Oral Health Protocol Training—Part II Pamela Alston, DDS, Lead Oral
45 Slides5.20 MB
Oral Health Protocol Training—Part II Pamela Alston, DDS, Lead Oral Health Specialist
CDC’s Guiding Principle CDC’s guiding principle is that dental settings should balance the need to provide necessary services with the need to minimize risk to patients and oral health personnel.
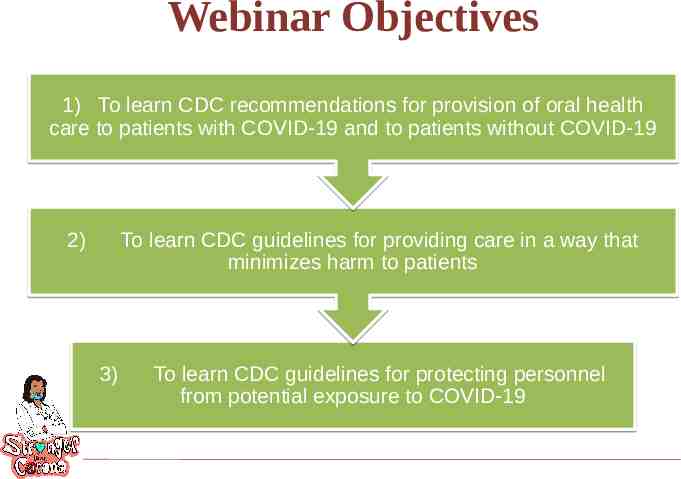
Webinar Objectives 1) To learn CDC recommendations for provision of oral health care to patients with COVID-19 and to patients without COVID-19 2) To learn CDC guidelines for providing care in a way that minimizes harm to patients 3) To learn CDC guidelines for protecting personnel from potential exposure to COVID-19
What is known about the Coronavirus in droplets Inhalation of coronavirus represents a major transmission route (COVID-19). Coronavirus size dictates its aerodynamic behavior, its ability to be inhaled Viruses in droplets (larger than 100 μm) fall in seconds within 6 feet The droplets can be sprayed like tiny cannonballs onto nearby individuals. Physical distancing reduces exposure to these droplets.
What is known about the Coronavirus in Aerosols Virus in aerosols (smaller than 100 μm) can remain suspended in air for hrs They are highly concentrated near an infected person But aerosols containing infectious virus can also travel more than 9 ft They accumulate in poorly ventilated indoor air Individuals with COVID-19, many of whom have no symptoms, release thousands of virus-laden aerosols and far fewer droplets when breathing and talking. Attention is being shifted to protecting against airborne transmission. Reference: Kimberly A. Prather, Linsey C. Marr, Robert T. Schooley, Melissa A. McDiarmid, Mary E. Wilson, Donald K. Milton, Airborne Transmission of SARS-CoV-2, Science 05 Oct 2020
