Patient Safety Indicators PSI 90 AHRQ Quality Indicators
44 Slides325.83 KB
Patient Safety Indicators PSI 90 AHRQ Quality Indicators evaluate in-hospital complications and adverse events following surgeries, procedures, and childbirth ages 18 years and older Jennifer Piña, BSN, RN, CCDS Clinical Documentation Specialist
Agenda Overview of PSI 90 Identify PSI 90 composite Identify common exclusion criteria for each measure Identify documentation opportunities to accurately reflect the correct PSI’s assigned.
The purpose of the PSI 90 composite measure score PSI-90 is a composite measure that was developed to : Monitor quality performance Used for comparative reporting Improvement quality care at the provider level. Screen for complications or adverse events that patients experience as a result of exposure to the healthcare system.
Patient Safety Indicators? PSIs are a set of measures that screen for complications or adverse events that patients experience inpatient in the hospital. When hospitals report PSIs in their quality data they can carry financial consequences as part of the pay for performance initiatives. PSIs reflect the quality of inpatient care and focus on preventing complications Intended to identify preventable conditions and develop plans for performance improvement. Reflect the safety climate of a hospital by providing a marker of patient safety during the delivery of care. Can be used as a resource for patients when selecting care options, used for providers in allocating resources, and for payers in

Measure Specifications (age 18 years and older) PSI 03 Pressure Ulcer Rate PSI 06 Iatrogenic Pneumothorax Rate PSI 08 In-Hospital Fall with Hip Fracture Rate PSI 09 Perioperative Hemorrhage or Hematoma Rate PSI 10 Post-Operative Acute Kidney Injury Requiring Dialysis Rate PSI 11 Postoperative Respiratory Failure Rate PSI 12 Perioperative Pulmonary Embolism or Deep Vein Thrombosis Rate PSI 13 Postoperative Sepsis Rate PSI 14 Postoperative Wound Dehiscence Rate PSI 15 Unrecognized Accidental Puncture or Laceration Rate
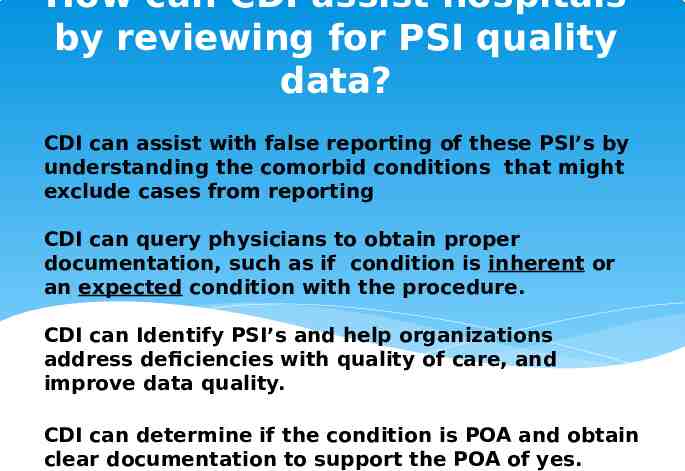
How can CDI assist hospitals by reviewing for PSI quality data? CDI can assist with false reporting of these PSI’s by understanding the comorbid conditions that might exclude cases from reporting CDI can query physicians to obtain proper documentation, such as if condition is inherent or an expected condition with the procedure. CDI can Identify PSI’s and help organizations address deficiencies with quality of care, and improve data quality. CDI can determine if the condition is POA and obtain clear documentation to support the POA of yes.
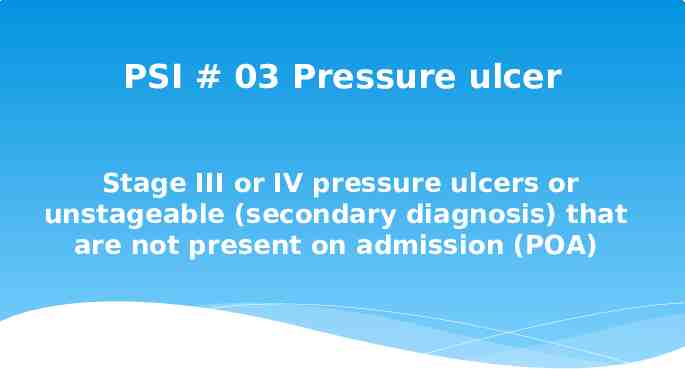
PSI # 03 Pressure ulcer Stage III or IV pressure ulcers or unstageable (secondary diagnosis) that are not present on admission (POA)
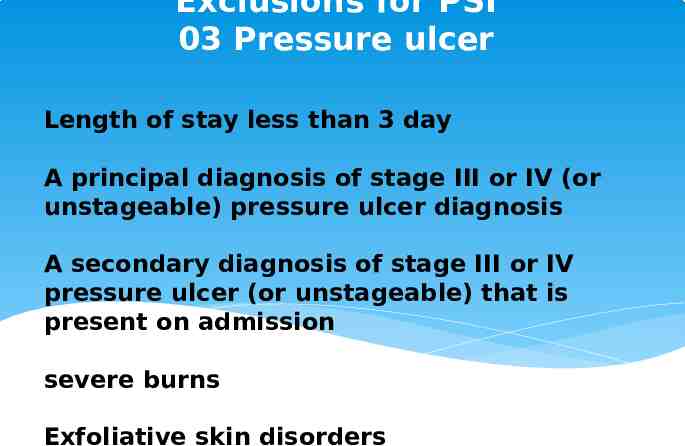
Exclusions for PSI 03 Pressure ulcer Length of stay less than 3 day A principal diagnosis of stage III or IV (or unstageable) pressure ulcer diagnosis A secondary diagnosis of stage III or IV pressure ulcer (or unstageable) that is present on admission severe burns Exfoliative skin disorders
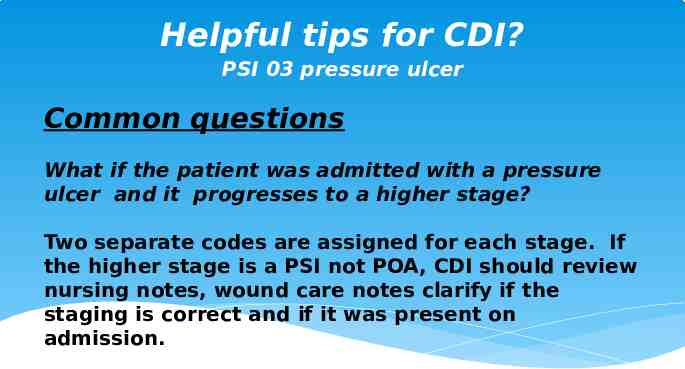
Helpful tips for CDI? PSI 03 pressure ulcer Common questions What if the patient was admitted with a pressure ulcer and it progresses to a higher stage? Two separate codes are assigned for each stage. If the higher stage is a PSI not POA, CDI should review nursing notes, wound care notes clarify if the staging is correct and if it was present on admission.
