procedural sedation: 1) with Propofol, Ketamine or Dexmedetomidine (Precedex), when there is limited access to the patient, or indirect view on the patient. (example : MRI), and highly recommended but not mandatory when ASA 3, OSA patient, respiratory distress, morbid obesity or Ramsay scale 4 CSGNA – Documentation [for procedural sedation] should include responses to sedation, tolerance of procedure, and the monitoring of blood pressure, pulse, ECG monitoring (if cardiac history may negatively impact outcomes), respirations, oxygen saturation via pulse oximetry, and capnography (gold standard). Postoperative Opioids The Joint Commission -Pulse oximetry can be used to monitor oxygenation, and capnography can be used to monitor ventilation. Staff should be educated not to rely on pulse oximetry alone because pulse oximetry can suggest adequate oxygen saturation in patients who are actively experiencing respiratory depression, especially when supplemental oxygen is being used – thus the value of using capnography to monitor ventilation. American Society of Anesthesiologists Techniques to Detect Respiratory Depression. Detection of respiratory depression includes measurement of (1) oxygen saturation levels, (2) carbon dioxide levels, and (3) level of sedation. Anesthesia Patient Safety Foundation “Capnography or other monitoring modalities that measure the adequacy of ventilation and airflow is indicated when supplemental oxygen is needed to maintain acceptable oxygen
CANADIAN ANESTHESIA SOCIETY 2012 – Updated Guidelines to the Practice of Anesthesia 1 Update requires capnography during general anesthesia and deeper levels of sedation (RSS 4-6) Definition of ‘Required Monitoring’: Monitors must be in continuous use throughout the administration of all anesthetics Monitoring guidelines for standard patient care apply to all patients receiving anesthesia or intravenous sedation 1. Merchant R, Chartrand D, Dain S, Dobson J, Kurrek M, LeDez K, Morgan P, Shukia R. Guidelines to the Practice of Anesthesia: Revised Edition 2012. Can J Anesth 2012;59:63-102.
LE COLLÈGE DES MÉDECINS DU QUÉBEC, L’ORDRE PROFESSIONNEL DES INHALOHÉRAPEUTES DU QUÉBEC (OPIQ) ET L’ORDRE DES INFIRMIÈRES ET INFIRMIERS DU QUÉBEC (OIIQ) 2015 – LA SÉDATION ANALGÉSIE1 Patient types: Pediatric ( 3 years old) and adult Key points : Capnography is now mandatory for any procedural sedation with: Propofol, Ketamine or Dexmedetomidine (Precedex). Capnography is now mandatory when there is limited access to the patient, or indirect view on the patient. (example : MRI) Capnography is highly recommended but not mandatory when : ASA 3, OSA patient, respiratory distress, morbid obesity or Ramsay scale 4 1 - http://www.cmq.org/publications-pdf/p-1-2015-04-01-fr-sedation-analgesie.pdf Accessed May 23, 2017
CANADIAN SOCIETY OF GASTROENTEROLOGY NURSES AND ASSOCIATES (CSGNA) 2015 - Procedural Sedation: Position Statement for Role of the Registered Nurse Document and monitor the patient receiving procedural sedation according to the institutional policy of where the nurse is employed. Documentation should include responses to sedation, tolerance of procedure, and the monitoring of blood pressure, pulse, ECG monitoring (if cardiac history may negatively impact outcomes), respirations, oxygen saturation via pulse oximetry, and capnography (gold standard). https://colibri-production-app.s3.amazonaws.com/sites/555e068a83781212ec01929d/assets/55f6bec64a2c09a49800ead0/Procedural Sedation position statement and role of the RN April 11 2015.pdf Accessed May 23, 2017
ANESTHESIA PATIENT SAFETY FOUNDATION 2011 – Postoperative Monitoring with Opioid Use “Continuous electronic monitoring of oxygenation and ventilation should be available and considered for all patients and would reduce the likelihood of unrecognized clinically significant opioid-induced depression of ventilation in the postoperative period.”1 “Capnography or other monitoring modalities that measure the adequacy of ventilation and airflow is indicated when supplemental oxygen is needed to maintain acceptable oxygen saturations.”1 “APSF is aware of hospital system experiences that support the effectiveness of alternative continuous respiratory monitoring technologies, such as capnography, in lieu of pulse oximetry.”1 1. Essential Monitoring Strategies to Detect Clinically Significant Drug- Induced Respiratory Depression in the Postoperative Period. Prepared by Stoelting, R. and Overdyk, F. http://www.apsf.org/announcements.php?id 7.
