Maryland NextGen Testbank: Fundamentals Mini-Review
79 Slides2.99 MB

Maryland NextGen Testbank: Fundamentals Mini-Review
NextGen Test Bank Disclosures This review uses items in the Maryland NextGen Test Bank accessed with a Qualtrics link or QR Code. The Maryland Testbank contains peer-reviewed items written by faculty across the State of Maryland that attempt to align with publicly available information about Next Generation NCLEX. The Maryland NextGen Test Bank Project was funded by the Maryland Nursing Workforce Center as part of a grant from the Maryland Higher Education Commission Nurse Support Program II # 20125. This review will take approximately 1.5 to 2 hours to complete. For best result, use a laptop, notebook, or desktop to answer the questions.
About The NextGen NCLEX Starting April 1, 2023, graduates will take an updated version of the National Council Licensure Exam referred to as Next Generation NCLEX. Next Generation NCLEX (NGN) will continue to test a candidate’s ability to provide safe client care while incorporating new methods to better test clinical judgment. The testing methods will include using new item response types in clinical judgment case studies and stand-alone questions to test the NCSBN Clinical Judgment Measurement Model(NCJMM) ( https://www.ncsbn.org/exams/next-generation-nclex/NGN Resources/clinical-j udgment-measurement-model.page )
The Five New Item Response Types Extended multiple response items with increased answer options. Drag-and-drop items that involve moving options to placeholders. Drop-down items where candidates select the missing words from sentences, paragraphs, or tables. Highlight items that require candidates to identify parts of the medical record to answer questions. Matrix/grid items that involve completing tables of information.
Case Studies Unfolding case studies use approved NGN item types to answer questions about evolving real-world nursing scenarios. Case studies present 6 linked questions to test the 6 steps of the NCJMM in order: 1. Recognize cues 2. Analyze cues 3. Prioritize hypotheses 4. Generate solutions 5. Take action 6. Evaluate outcomes Candidates should expect to complete 3 to 5 case studies in a minimum length 85 question NCLEX exam.
Stand-alone Item Types Stand-alone (single) items test either client needs or clinical judgment Client needs items test knowledge of the 8 client needs using traditional or new item types. Clinical judgment items present information in a clinical scenario specifically targeting one or more NCJMM clinical judgment step. There are 2 unique types of clinical judgment stand-alone items: Bowtie Trend Clinical judgment stand-alone items make up approximately 10% of stand-alone items.
