POLYTRAUMA NETWORK SITE SERVICES Presented by: Esmeralda Madrigal
22 Slides1.12 MB
POLYTRAUMA NETWORK SITE SERVICES Presented by: Esmeralda Madrigal Stefanie Chin
Our Mission The PSC offers a unique mission to care for recently injured returning active duty service members (ADSM) and veterans. Mission: The PSC is dedicated to providing rehabilitation services that restore physical, intellectual, communicative, psychosocial and vocational skills, and to facilitating the transfer of those skills from the hospital setting to daily life. Such services include, but are not limited to, inpatient rehabilitation, outpatient rehabilitation, emerging consciousness programs, transitional rehabilitation, day programs, and community re-entry programs.

Definition of Polytrauma “Polytrauma” is a new medical term that evolved to describe unique, complex patterns of injuries from OEF/OIF: Complex, multiple injuries occurring as a result of same event Unpredictable patterns including brain injury, amputation, hearing and vision impairments, spinal cord injuries, psychological trauma, and musculoskeletal wounds Individuals with polytrauma require extraordinary level of integration and coordination of medical, rehabilitation, and support services Brain Injury is primary injury that drives care Higher level of acuity due to severity of injuries Simultaneous treatment of multiple injuries Sequence and integrate therapies to meet patient need Coordinate interdisciplinary team effort with expanded team of consultants

VAPAHCS Rehabilitation Programs VAPAHCS has four rehabilitation programs under the Polytrauma System of Care. Polytrauma Rehabilitation Center (PRC) Comprehensive Rehabilitation Center (CRC) Inpatient Acute Rehabilitation, General Rehabilitation Polytrauma Transitional Rehabilitation Program (PTRP) Inpatient Acute Rehabilitation, Brain Injury Residential /Outpatient Day Program Polytrauma Network Site (PNS) Outpatient Clinic

Polytrauma Rehabilitation Center (PRC) Multidisciplinary preadmission review to develop a customized treatment plan 4 clinical pathways-emerging consciousness, sub-acute, acute and short-stay TBI evaluation CARF accredited Provides inpatient acute care for full range of brain injuries and associated injuries

Polytrauma Transitional Rehabilitation Program (PTRP) Post-acute day treatment program for individuals with moderate to severe TBI CARF Accredited Hybrid residential/outpatient program 12 Residential Beds Off-site apartments (Moffett Field)

Polytrauma Network Site (PNS) Outpatient blast injury/TBI evaluative clinic At Palo Alto, we evaluate anyone with a positive TBI screen Manage stable Polytrauma sequelae Proactive follow-up ensuring comprehensive outpatient Polytrauma care in VISN 21 Facilitates Polytrauma education in VISN 21 Provides family support

Nature of Injuries Improvised Explosive Devices (IED) Rocket-propelled Grenades (RPG) Landmines Mortars Hand Grenades Snipers MVA Assaults Falls Any other blows to the head

Many issues following deployment are not visible Ringing in ears- Audiology Blurred vision/light sensitivityEye Clinic Poor memory/concentrationNeuropsychology/Speech Depression/PTSDTrauma Services Back Pain, HeadachesPrimary Care, Neurology and PM&R OIF/OEF Normal Appearance Team Approach
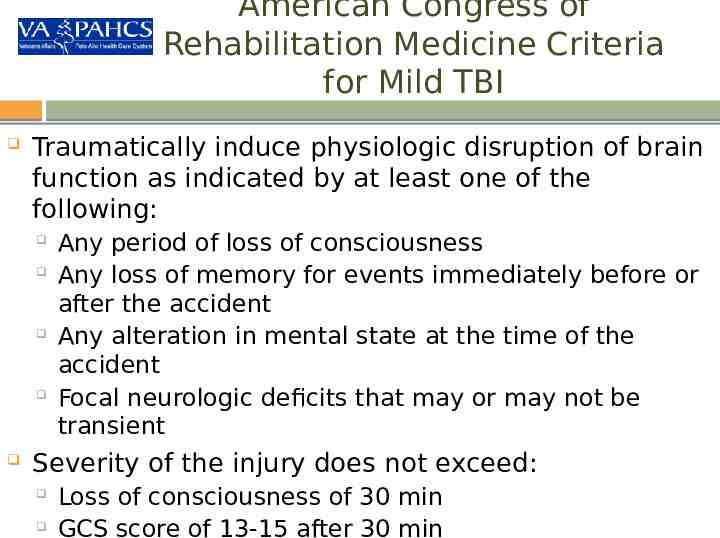
American Congress of Rehabilitation Medicine Criteria for Mild TBI Traumatically induce physiologic disruption of brain function as indicated by at least one of the following: Any period of loss of consciousness Any loss of memory for events immediately before or after the accident Any alteration in mental state at the time of the accident Focal neurologic deficits that may or may not be transient Severity of the injury does not exceed: Loss of consciousness of 30 min GCS score of 13-15 after 30 min
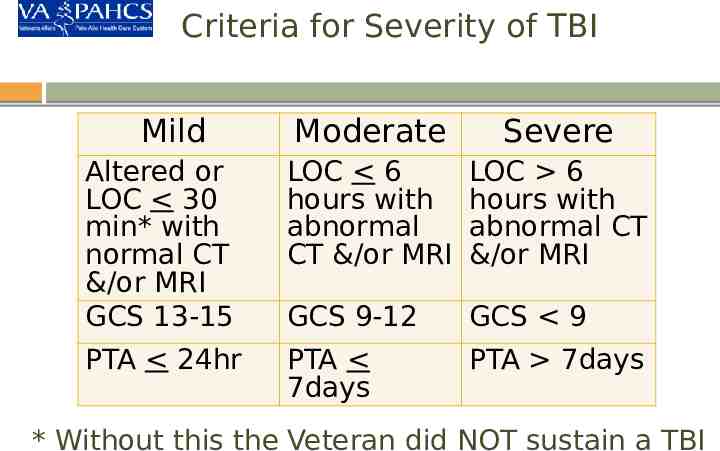
Criteria for Severity of TBI Mild Moderate Severe Altered or LOC 30 min* with normal CT &/or MRI GCS 13-15 LOC 6 hours with abnormal CT &/or MRI LOC 6 hours with abnormal CT &/or MRI GCS 9-12 GCS 9 PTA 24hr PTA 7days PTA 7days * Without this the Veteran did NOT sustain a TBI