THE JOINT COMMISSION 2012 – Safe use of opioids in hospitals1 “Create and implement policies and procedures for the ongoing clinical monitoring of patients receiving opioid therapy by performing serial assessments of the quality and adequacy of respiration and the depth of sedation.” “In addition to monitoring respiration and sedation, pulse oximetry can be used to monitor oxygenation, and capnography can be used to monitor ventilation. Staff should be educated not to rely on pulse oximetry alone because pulse oximetry can suggest adequate oxygen saturation in patients who are actively experiencing respiratory depression, especially when supplemental oxygen is being used – thus the value of using capnography to monitor ventilation.” “When pulse oximetry or capnography is used, it should be used continuously rather than intermittently.” 1. Joint Commission Sentinel Event Alert: Issue #49, pp1-4, August 8, 2012. (Available at www.jointcommission.org).
AMERICAN SOCIETY OF ANESTHESIOLOGISTS 2016 - Practice Guidelines for the Prevention, Detection, and Management of Respiratory Depression Associated with Neuraxial Opioid Administration For these guidelines, respiratory depression may be indicated by (1) reduced respiratory rate (e.g., to less than 10 breaths/min), (2) reduced oxygen saturation (e.g., arterial oxygen saturation less than 90%), or (3) hypercapnia/hypercarbia (e.g., arterial carbon dioxide tension more than 50 mmHg). These guidelines include specific recommendations in four areas Detection of respiratory depression through monitoring for adequacy of ventilation, oxygenation, and level of consciousness. Monitoring for Respiratory Depression - Respiratory depression monitoring includes (1) consideration of techniques to detect respiratory depression and (2) perioperative monitoring for respiratory depression. Techniques to Detect Respiratory Depression. Detection of respiratory depression includes measurement of (1) oxygen saturation levels, (2) carbon dioxide levels, and (3) level of sedation. Literature Findings Although the literature is insufficient to evaluate carbon dioxide monitoring for neuraxial opioids, literature reporting end-tidal carbon dioxide monitoring for parenteral opioids suggest that such monitoring is effective in detecting hypercapnia or hypercarbia. Practice Guidelines for the Prevention, Detection, and Management of Respiratory Depression Associated with Neuraxial Opioid Administration An Updated Report by the American Society of Anesthesiologists Task Force on Neuraxial Opioids and the American Society of Regional Anesthesia and Pain Medicine Anesthesiology 2016; 124(3):535-552 www.asahq.org
HEART AND STROKE FOUNDATION OF CANADA3 November 2010 – Guidelines for CPR and ECC1 (updated in 2015) Continuous quantitative waveform capnography recommended for intubated adult patients throughout the peri-arrest period Applications now include recommendations for : ET tube placement Monitoring CPR quality Detecting ROSC Recommendations pertinent to both ACLS and PALS Similar guidelines have been adopted by the American Heart Association1, European Resuscitation Council2, Japan ALS Council4, and other countries’ Resuscitation Councils 1 American Heart Association (AHA) Guidelines for Cardiopulmonary Resuscitation (CPR) and Emergency Cardiovascular Care (ECC). Highlights of the 2010 American Heart Association Guidelines for CPR and ECC. 2. European Resuscitation Council Summary of the Main Changes in the Resuscitation Guidelines, ERC Guidelines 2010. 3. Heart and Stroke Foundation of Canada/American Heart Association (AHA) Guidelines for Cardiopulmonary Resuscitation (CPR) and Emergency Cardiovascular Care (ECC). Highlights of the 2010 American Heart Association Guidelines for CPR and ECC. 4. Japan ALS Task Force. Chapter 2, Advanced Life Support and Chapter 3, Pediatric Basic Life Support, Pediatric Advanced Life Support.