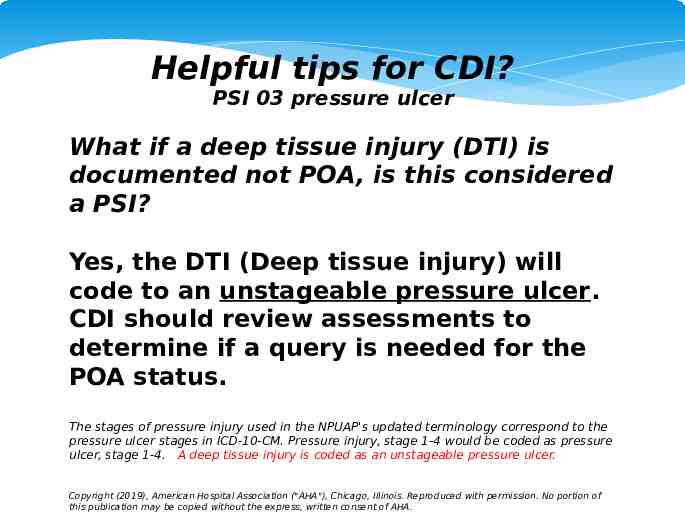
Helpful tips for CDI? PSI 03 pressure ulcer What if a deep tissue injury (DTI) is documented not POA, is this considered a PSI? Yes, the DTI (Deep tissue injury) will code to an unstageable pressure ulcer. CDI should review assessments to determine if a query is needed for the POA status. The stages of pressure injury used in the NPUAP's updated terminology correspond to the pressure ulcer stages in ICD-10-CM. Pressure injury, stage 1-4 would be coded as pressure ulcer, stage 1-4. A deep tissue injury is coded as an unstageable pressure ulcer. Copyright (2019), American Hospital Association ("AHA"), Chicago, Illinois. Reproduced with permission. No portion of this publication may be copied without the express, written consent of AHA.
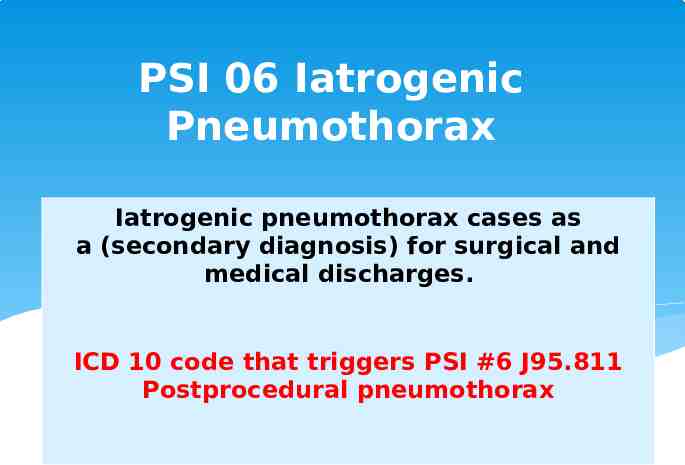
PSI 06 Iatrogenic Pneumothorax Iatrogenic pneumothorax cases as a (secondary diagnosis) for surgical and medical discharges. ICD 10 code that triggers PSI #6 J95.811 Postprocedural pneumothorax
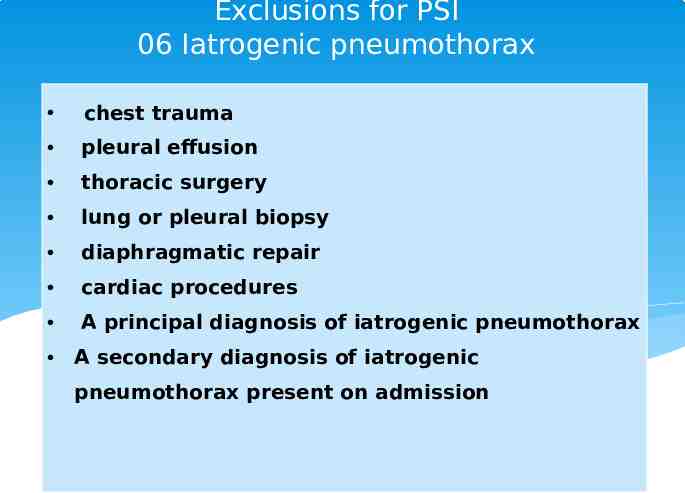
Exclusions for PSI 06 Iatrogenic pneumothorax chest trauma pleural effusion thoracic surgery lung or pleural biopsy diaphragmatic repair cardiac procedures A principal diagnosis of iatrogenic pneumothorax A secondary diagnosis of iatrogenic pneumothorax present on admission
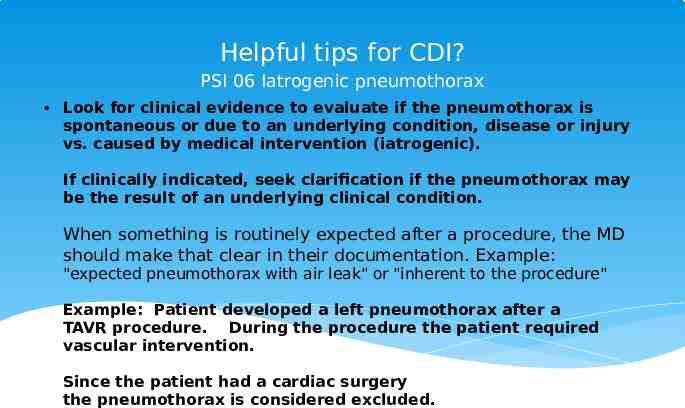
Helpful tips for CDI? PSI 06 Iatrogenic pneumothorax Look for clinical evidence to evaluate if the pneumothorax is spontaneous or due to an underlying condition, disease or injury vs. caused by medical intervention (iatrogenic). If clinically indicated, seek clarification if the pneumothorax may be the result of an underlying clinical condition. When something is routinely expected after a procedure, the MD should make that clear in their documentation. Example: "expected pneumothorax with air leak" or "inherent to the procedure" Example: Patient developed a left pneumothorax after a TAVR procedure. During the procedure the patient required vascular intervention. Since the patient had a cardiac surgery the pneumothorax is considered excluded.