PNS Scope of Clinical Services Provide specialized interdisciplinary post-acute rehabilitation services; inpatient and outpatient Continued management of existing and emerging sequelae Manage rehabilitation plan developed at PRC Manage new polytrauma patients in consultation with PRC Identify resources for VA and non-VA care across the VISN Provide proactive clinical and psychosocial case management; continued support for families Provide regular follow-up care, check-ups Coordinate services between VHA, VBA, DOD, private sector (fee-basis)

PNS Patient Demographics VAPAHCS has evaluated approx 1,300 patients for mTBI Consult driven referral system Mostly male, aged 21-38 years old FY 08 to present: TBI dx: 75% PTSD/Mental Health dx: 64.2% MSK/pain dx: 31.3% Variety of psychosocial factors impact functioning Active duty service members and veterans Social Isolation Substance Use and/or abuse

Who is Appropriate for Referral to Polytrauma Outpatient Clinic? OEF/OIF patients who have positive TBI screen: refer for TBI second level evaluation which is a 2 hr appointment Patients with history of TBI and current functional impairments: refer for PNS MD "followup" which is a 1 hr appointment slot Unlike some PNS across the country, VAPAHCS PNS also evaluates non-OEF/OIF patients who have known or suspected TBI PNS MD determines if history is consistent with TBI, and determines if pt has functional impairments that would benefit from PNS interdisciplinary services Only PNS MDs may refer to PNS disciplines (PT, OT, SLP, RT,

PNS Referral Process Referrals and transfers are coordinated by the Social Work case managers and/or nurse case manager In consultation with the PNS physiatrist as needed Referrals can be made by telephone contact if outside the VA or by consultation within the VA The SW will facilitate the enrollment process if needed Tricare authorization needed prior for active duty service members Medical records requested, if available

Specialized Rehabilitation Team PNS teams include: Physiatry, Nursing, Occupational/Physical/Recreational therapy, Speech Language Pathology, Optometry, Social Work and Neuropsychology Interdisciplinary team approach to care Patient/family focused care CARF Accreditation since 2010 Tele Rehabilitation PNS evaluations conducted using V-tel technology

Telehealth Initiative Polytrauma Telehealth TBI Second Level Evaluation and Follow-up Program Provider / Distant Site Patient / Originating Site TBI Specialty Physiatrist Locations: Patient and Telepresenter Locations Community Based Outpatient Clinics' Livermore Modesto Palo Alto Monterey Stockton
Community Re-integration Common goals of veterans/SMs: School Employment PNS team members assist with community re-integration Collaborate with local schools Provide resources for education and employment

Advanced Technology Applications Rapidly evolving devices and technology have great potential for rehabilitation, and are well-received by Veterans Establishing Assistive Technology Labs at 4 Polytrauma Rehabilitation Centers Labs will serve as resource for VA Health Care and provide access to most advanced technology for: Cognitive impairment Sensory impairment (hearing, vision, speech) Computer access Communication devices Wheeled mobility / Seating / Lift systems Home / Vehicle Modification Self care Home Telehealth

PNS Contacts Julianna Brooks, Program Director [email protected] 650 493-5000, ext. 65053 650 444-8029 cell Rose Salerno, RN, CBIST 650 493-5000, ext. 66150 650 380-8223 Esmeralda Madrigal, LMSW, CBIS 650 493-5000, ext. 62768 650 444-8252 cell Stefanie Chin, LMSW 650 493-5000, ext. 69226 650 814-0583 cell

OEF/OIF Contacts Laura Gomez, LCSW – Program Manager 650 493-5000, ext. 60007 Amy Alderman, LMSW 650 493-5000, ext. 66870 Pamela Calimlim, LCSW 650 493-5000, ext. 67203 Raquel Morales, LMSW 650 493-5000, ext. 77629
Thank You! Questions?