Stand-alone Item: Bowtie A bowtie is a drag-and-drop response item variation. After reading a clinical scenario, candidates move response options (tokens) to placeholders (targets). On NCLEX the placeholders are arranged in the shape of a bowtie. Candidates must select: 1 condition the client is most likely experiencing from 4 options. 2 actions to take to address the condition from 5 options. 2 parameters to monitor the client’s progress from 5 options.
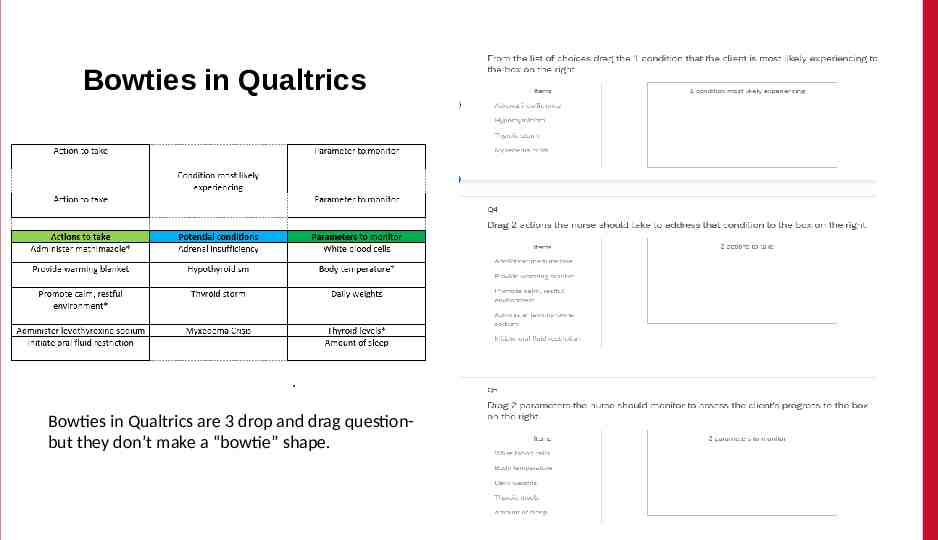
Bowties in Qualtrics Bowties in Qualtrics are 3 drop and drag questionbut they don’t make a “bowtie” shape.
Stand-alone Item: Trends Trend items require the candidate to make clinical judgments based on client data presented at different time points. Trend items may address one or more clinical judgment steps but do not follow the sixitem sequence like case studies do. Trend items can feature any item response type except bowtie.
About This Review Your instructor will provide a QR code or link to answer a series of case studies, bowtie items and trends across a lifespan While questions throughout the test bank use all 5 new item response, not all specific variations that might be used on NCLEX are not included such as drop-down items formatted as a table. Information needed to answer questions will be displayed in a medical record, but the medical record will display differently on the actual NCLEX. To see how items will exactly appear on NCLEX see tutorials at https://nclex.com/next-generation-nclex.page
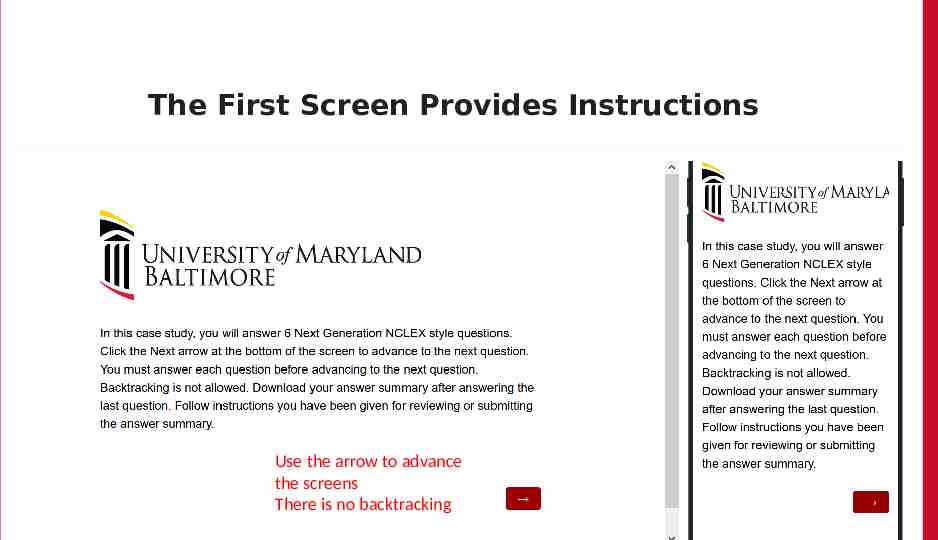
The First Screen Provides Instructions Use the arrow to advance the screens There is no backtracking
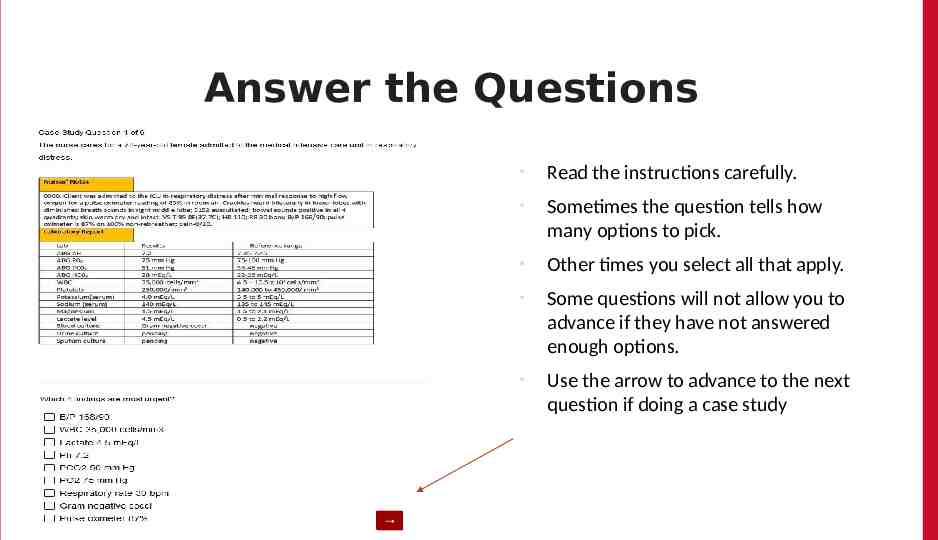
Answer the Questions Read the instructions carefully. Sometimes the question tells how many options to pick. Other times you select all that apply. Some questions will not allow you to advance if they have not answered enough options. Use the arrow to advance to the next question if doing a case study
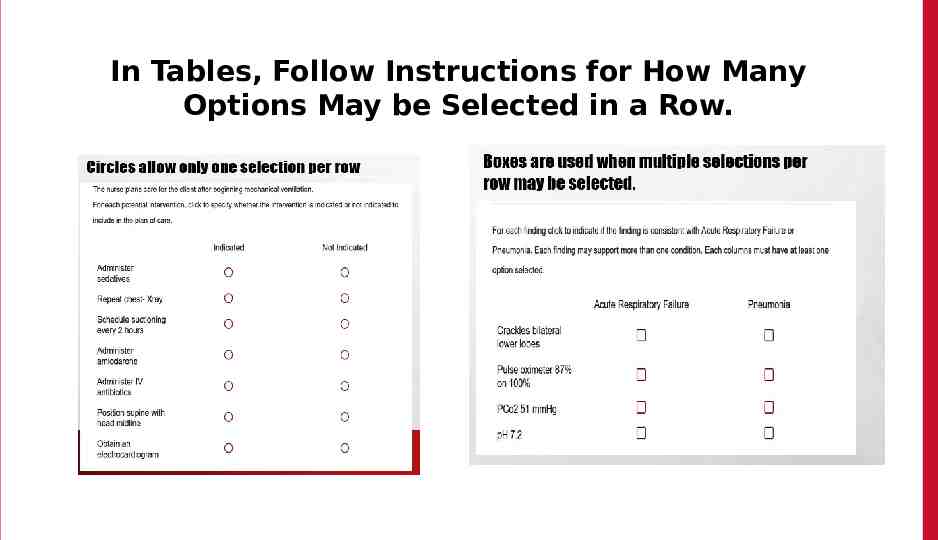
In Tables, Follow Instructions for How Many Options May be Selected in a Row.
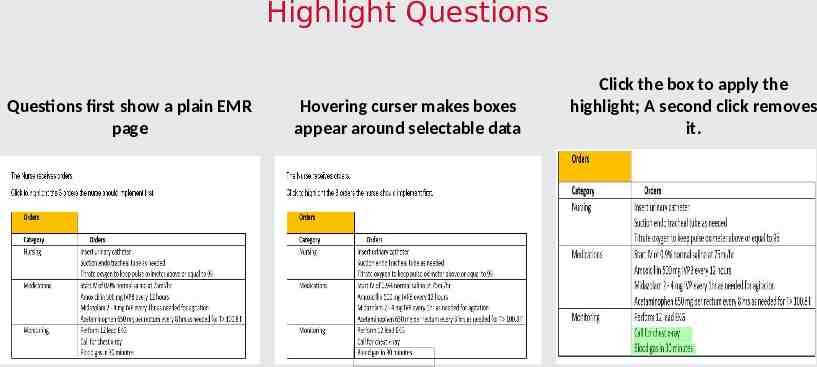
Highlight Questions Questions first show a plain EMR page Hovering curser makes boxes appear around selectable data Click the box to apply the highlight; A second click removes it.
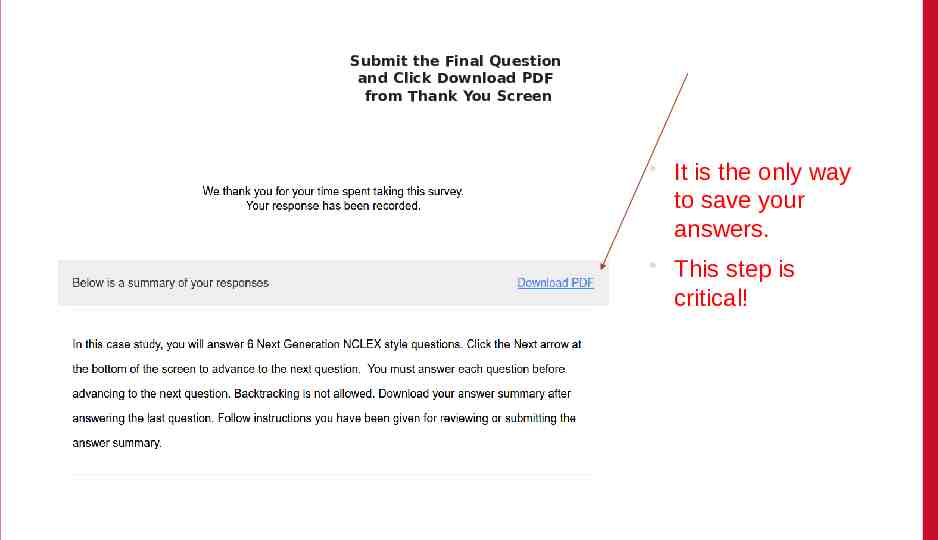
Submit the Final Question and Click Download PDF from Thank You Screen It is the only way to save your answers. This step is critical!
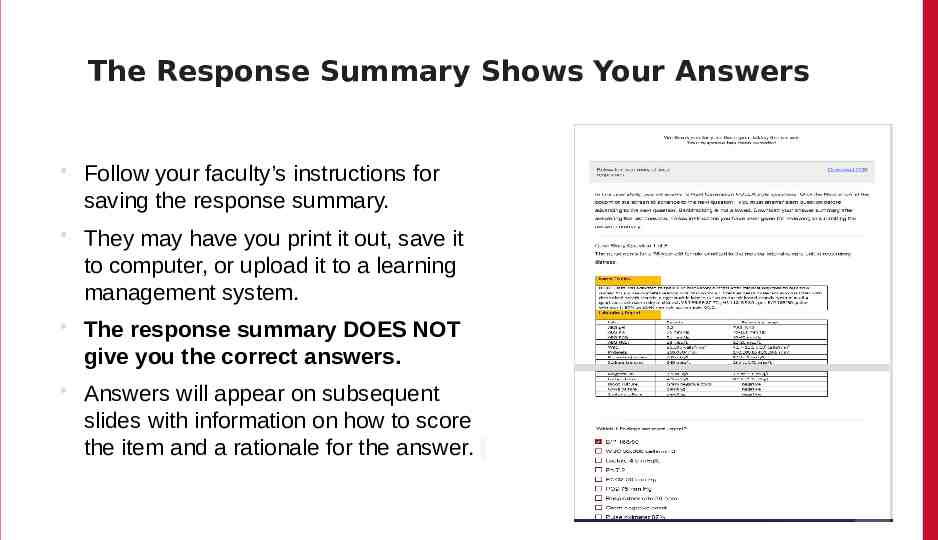
The Response Summary Shows Your Answers Follow your faculty’s instructions for saving the response summary. They may have you print it out, save it to computer, or upload it to a learning management system. The response summary DOES NOT give you the correct answers. Answers will appear on subsequent slides with information on how to score the item and a rationale for the answer.