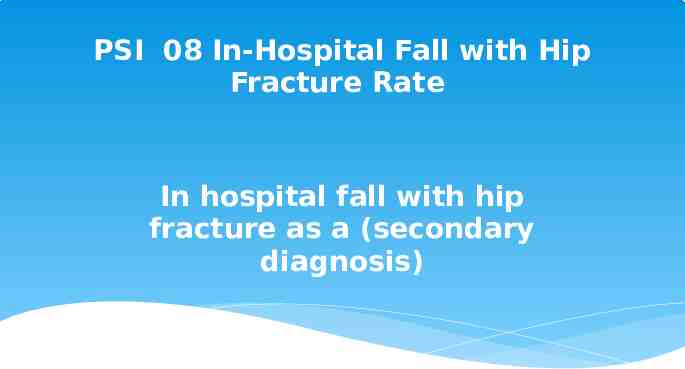
PSI 08 In-Hospital Fall with Hip Fracture Rate In hospital fall with hip fracture as a (secondary diagnosis)
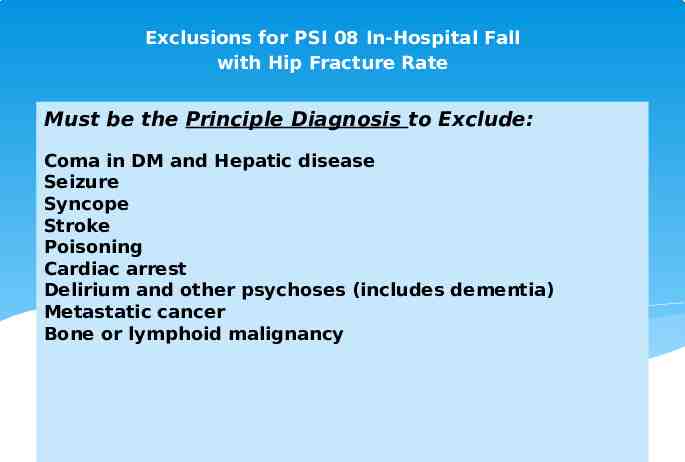
Exclusions for PSI 08 In-Hospital Fall with Hip Fracture Rate Must be the Principle Diagnosis to Exclude: Coma in DM and Hepatic disease Seizure Syncope Stroke Poisoning Cardiac arrest Delirium and other psychoses (includes dementia) Metastatic cancer Bone or lymphoid malignancy
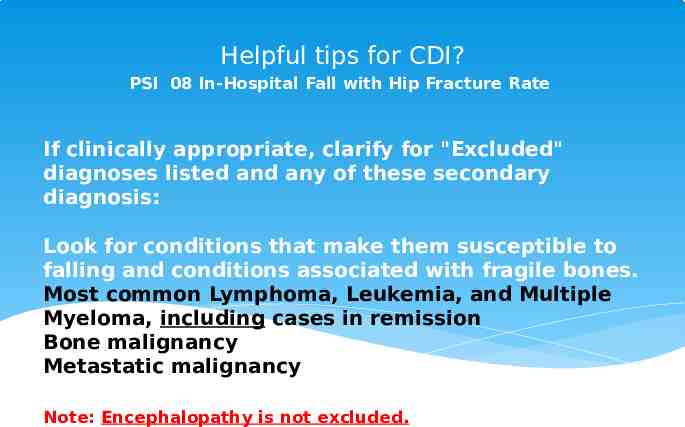
Helpful tips for CDI? PSI 08 In-Hospital Fall with Hip Fracture Rate If clinically appropriate, clarify for "Excluded" diagnoses listed and any of these secondary diagnosis: Look for conditions that make them susceptible to falling and conditions associated with fragile bones. Most common Lymphoma, Leukemia, and Multiple Myeloma, including cases in remission Bone malignancy Metastatic malignancy Note: Encephalopathy is not excluded.