What is known about the Coronavirus in Aerosols Follow existing mandates of mask-wearing, social distancing, hand hygiene Improve indoor air using ventilation and filtration Improve protection for high-risk workers. Reference: Kimberly A. Prather, Linsey C. Marr, Robert T. Schooley, Melissa A. McDiarmid, Mary E. Wilson, Donald K. Milton, Airborne Transmission of SARS-CoV-2, Science 05 Oct 2020
What is known about the Coronavirus in Aerosols Follow existing mandates of mask-wearing, social distancing, hand hygiene Improve indoor air using ventilation and filtration Improve protection for high-risk workers. Reference: Kimberly A. Prather, Linsey C. Marr, Robert T. Schooley, Melissa A. McDiarmid, Mary E. Wilson, Donald K. Milton, Airborne Transmission of SARS-CoV-2, Science 05 Oct 2020
What is known about the Coronavirus in Aerosals Many individuals with COVID-19 don’t have any symptoms COVID-19 individuals release thousands of virus-laden aerosols but far fewer droplets when breathing and talking. One is far more likely to inhale aerosols than be sprayed by a droplet. Attention is being shifted to protecting against airborne transmission. Reference: Kimberly A. Prather, Linsey C. Marr, Robert T. Schooley, Melissa A. McDiarmid, Mary E. Wilson, Donald K. Milton, Airborne Transmission of SARS-CoV-2, Science 05 Oct 2020
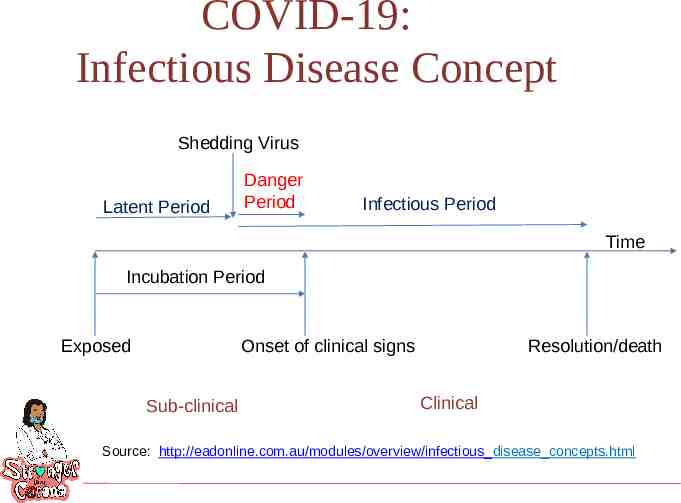
COVID-19: Infectious Disease Concept Shedding Virus Latent Period Danger Period Infectious Period Time Incubation Period Onset of clinical signs Exposed Sub-clinical Resolution/death Clinical Source: http://eadonline.com.au/modules/overview/infectious disease concepts.html
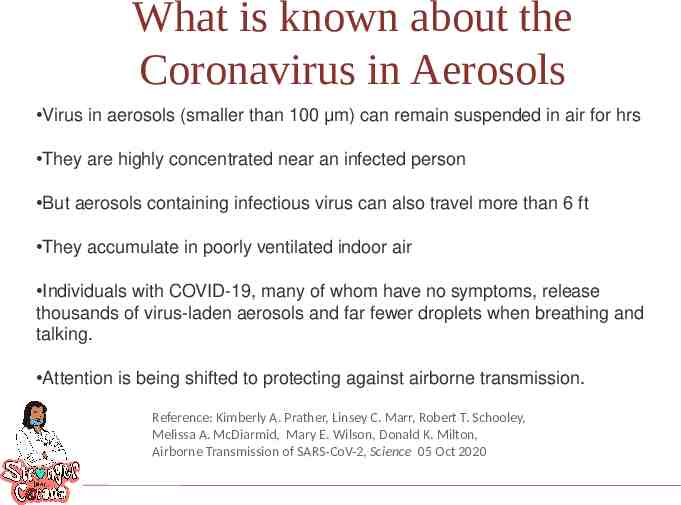