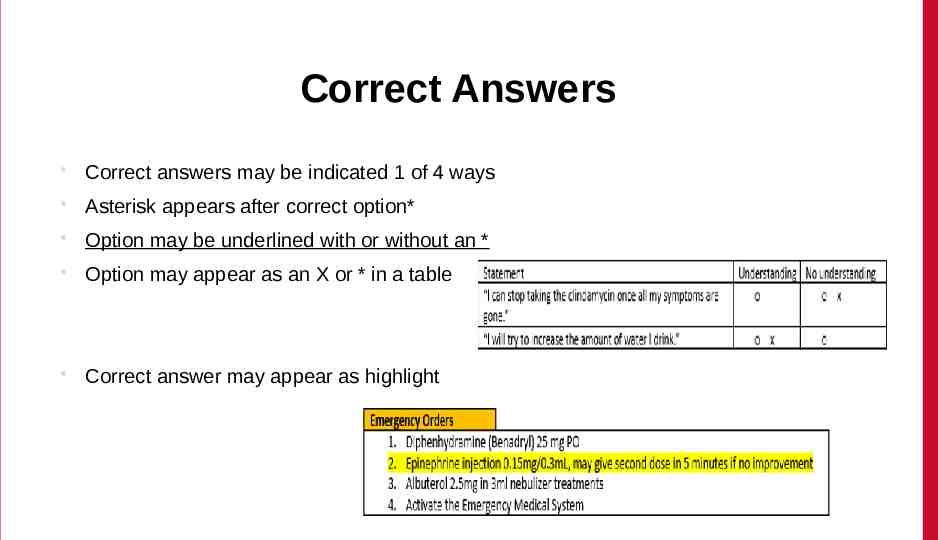
Correct Answers Correct answers may be indicated 1 of 4 ways Asterisk appears after correct option* Option may be underlined with or without an * Option may appear as an X or * in a table Correct answer may appear as highlight
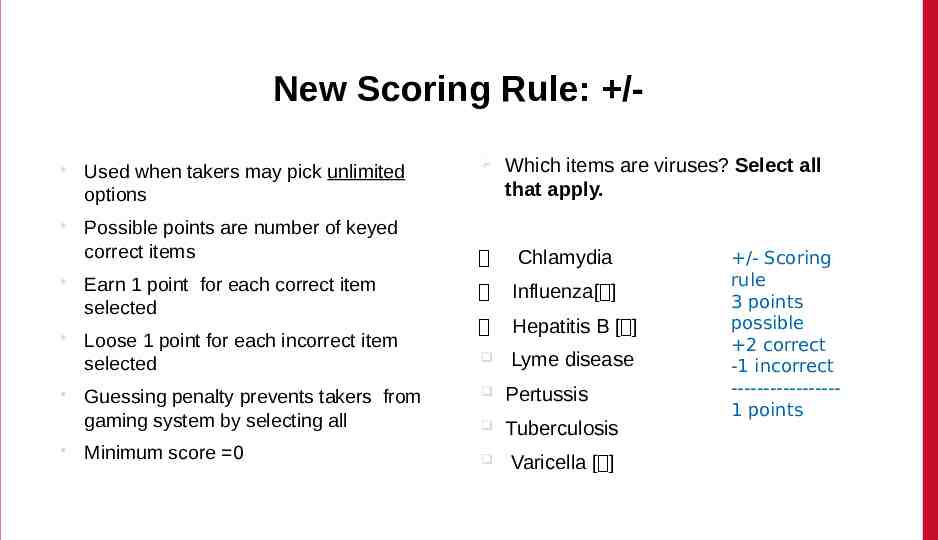
New Scoring Rule: / Used when takers may pick unlimited options Possible points are number of keyed correct items Which items are viruses? Select all that apply. Chlamydia Earn 1 point for each correct item selected Influenza[ ] Loose 1 point for each incorrect item selected Hepatitis B [ ] Lyme disease Guessing penalty prevents takers from gaming system by selecting all Minimum score 0 Pertussis Tuberculosis Varicella [ ] /- Scoring rule 3 points possible 2 correct -1 incorrect ----------------1 points
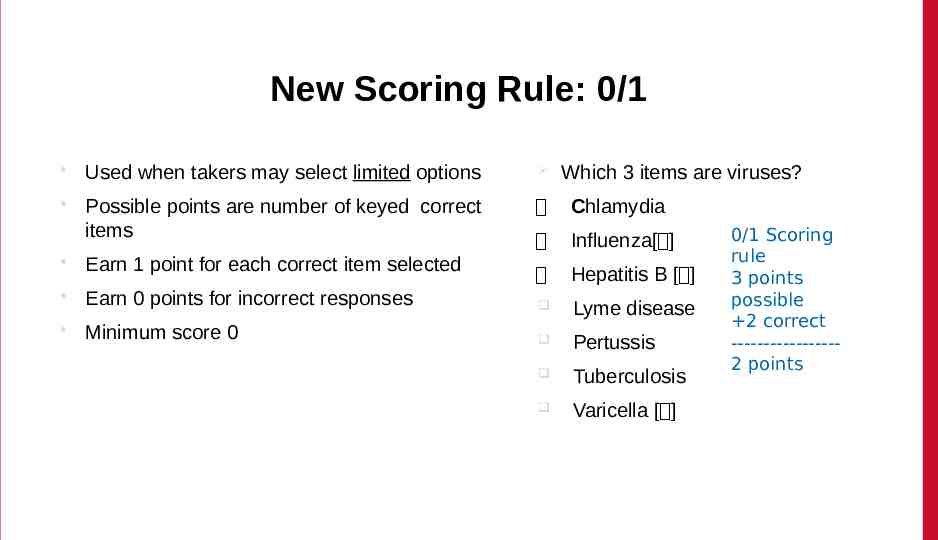
New Scoring Rule: 0/1 Used when takers may select limited options Which 3 items are viruses? Possible points are number of keyed correct items Chlamydia Influenza[ ] Earn 1 point for each correct item selected Hepatitis B [ ] Earn 0 points for incorrect responses Lyme disease Minimum score 0 Pertussis Tuberculosis Varicella [ ] 0/1 Scoring rule 3 points possible 2 correct ----------------2 points
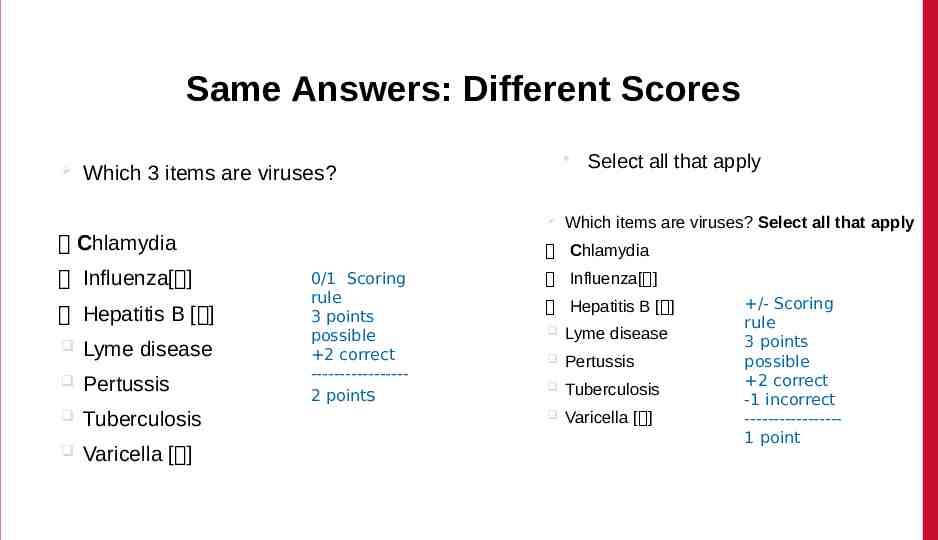