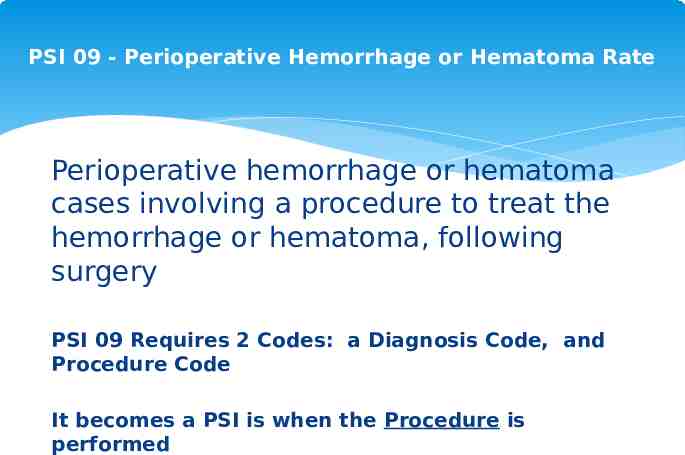
PSI 09 - Perioperative Hemorrhage or Hematoma Rate Perioperative hemorrhage or hematoma cases involving a procedure to treat the hemorrhage or hematoma, following surgery PSI 09 Requires 2 Codes: a Diagnosis Code, and Procedure Code It becomes a PSI is when the Procedure is performed
Exclusions for PSI 09 Perioperative Hemorrhage or Hematoma Rate Coagulation disorders such as thrombocytopenia, DIC, Von Willebrands disease can exclude patient from this PSI.
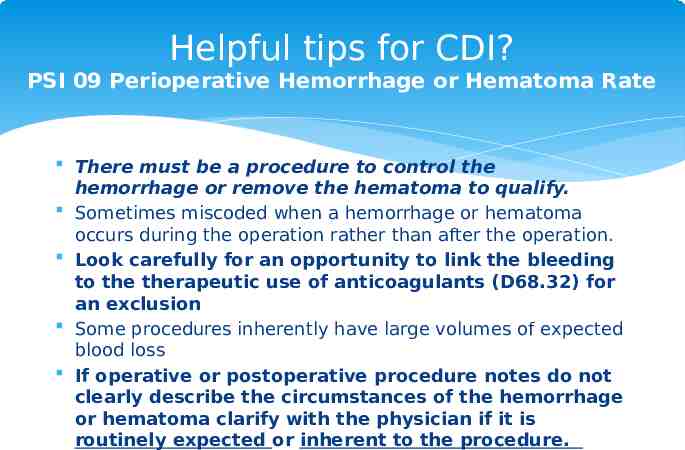
Helpful tips for CDI? PSI 09 Perioperative Hemorrhage or Hematoma Rate There must be a procedure to control the hemorrhage or remove the hematoma to qualify. Sometimes miscoded when a hemorrhage or hematoma occurs during the operation rather than after the operation. Look carefully for an opportunity to link the bleeding to the therapeutic use of anticoagulants (D68.32) for an exclusion Some procedures inherently have large volumes of expected blood loss If operative or postoperative procedure notes do not clearly describe the circumstances of the hemorrhage or hematoma clarify with the physician if it is routinely expected or inherent to the procedure.
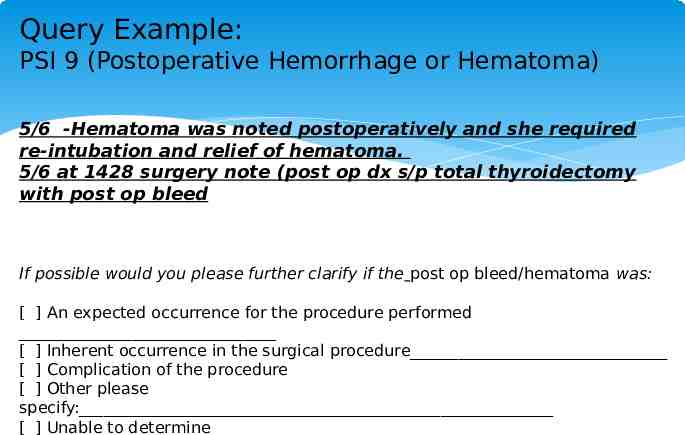
Query Example: PSI 9 (Postoperative Hemorrhage or Hematoma) 5/6 -Hematoma was noted postoperatively and she required re-intubation and relief of hematoma. 5/6 at 1428 surgery note (post op dx s/p total thyroidectomy with post op bleed If possible would you please further clarify if the post op bleed/hematoma was: [ ] An expected occurrence for the procedure performed [ ] Inherent occurrence in the surgical procedure [ ] Complication of the procedure [ ] Other please specify: [ ] Unable to determine
PSI 10 Post-Operative Acute Kidney Injury Requiring Dialysis New onset Acute Kidney Failure which occurs after an elective surgery that requires dialysis.
Exclusions PSI 10 Post-Operative Acute Kidney Injury Requiring Dialysis Rate Acute Kidney Failure as the Principal Diagnosis Acute kidney Failure documented to be present on admission (POA) Cases with acute kidney failure and cardiac arrhythmia, cardiac arrest, shock, urinary tract obstruction or chronic kidney failure;
Helpful tips for CDI? PSI 10 Post-Operative Acute Kidney Injury Requiring Dialysis Rate If this condition develops after surgery, it only counts against PSI #10 if patient needs dialysis.
PSI 11 Postoperative Respiratory Failure Postoperative respiratory failure as a (secondary diagnosis), prolonged mechanical ventilation, or reintubation cases. Acute Respiratory Failure Following Surgery and Postoperative respiratory failure should only be documented if the reason for prolonged mechanical ventilation is directly related to the surgery itself.
PSI 11 Postoperative Respiratory Failure “Prolonged mechanical ventilation” should be defined based on your institutional norms, but should only be considered if the patient remains ventilated for more than 48 hours after surgery. Should not use postop respiratory failure if the patient did not remain on the ventilator longer than would typically be expected for the surgery or procedure performed.