What is known about the Coronavirus in Aerosols Virus in aerosols (smaller than 100 μm) can remain suspended in air for hrs They are highly concentrated near an infected person But aerosols containing infectious virus can also travel more than 6 ft They accumulate in poorly ventilated indoor air Individuals with COVID-19, many of whom have no symptoms, release thousands of virus-laden aerosols and far fewer droplets when breathing and talking. Attention is being shifted to protecting against airborne transmission. Reference: Kimberly A. Prather, Linsey C. Marr, Robert T. Schooley, Melissa A. McDiarmid, Mary E. Wilson, Donald K. Milton, Airborne Transmission of SARS-CoV-2, Science 05 Oct 2020
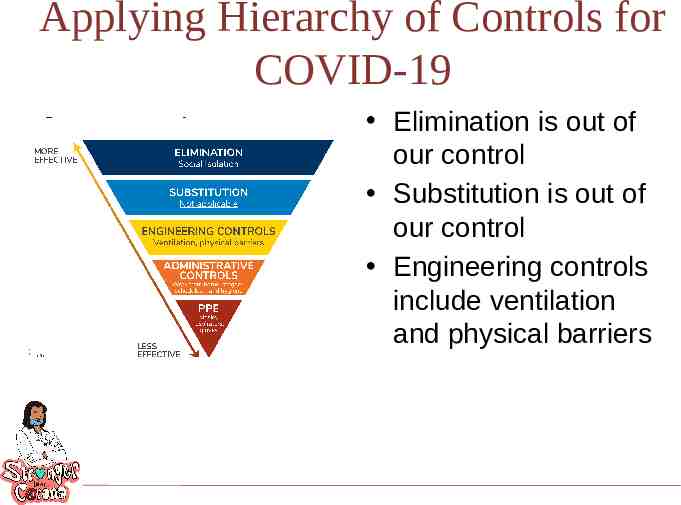
Applying Hierarchy of Controls for COVID-19 Elimination is out of our control Substitution is out of our control Engineering controls include ventilation and physical barriers
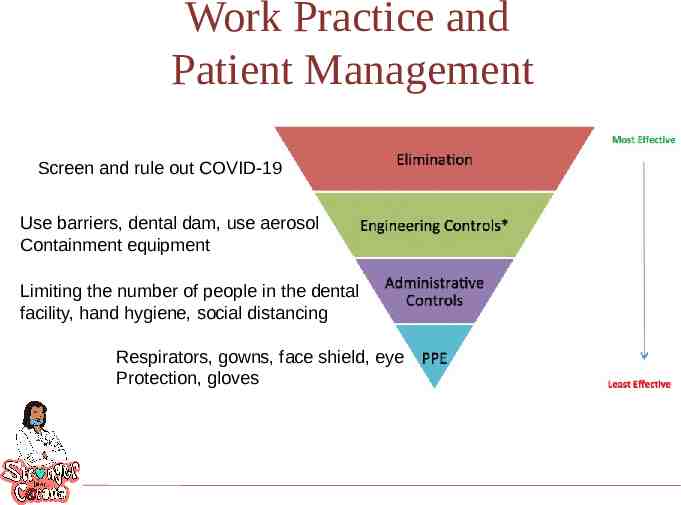
Work Practice and Patient Management Screen and rule out COVID-19 Use barriers, dental dam, use aerosol Containment equipment Limiting the number of people in the dental facility, hand hygiene, social distancing Respirators, gowns, face shield, eye Protection, gloves
Precautions When Performing Aerosol Generating Procedures (AGPs) Perform AGP cautiously and avoid if possible. If performed, the following should occur: – wear an N95 mask, eye protection, gloves, and a gown. – AGPs should ideally take place in an AIIR. Use high volume intraoral suction Use extraoral vacuum unit between patient’s mouth and provider’s face An air purification filtration/UV germicidal irradiation system.
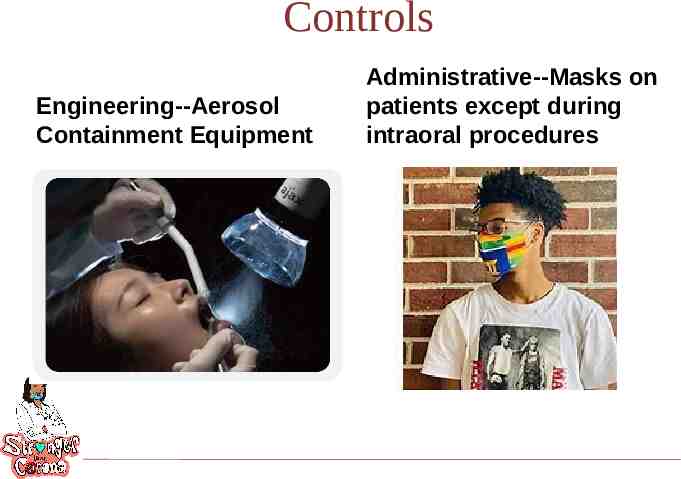
Controls Engineering--Aerosol Containment Equipment Administrative--Masks on patients except during intraoral procedures
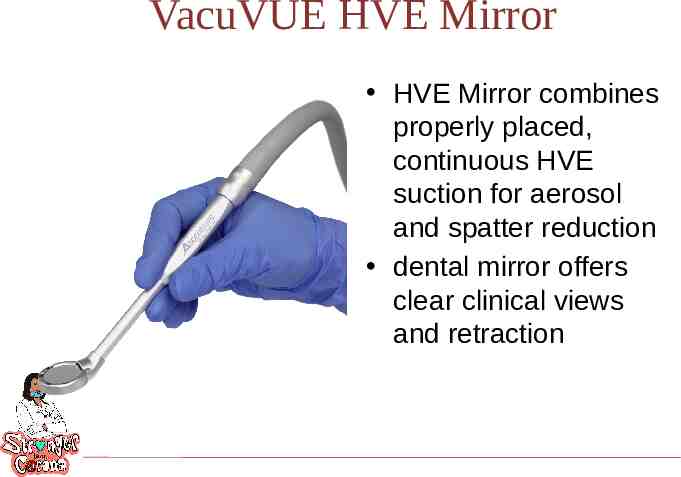
VacuVUE HVE Mirror HVE Mirror combines properly placed, continuous HVE suction for aerosol and spatter reduction dental mirror offers clear clinical views and retraction