Same Answers: Different Scores Which 3 items are viruses? Chlamydia Influenza[ ] Hepatitis B [ ] Lyme disease Pertussis Tuberculosis Varicella [ ] Select all that apply Which items are viruses? Select all that apply Chlamydia 0/1 Scoring rule 3 points possible 2 correct ----------------2 points Influenza[ ] Hepatitis B [ ] Lyme disease Pertussis Tuberculosis Varicella [ ] /- Scoring rule 3 points possible 2 correct -1 incorrect ----------------1 point
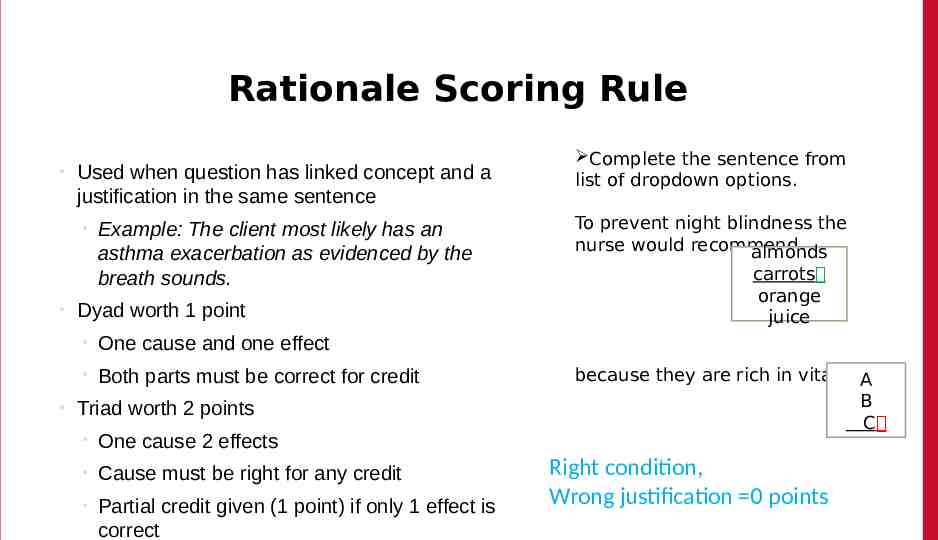
Rationale Scoring Rule Used when question has linked concept and a justification in the same sentence Example: The client most likely has an asthma exacerbation as evidenced by the breath sounds. Dyad worth 1 point One cause and one effect Both parts must be correct for credit Triad worth 2 points One cause 2 effects Cause must be right for any credit Partial credit given (1 point) if only 1 effect is correct Complete the sentence from list of dropdown options. To prevent night blindness the nurse would recommend almonds carrots orange juice because they are rich in vitaminA B C Right condition, Wrong justification 0 points
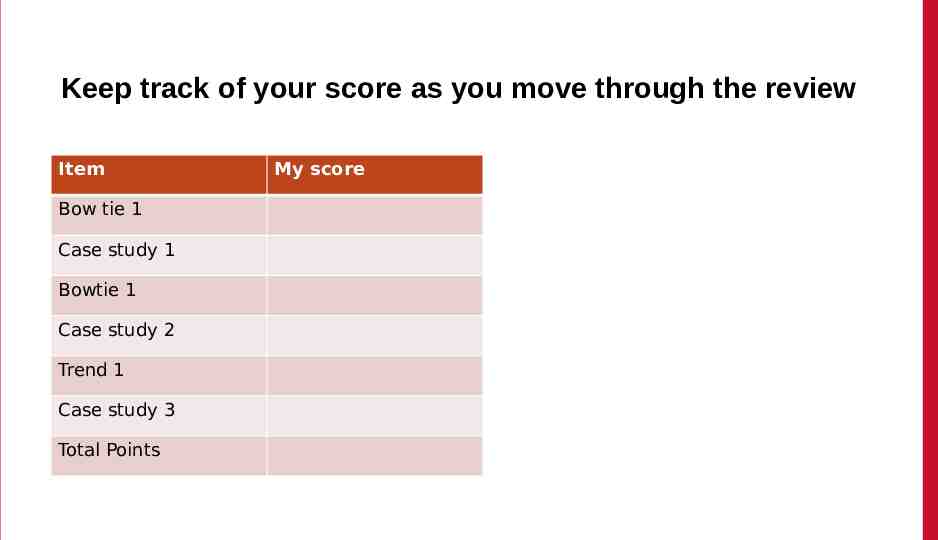
Keep track of your score as you move through the review Item Bow tie 1 Case study 1 Bowtie 1 Case study 2 Trend 1 Case study 3 Total Points My score
Final Link The final link in the review takes you to the course evaluation. This anonymous information will be used to help us understand how this review is being used and how to improve the experience.