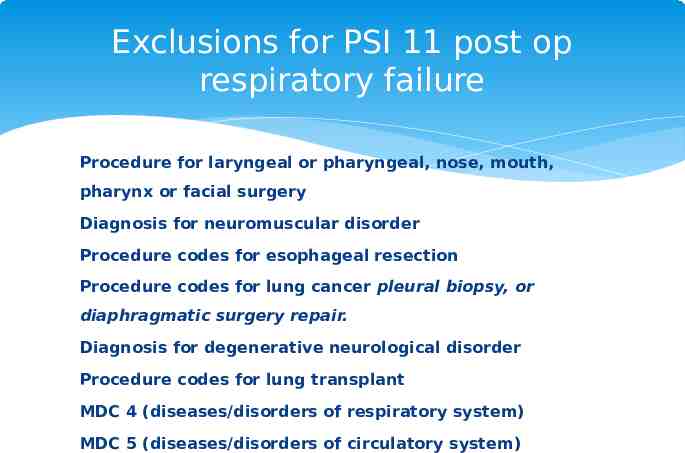
Exclusions for PSI 11 post op respiratory failure Procedure for laryngeal or pharyngeal, nose, mouth, pharynx or facial surgery Diagnosis for neuromuscular disorder Procedure codes for esophageal resection Procedure codes for lung cancer pleural biopsy, or diaphragmatic surgery repair. Diagnosis for degenerative neurological disorder Procedure codes for lung transplant MDC 4 (diseases/disorders of respiratory system) MDC 5 (diseases/disorders of circulatory system)
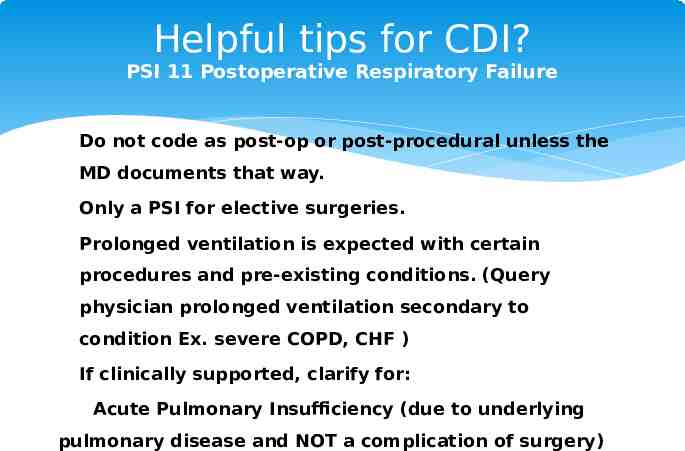
Helpful tips for CDI? PSI 11 Postoperative Respiratory Failure Do not code as post‐op or post‐procedural unless the MD documents that way. Only a PSI for elective surgeries. Prolonged ventilation is expected with certain procedures and pre-existing conditions. (Query physician prolonged ventilation secondary to condition Ex. severe COPD, CHF ) If clinically supported, clarify for: Acute Pulmonary Insufficiency (due to underlying pulmonary disease and NOT a complication of surgery)
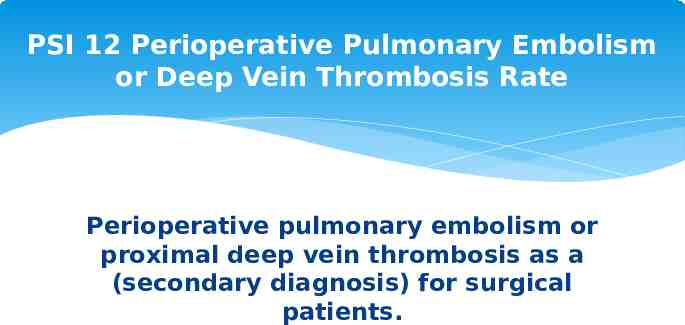
PSI 12 Perioperative Pulmonary Embolism or Deep Vein Thrombosis Rate Perioperative pulmonary embolism or proximal deep vein thrombosis as a (secondary diagnosis) for surgical patients.
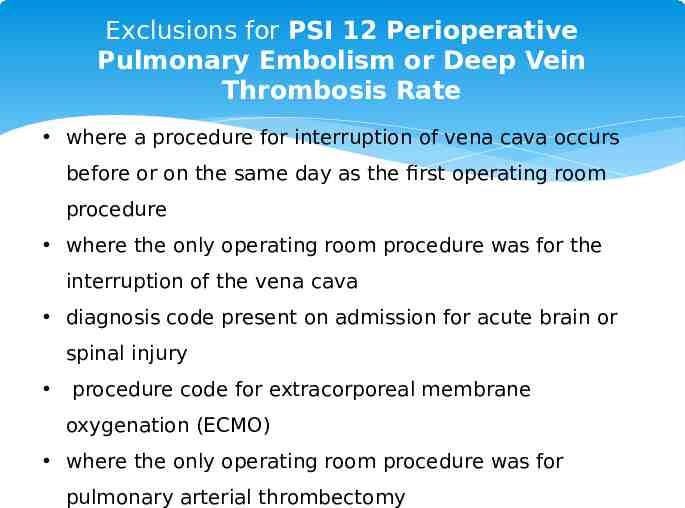
Exclusions for PSI 12 Perioperative Pulmonary Embolism or Deep Vein Thrombosis Rate where a procedure for interruption of vena cava occurs before or on the same day as the first operating room procedure where the only operating room procedure was for the interruption of the vena cava diagnosis code present on admission for acute brain or spinal injury procedure code for extracorporeal membrane oxygenation (ECMO) where the only operating room procedure was for pulmonary arterial thrombectomy
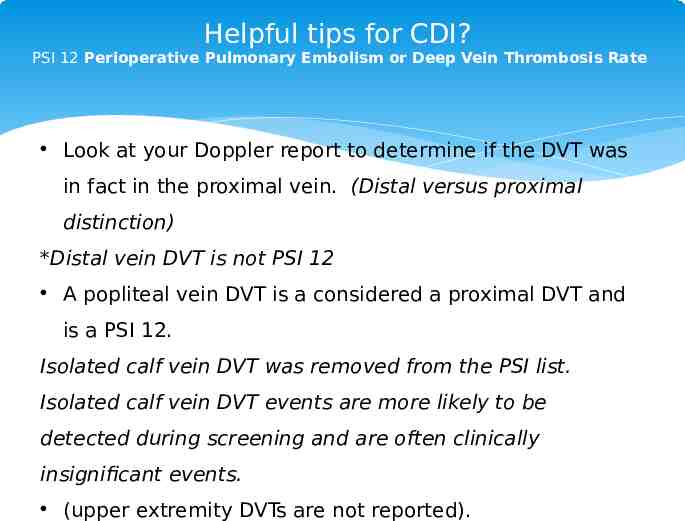
Helpful tips for CDI? PSI 12 Perioperative Pulmonary Embolism or Deep Vein Thrombosis Rate Look at your Doppler report to determine if the DVT was in fact in the proximal vein. (Distal versus proximal distinction) *Distal vein DVT is not PSI 12 A popliteal vein DVT is a considered a proximal DVT and is a PSI 12. Isolated calf vein DVT was removed from the PSI list. Isolated calf vein DVT events are more likely to be detected during screening and are often clinically insignificant events. (upper extremity DVTs are not reported).