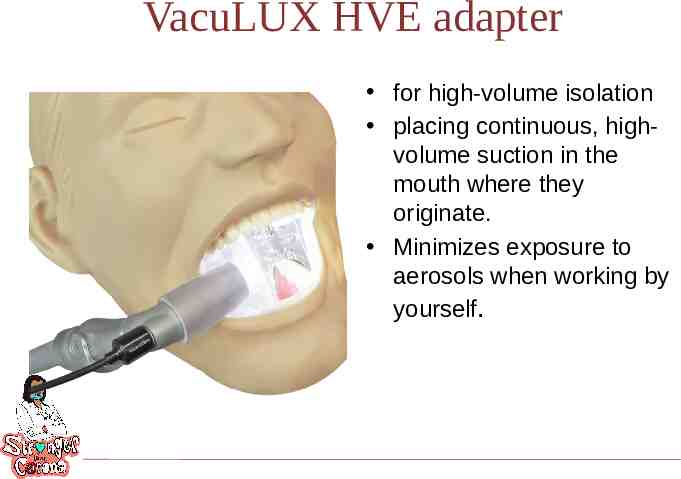
VacuLUX HVE adapter for high-volume isolation placing continuous, highvolume suction in the mouth where they originate. Minimizes exposure to aerosols when working by yourself.
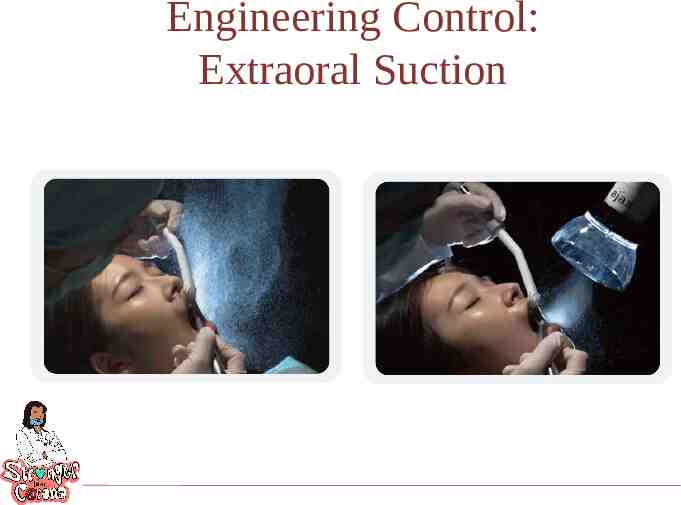
Engineering Control: Extraoral Suction
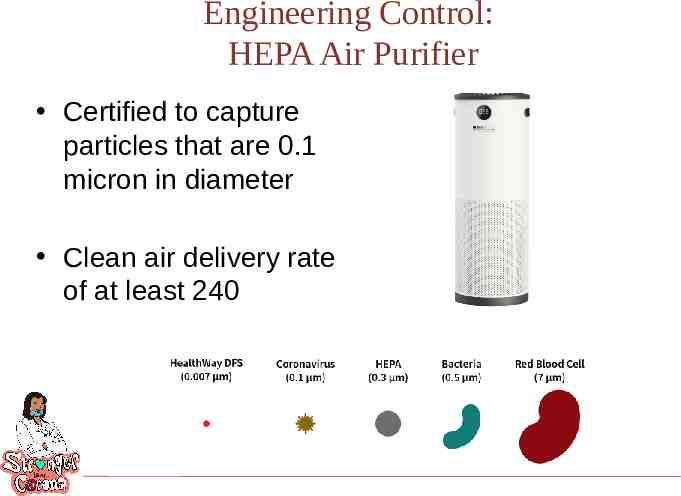
Engineering Control: HEPA Air Purifier Certified to capture particles that are 0.1 micron in diameter Clean air delivery rate of at least 240
Oral Health Personnel OSHA categorizes oral health personnel as very high risk when performing aerosol generating procedures Rotary dental instruments create a visible spray The spray contains particle droplets No confirmed cases of COVID-19 transmitted in a dental setting OHP have the potential for direct or indirect exposure to patients or infectious materials including: o body substances o contaminated medical supplies, devices, and equipment o contaminated environmental surfaces o contaminated air
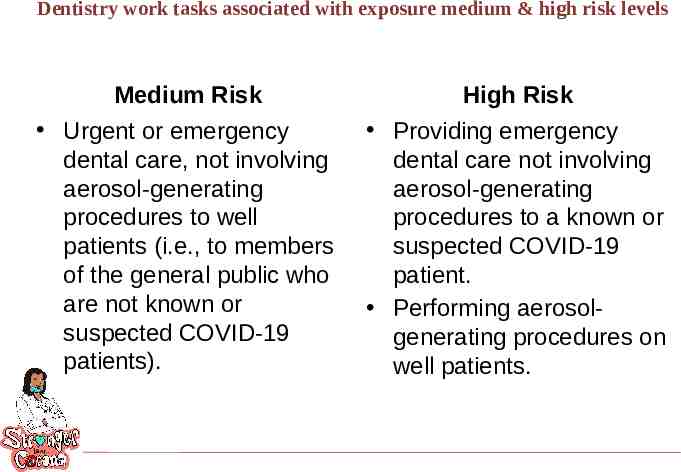
Dentistry work tasks associated with exposure medium & high risk levels Medium Risk High Risk Urgent or emergency dental care, not involving aerosol-generating procedures to well patients (i.e., to members of the general public who are not known or suspected COVID-19 patients). Providing emergency dental care not involving aerosol-generating procedures to a known or suspected COVID-19 patient. Performing aerosolgenerating procedures on well patients.
CDC’s Interim Infection Prevention and Control Guidance for Dental Settings CDC’s Interim Guidance supplements the 2003 Guidance “Interim” indicates that the guidelines were developed using less thorough processes. CDC issued CDC's Interim Guidance in 2020 for Dental Settings in March, April, May and June. The latest guidance was issued June 3rd.