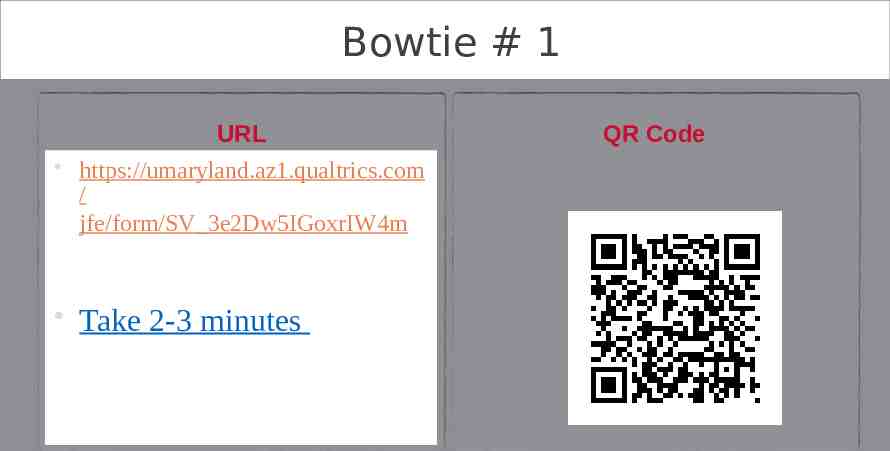
Bowtie # 1 URL https://umaryland.az1.qualtrics.com / jfe/form/SV 3e2Dw5IGoxrIW4m Take 2-3 minutes QR Code
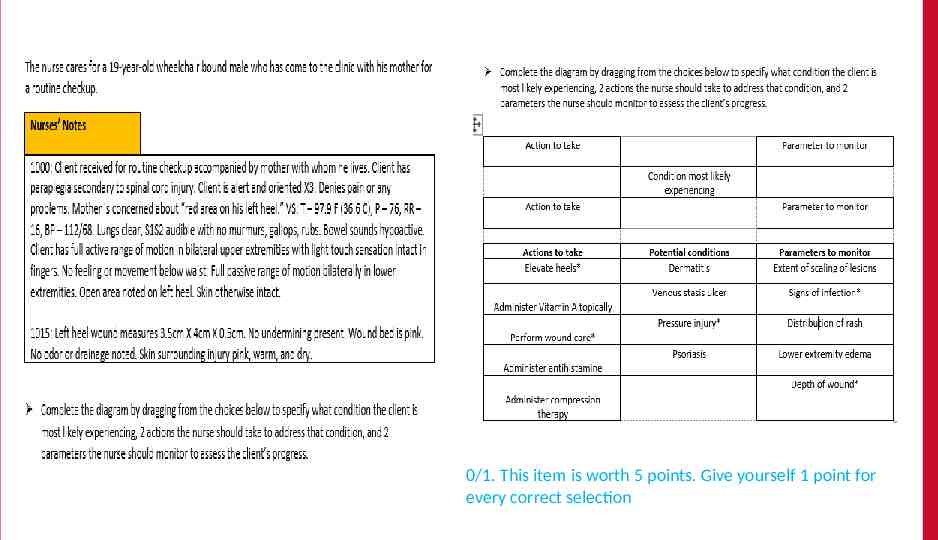
0/1. This item is worth 5 points. Give yourself 1 point for every correct selection
Rationale The assessment data (location over bony prominence, shallow wound, surrounding skin within normal parameters) indicates a stage II pressure injury. Wound care will facilitate healing and elevating the heels while in bed will relieve direct pressure. The wound should be monitored for signs of infection. A decrease in wound depth would indicate that the pressure injury was improving.
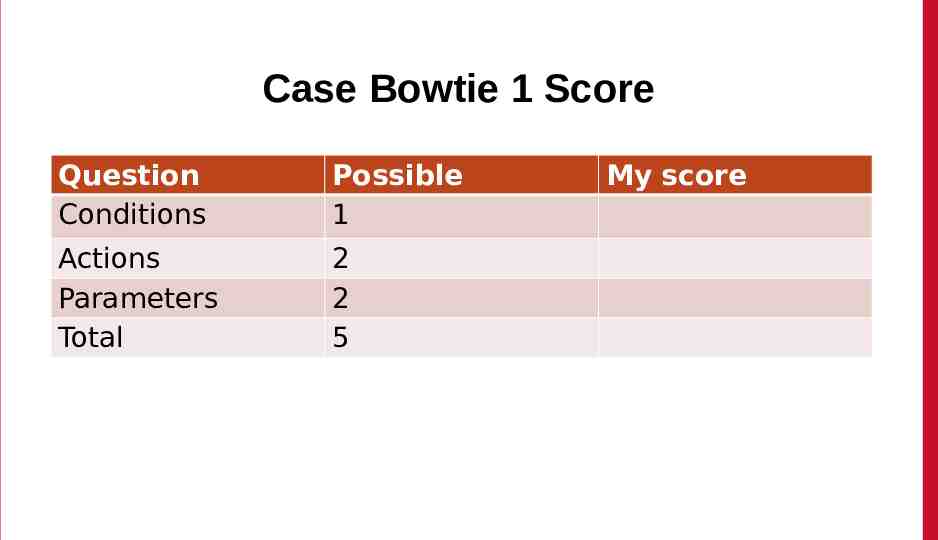
Case Bowtie 1 Score Question Conditions Possible 1 Actions Parameters Total 2 2 5 My score
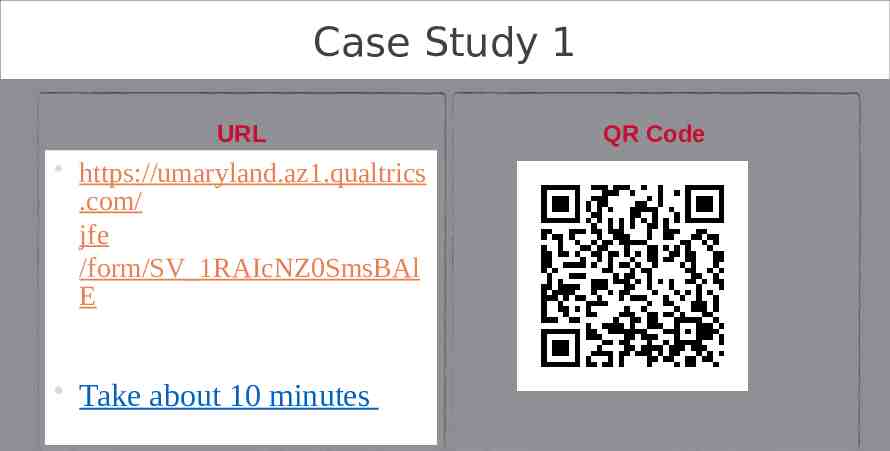
Case Study 1 URL https://umaryland.az1.qualtrics .com/ jfe /form/SV 1RAIcNZ0SmsBAl E Take about 10 minutes QR Code
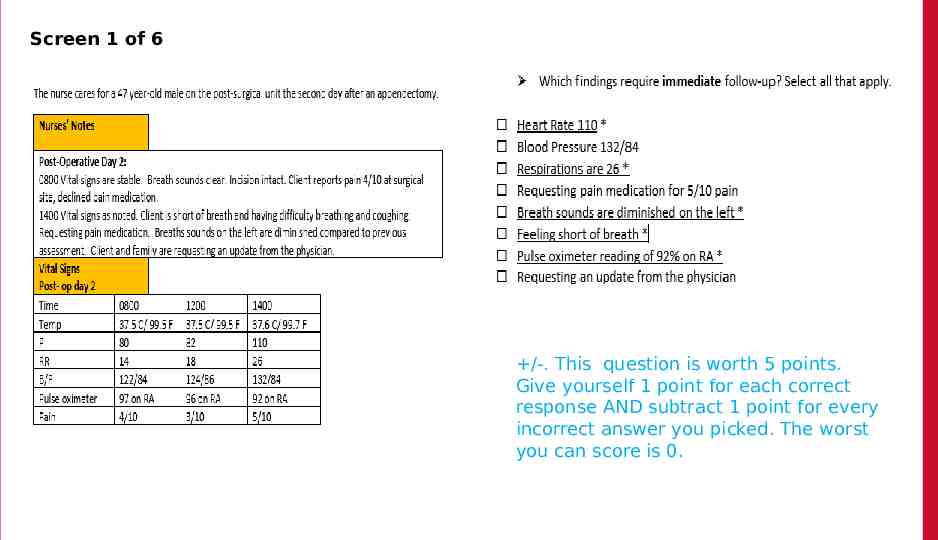
Screen 1 of 6 /-. This question is worth 5 points. Give yourself 1 point for each correct response AND subtract 1 point for every incorrect answer you picked. The worst you can score is 0.
Rationale The nurse should identify signs and symptoms of post-operative complications that need to be addressed. Signs of atelectasis include increased heart rate, increased respirations, breathing difficulties and low oxygen levels. Breath sounds will be diminished due to collapsed alveoli. Blood pressure is not affected unless it becomes elevated due to the stress of breathing difficulties. Pain medication is important but first the breathing issues must be addressed.