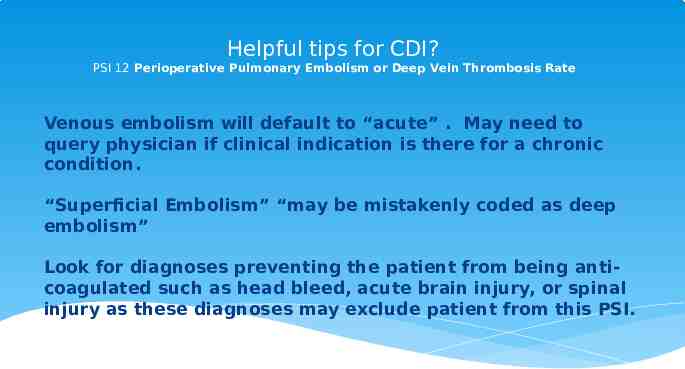
Helpful tips for CDI? PSI 12 Perioperative Pulmonary Embolism or Deep Vein Thrombosis Rate Venous embolism will default to “acute” . May need to query physician if clinical indication is there for a chronic condition. “Superficial Embolism” “may be mistakenly coded as deep embolism” Look for diagnoses preventing the patient from being anti‐ coagulated such as head bleed, acute brain injury, or spinal injury as these diagnoses may exclude patient from this PSI.
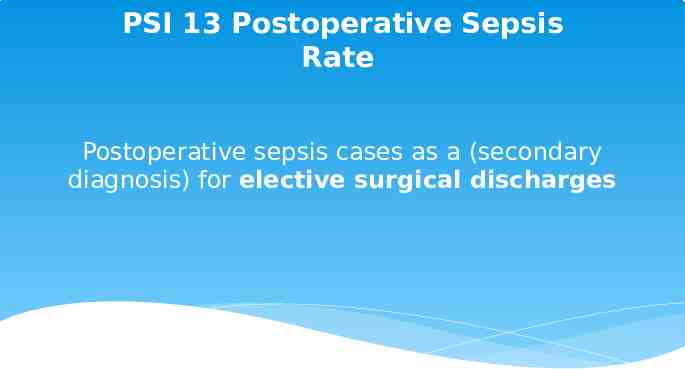
PSI 13 Postoperative Sepsis Rate Postoperative sepsis cases as a (secondary diagnosis) for elective surgical discharges
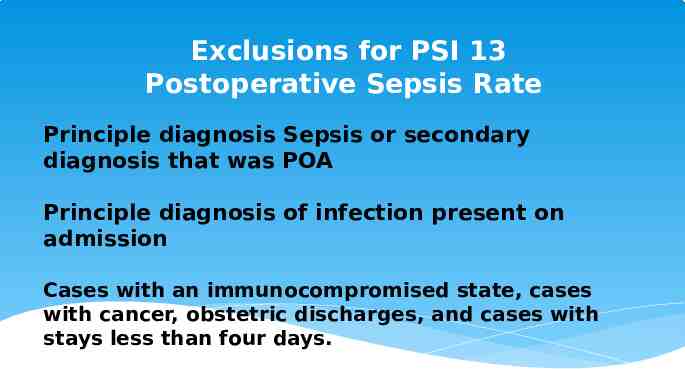
Exclusions for PSI 13 Postoperative Sepsis Rate Principle diagnosis Sepsis or secondary diagnosis that was POA Principle diagnosis of infection present on admission Cases with an immunocompromised state, cases with cancer, obstetric discharges, and cases with stays less than four days.
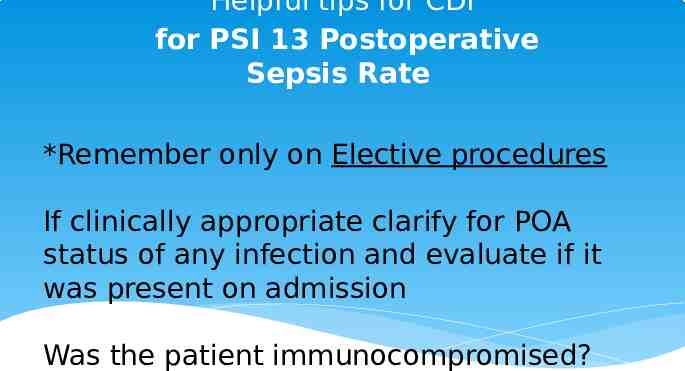
Helpful tips for CDI for PSI 13 Postoperative Sepsis Rate *Remember only on Elective procedures If clinically appropriate clarify for POA status of any infection and evaluate if it was present on admission Was the patient immunocompromised?