Telehealth
CDC Interim Infection Prevention and Control Guidance for Dental Settings Initially recommended that only dentists only perform emergency evaluations and urgent care Used the American Dental Association’s definitions for emergency & urgent conditions 2 reasons for delaying elective visits and procedures--to protect oral health personnel and to preserve PPE Removed recommendation that all elective procedures be postponed on May 18, 2020
Health Care System caveats for providing elective services Must operate without crisis standards Ensure adequate staffing Must have PPE & other supplies available Must have a plan in the case of a community surge in transmissions Have patient scheduling and flow protocols
Getting Ready to Reopen Take inventory to decide on supply of PPE and supplies (2 weeks of PPE in clinic) Know what methods will be in place to reduce/eliminate aerosol production Learn about facility screening practice for COVID-19 Decide the logistics for social distancing among patients and the dental team
Getting the dental facility ready Dental unit waterlines (DUWL) Autoclaves and instrument cleaning equipment Air compressor, vacuum and suction lines, radiography equipment, high-tech equipment, amalgam separators, and other dental equipment: Follow protocol for recommended maintenance per manufacturer IFU. Get the ventilation system checked.
When Oral Health Personnel Return As part of routine practice, monitor selves for fever and symptoms consistent with COVID-19. Provide for oral health personnel to stay home when ill or under quarantine without jeopardizing job security. If fever (T 100.0 F) or symptoms consistent with COVID19 develop while at work, keep cloth face covering or facemask on, inform supervisor, and leave the workplace.