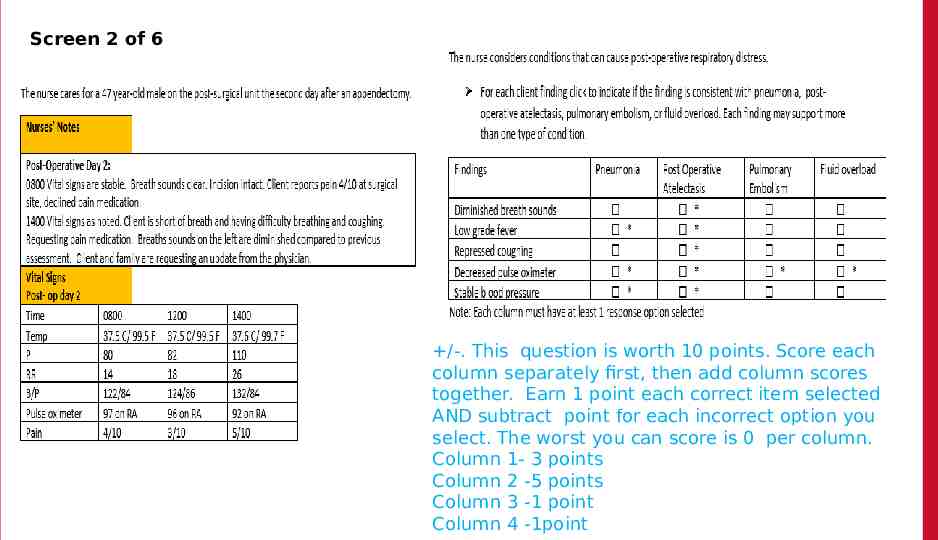
Screen 2 of 6 /-. This question is worth 10 points. Score each column separately first, then add column scores together. Earn 1 point each correct item selected AND subtract point for each incorrect option you select. The worst you can score is 0 per column. Column 1- 3 points Column 2 -5 points Column 3 -1 point Column 4 -1point
Rationale The nurse should differentiate signs and symptoms of atelectasis, pneumonia, pulmonary embolism, and fluid overload in clients with respiratory distress following surgery. All respiratory issues include shortness of breath and increased respirations, and decreased pulse oximeter readings. Diminished breath sounds and repressed coughing are most associated with post-op atelectasis. Coughing, rhonchi, wheezing, or crackles would be expected with the other three conditions. Low-grade fever and normal and stable blood pressures would be expected with atelectasis and pneumonia. Fever could also be higher with pneumonia. Unstable blood pressures would be expected for pulmonary embolism or fluid overload. Hypotension is typically seen with pulmonary embolism. Hypertension is associated with fluid overload.
Screen 3 of 6 0/1. This question is worth 1 point. Give yourself 1 point if you answered correctly.
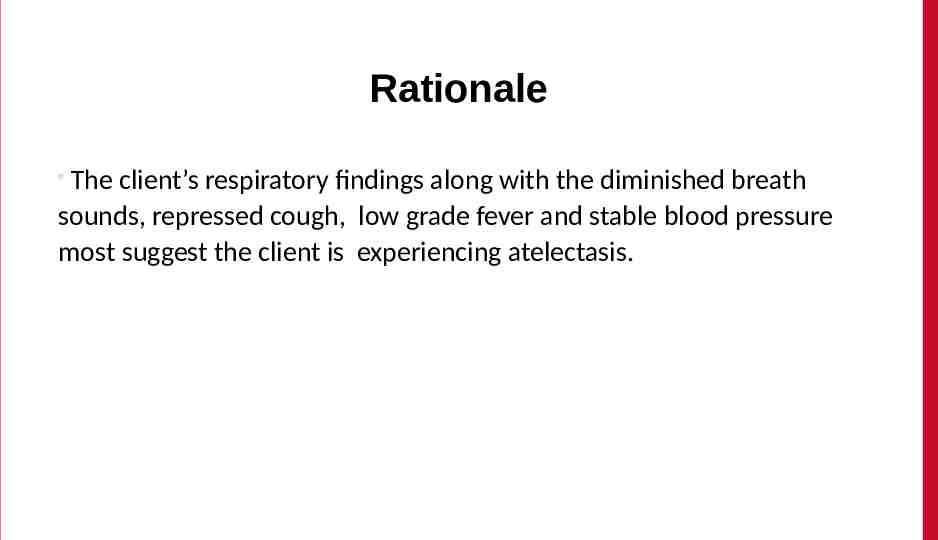
Rationale The client’s respiratory findings along with the diminished breath sounds, repressed cough, low grade fever and stable blood pressure most suggest the client is experiencing atelectasis.
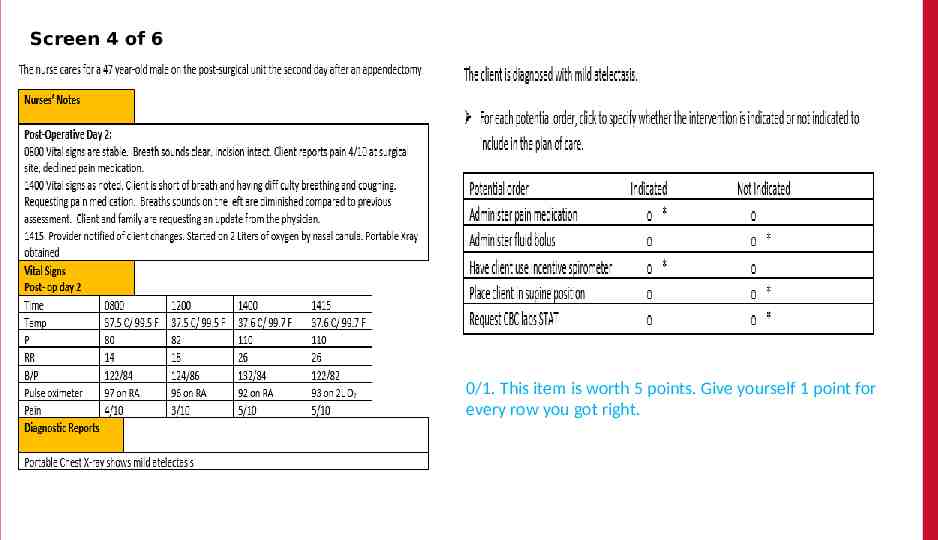
Screen 4 of 6 0/1. This item is worth 5 points. Give yourself 1 point for every row you got right.