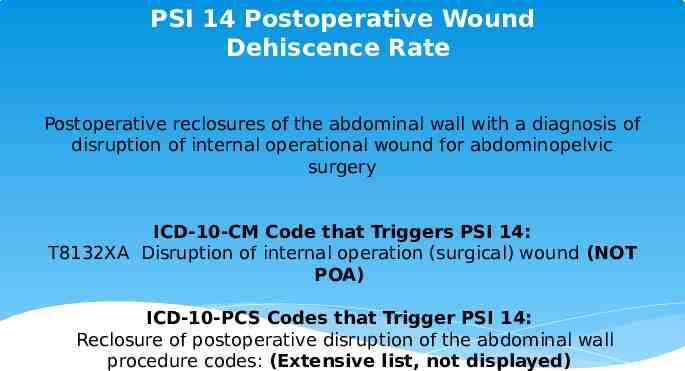
PSI 14 Postoperative Wound Dehiscence Rate Postoperative reclosures of the abdominal wall with a diagnosis of disruption of internal operational wound for abdominopelvic surgery ICD-10-CM Code that Triggers PSI 14: T8132XA Disruption of internal operation (surgical) wound (NOT POA) ICD-10-PCS Codes that Trigger PSI 14: Reclosure of postoperative disruption of the abdominal wall procedure codes: (Extensive list, not displayed)
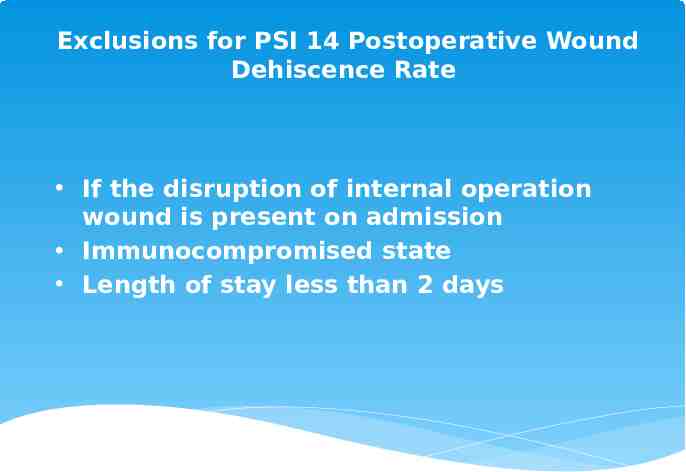
Exclusions for PSI 14 Postoperative Wound Dehiscence Rate If the disruption of internal operation wound is present on admission Immunocompromised state Length of stay less than 2 days
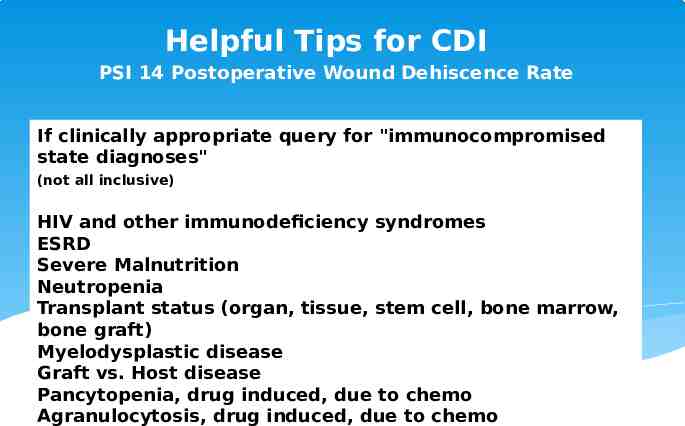
Helpful Tips for CDI PSI 14 Postoperative Wound Dehiscence Rate If clinically appropriate query for "immunocompromised state diagnoses" (not all inclusive) HIV and other immunodeficiency syndromes ESRD Severe Malnutrition Neutropenia Transplant status (organ, tissue, stem cell, bone marrow, bone graft) Myelodysplastic disease Graft vs. Host disease Pancytopenia, drug induced, due to chemo Agranulocytosis, drug induced, due to chemo
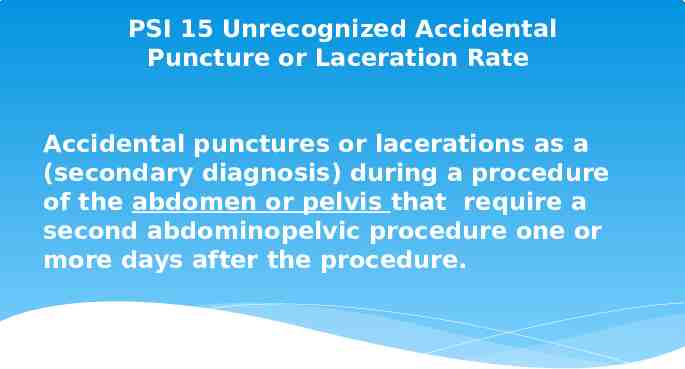
PSI 15 Unrecognized Accidental Puncture or Laceration Rate Accidental punctures or lacerations as a (secondary diagnosis) during a procedure of the abdomen or pelvis that require a second abdominopelvic procedure one or more days after the procedure.
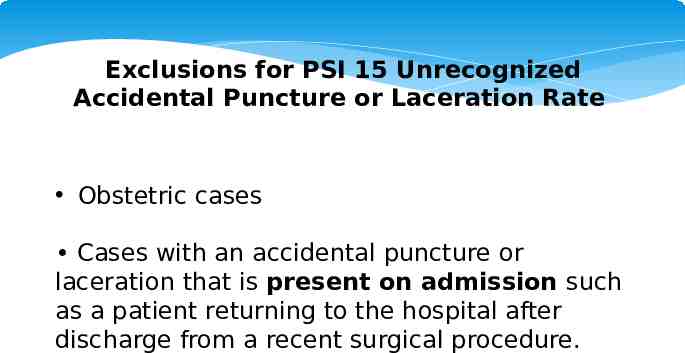
Exclusions for PSI 15 Unrecognized Accidental Puncture or Laceration Rate Obstetric cases Cases with an accidental puncture or laceration that is present on admission such as a patient returning to the hospital after discharge from a recent surgical procedure.