When Oral Health Personnel Return Evaluate the necessity of the dental care based on urgency Prioritize care that was previously postponed Prioritize dental conditions likely to lead to dental emergencies if treatment is not provided in a timely manner. Provide preventive services (fluoride, sealants, scaling) taking measures to minimize aerosol generation. Consider minimally invasive restorative techniques If aerosol generating procedures are necessary, employ aerosol management tools
Aggressive Source Control* Measures Perform fever and symptom tracking. Require everyone to wear a cloth face covering while in the dental facility, regardless of symptoms. Instruct patients to perform hand hygiene before and after they touch or adjust their cloth face covering Have appropriate triage, evaluation, and isolation of individuals who report symptoms should still occur. *Source control presumes everyone is infected and symptomatic and asymptomatic and sets forth measures that might help reduce the risk of transmission of SARS CoV-2.
Have you experienced any of the following symptoms in the past 48 hours? fever or chills cough shortness of breath or difficulty breathing fatigue muscle or body aches headache new loss of taste or smell sore throat congestion or runny nose nausea or vomiting diarrhea This tool was developed by the Centers for Disease Control and Prevention (CDC) for use by CDC. The tool, however, is in the public domain and may be recreated, utilized, and adapted by the public at will. The CDC name and logo may not be utilized if the tool is recreated for use by an external entity. The tool is provided “as-is”; CDC accepts no liability for the use by an external entity. The external entity assumes all risks and liabilities associated with the recreation, utilization and adaption of the tool for external entity’s use. CDC will not provide any support for the tool if recreated by an external entity. CDC, with regard to this tool, makes no other representations, warranties, express or implied, and hereby disclaims all implied representation and warranties, including any warranty of merchantability and warranty of fitness for a particular purpose.
Personal Protective Equipment Dental procedures not involving aerosol-generating procedures Dental procedures that may or are known to generate aerosols Work clothing, such as scrubs, lab coat, and/or smock, or a gown Gloves Eye protection (e.g., goggles, face shield) NIOSH-certified, N95 filtering facepiece respirator or better (can be a “duckbill” type Gloves Gown Eye protection (e.g., goggles, face shield) NIOSH-certified, N95 filtering facepiece respirator or better (can be a “duckbill” type
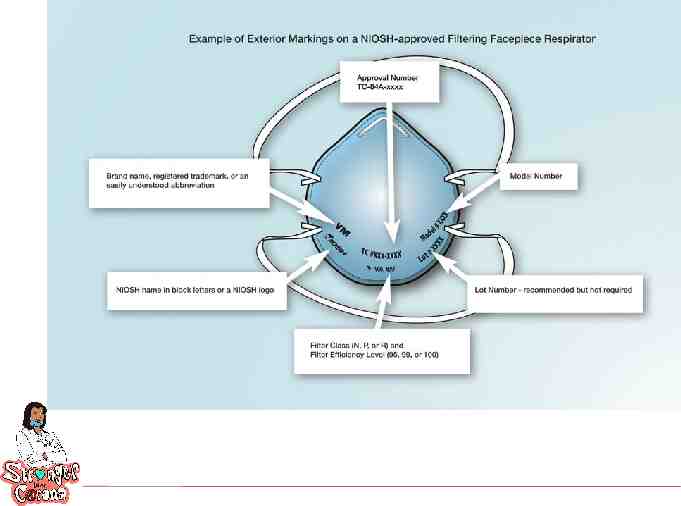
Respirators Recommended for oral health personnel during the COVID-19 N95 respirators or respirators that offer a higher level of protection should be used instead of a facemask when performing or present for an aerosol generating procedure Must be in the context of a complete respiratory protection program in accordance with OSHA Respiratory Protection standard (29 CFR 1910.134) OSHA has issued temporary enforcement guidance regarding discretion, e.g., enforcement discretion for required annual fit testing
Extended Use of Facemasks and Respirators Should only be undertaken when the facility is at contingency or crisis capacity and has reasonably implemented all applicable administrative and engineering controls. Such controls include selectively canceling elective and non-urgent procedures and appointments for which PPE is typically used by DHCP Extended use of PPE is not intended to encourage dental facilities to practice at a normal patient volume during a PPE shortage, but only to be implemented in the short term when other controls have been exhausted. Once the supply of PPE has increased, facilities should return to standard procedures.