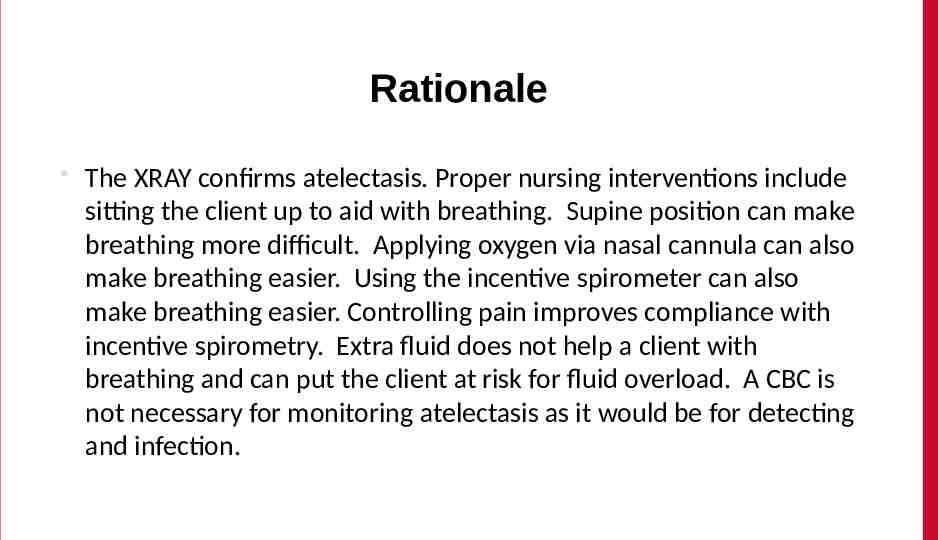
Rationale The XRAY confirms atelectasis. Proper nursing interventions include sitting the client up to aid with breathing. Supine position can make breathing more difficult. Applying oxygen via nasal cannula can also make breathing easier. Using the incentive spirometer can also make breathing easier. Controlling pain improves compliance with incentive spirometry. Extra fluid does not help a client with breathing and can put the client at risk for fluid overload. A CBC is not necessary for monitoring atelectasis as it would be for detecting and infection.
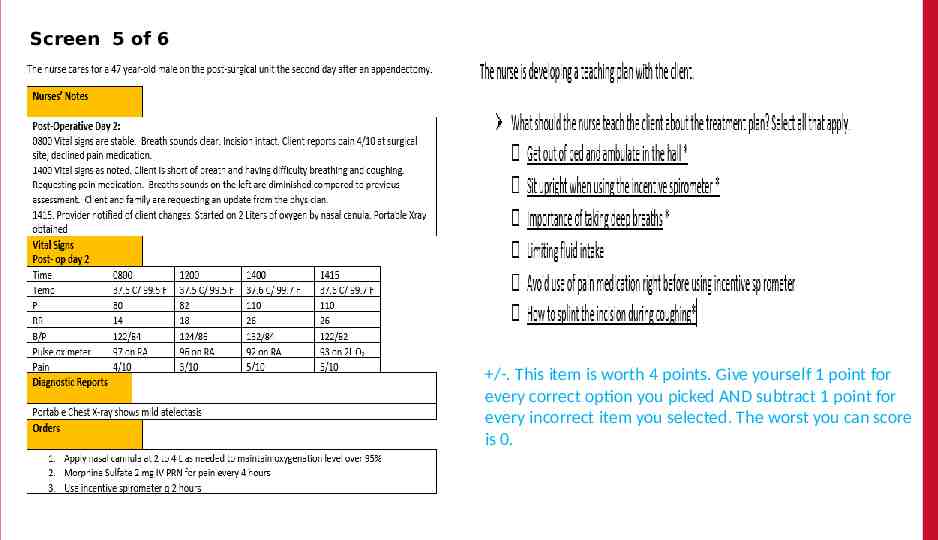
Screen 5 of 6 The /-. This item is worth 4 points. Give yourself 1 point for every correct option you picked AND subtract 1 point for every incorrect item you selected. The worst you can score is 0.
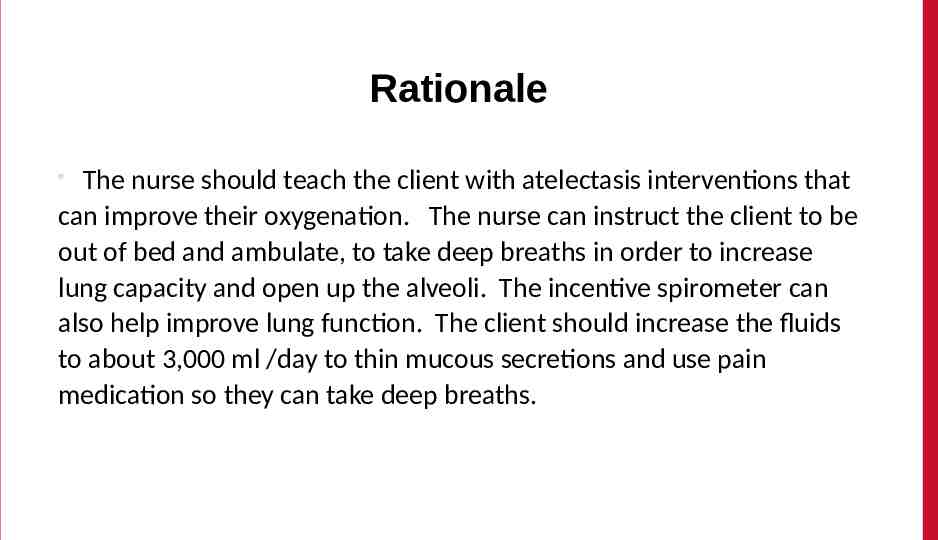
Rationale The nurse should teach the client with atelectasis interventions that can improve their oxygenation. The nurse can instruct the client to be out of bed and ambulate, to take deep breaths in order to increase lung capacity and open up the alveoli. The incentive spirometer can also help improve lung function. The client should increase the fluids to about 3,000 ml /day to thin mucous secretions and use pain medication so they can take deep breaths.
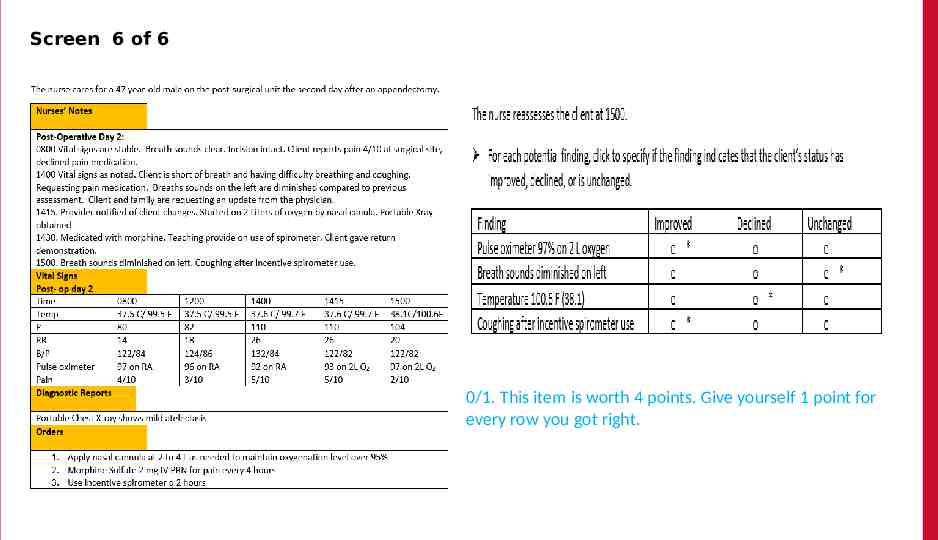
Screen 6 of 6 The 0/1. This item is worth 4 points. Give yourself 1 point for every row you got right.