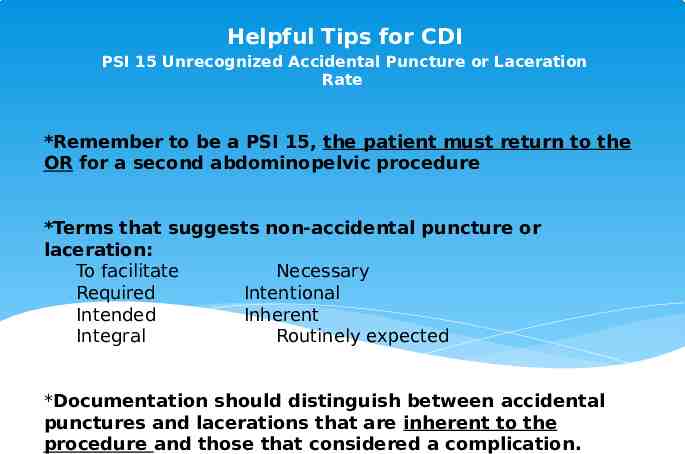
Helpful Tips for CDI PSI 15 Unrecognized Accidental Puncture or Laceration Rate *Remember to be a PSI 15, the patient must return to the OR for a second abdominopelvic procedure *Terms that suggests non-accidental puncture or laceration: To facilitate Necessary Required Intentional Intended Inherent Integral Routinely expected *Documentation should distinguish between accidental punctures and lacerations that are inherent to the procedure and those that considered a complication.
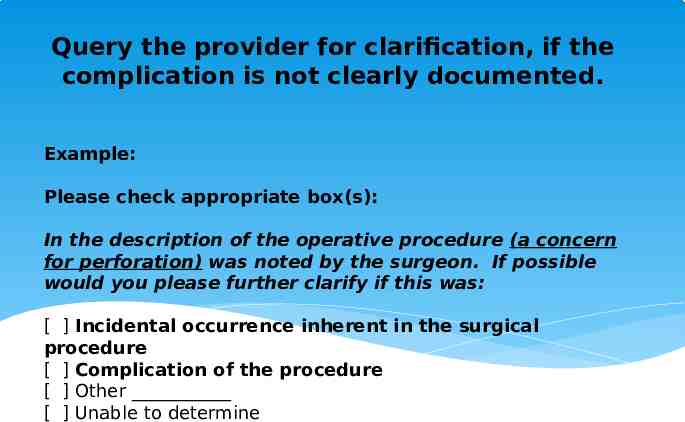
Query the provider for clarification, if the complication is not clearly documented. Example: Please check appropriate box(s): In the description of the operative procedure (a concern for perforation) was noted by the surgeon. If possible would you please further clarify if this was: [ ] Incidental occurrence inherent in the surgical procedure [ ] Complication of the procedure [ ] Other [ ] Unable to determine
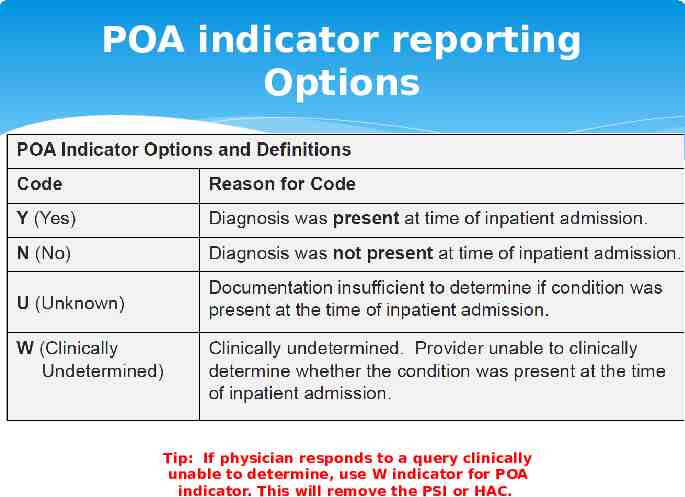
POA indicator reporting Options Tip: If physician responds to a query clinically unable to determine, use W indicator for POA indicator. This will remove the PSI or HAC.
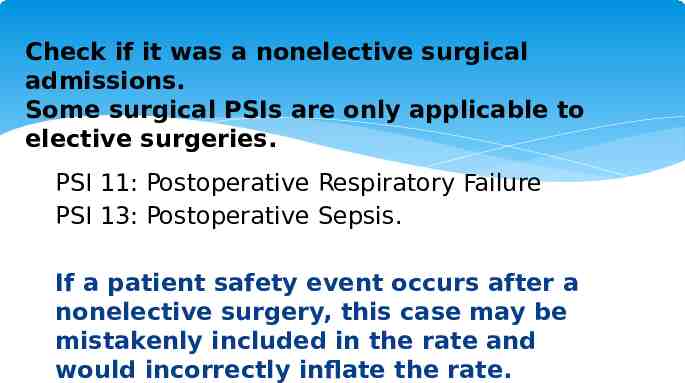
Check if it was a nonelective surgical admissions. Some surgical PSIs are only applicable to elective surgeries. PSI 11: Postoperative Respiratory Failure PSI 13: Postoperative Sepsis. If a patient safety event occurs after a nonelective surgery, this case may be mistakenly included in the rate and would incorrectly inflate the rate.

Sources: Agency for Healthcare Research and Quality (AHRQ) Patient Safety Indicators Overview https://www.qualityindicators.ahrq.gov/Modules/psi resources.aspx CMS Measures Inventory Tool: PSI 90 (August 2018) https://cmit.cms.gov/CMIT public/ListMeasures? struts.token.name token&token IGEFI3TEK7QGBQUOLWH26NA2S8PP41M3&filters &view &m akeStick &wasSearchSub AHRQ PSI 90 Fact Sheet https://www.qualityindicators.ahrq.gov/News/PSI90 Factsheet FAQ v1.pdf