Eye Protection Put on eye protection (i.e., goggles or a disposable face shield that covers the front and sides of the face) upon entry to the patient room or care area, if not already wearing as part of extended use or reuse strategies to optimize to optimize PPE supply. Personal eyeglasses and contact lenses are NOT considered adequate eye protection. Reusable eye protection (e.g., goggles or loupes) must be cleaned and disinfected according to manufacturer’s reprocessing instructions prior to re-use.
Gloves – Put on clean, non-sterile gloves upon entry into the patient room or care area. – Change gloves if they become torn or heavily contaminated during the patient visit. – Remove and discard gloves when leaving the patient room or care area and immediately perform hand hygiene.
Gowns – Put on a clean isolation gown upon entry into the patient room or area. – Change the gown if it becomes soiled and after aerosol generating procedures – If there are shortages of gowns, they should be prioritized for: aerosol generating procedures care activities where splashes and sprays are anticipated
Headcovers and shoe covers Not considered PPE Heads are close enough for droplets and aerosols to land on Shoes touch floors where droplets land
Environmental Infection Control Ensure that environmental cleaning and disinfection procedures are followed consistently and correctly. Routine cleaning and disinfection procedures (e.g., using cleaners and water to pre-clean surfaces prior to applying an EPA-registered, disinfectant
Disinfection Wait 15 minutes after completion of clinical care and exit of each patient to begin to clean and disinfect room surfaces. Appropriate PPE should be worn for all activities involving potential exposure to patient body fluids, contaminated surfaces and equipment, and hazardous chemicals (e.g. disinfectants). Puncture resistant/utility gloves, masks, eye protection and gowns should be worn while handling contaminated instruments. Patients should be scheduled in a manner that allows for complete disinfection of operatories. It is recommended to increase patient appointment time Do not double-book appointments. Barriers should be used when possible, especially for hard-to-clean surfaces (e.g. light switches, computer, mouse, dental unit) and changed between patients.
“During the resumption process, centers must abide by federal, state, and local regulations regarding physical distancing, size of group gatherings, and wearing face masks by following whichever regulations are the most restrictive. In some cases, PRH requirements may not be able to be met because they are in conflict with regulations.”
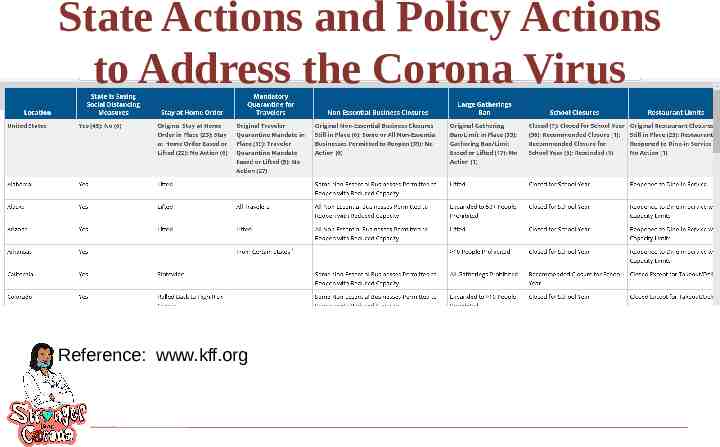
State Actions and Policy Actions to Address the Corona Virus Reference: www.kff.org
“Until more is known about how COVID19 spreads, OSHA recommends—” using a combination of standard precautions, contact precautions, and contact precautions. performing patient care that does not involve aerosol-generating procedures on individuals without suspected or confirmed COVID19 Follow OSHA's Bloodborne Pathogens (29 CFR 1910.1030) standard Follow Personal Protective Equipment (29 CFR 1910.132) standard Follow OSHA’s Respiratory Protection (29 CFR 1910.134) standard
References ADHA Interim Guidance on Returning to Work adha.org CDC’s Interim Infection Prevention and Control Recommendations for Patient s with Suspected or Confirmed Coronavirus Disease 2019 (COVID-19) i n Healthcare Settings Guidelines for Infection Control in Dental Health Care Settings – 2003 Interim Infection Prevention and Control Guidance for Dental Settings During the COVID-19 Response(May 19, 2020) https://www.cdc.gov/coronavirus/2019-ncov/hcp/dental-settings.html
Resiliency “I can be changed by what happens to me but I refuse to be reduced by it.” --Maya Angelou