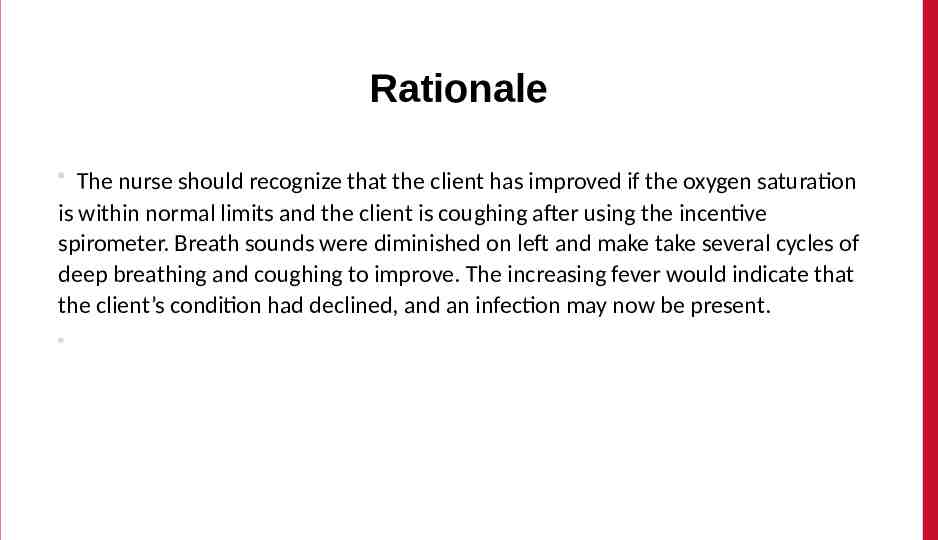
Rationale The nurse should recognize that the client has improved if the oxygen saturation is within normal limits and the client is coughing after using the incentive spirometer. Breath sounds were diminished on left and make take several cycles of deep breathing and coughing to improve. The increasing fever would indicate that the client’s condition had declined, and an infection may now be present.
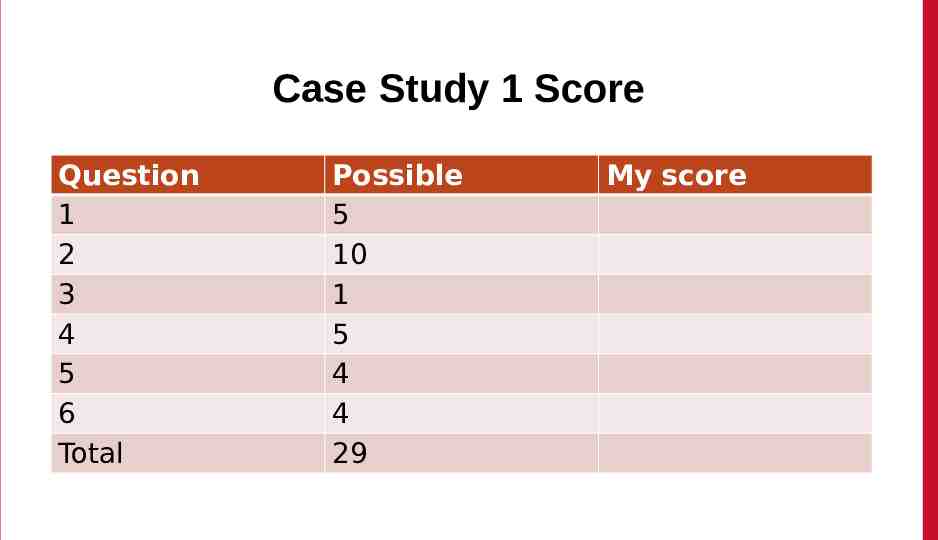
Case Study 1 Score Question 1 2 3 4 5 6 Total Possible 5 10 1 5 4 4 29 My score
Bowtie # 2 URL https://umaryland.az1.qualtrics.com / jfe/form/SV 4VMW6Rt7x79A9E2 Take 2-3 minutes QR Code
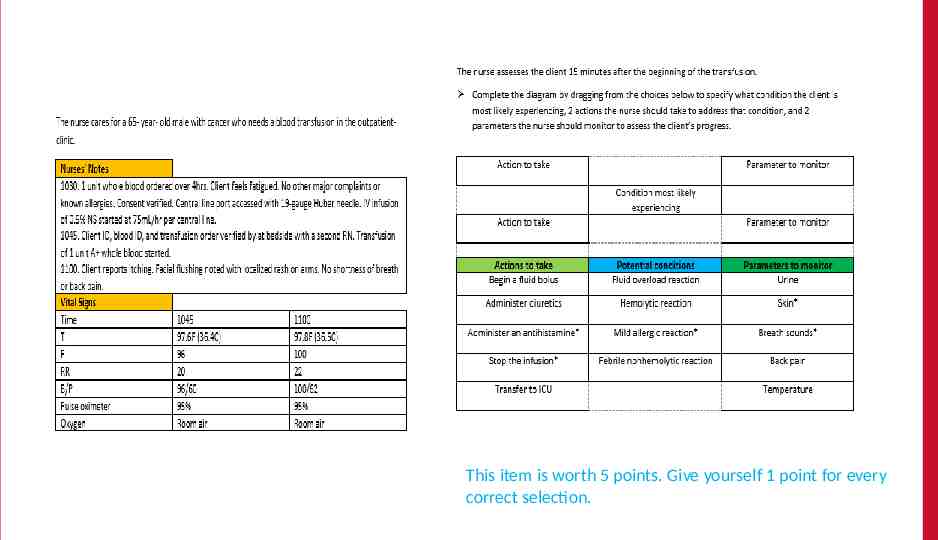
This item is worth 5 points. Give yourself 1 point for every correct selection.
Rationale Based on the stable vital signs with skin changes, the nurse would most suspect that the client is having a mild allergic reaction to a foreign protein in the donor blood. The nurse should stop the transfusion and administer and antihistamine. The nurse would monitor the skin for improvement and the breaths sounds to ensure the allergic reaction is continuing to be mild versus anaphylaxis.
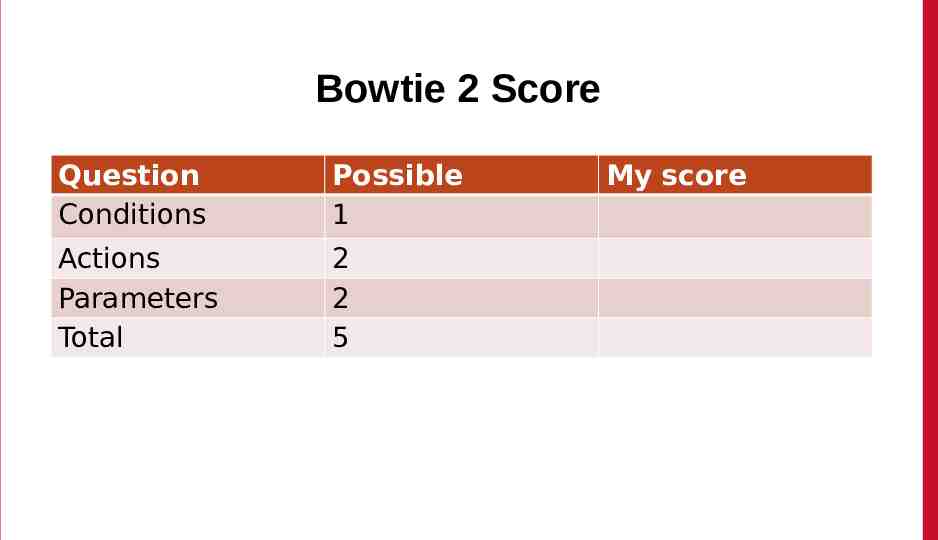
Bowtie 2 Score Question Conditions Possible 1 Actions Parameters Total 2 2 5 My score
Case Study # 2 URL https://umaryland.az1.qualtrics .com/ jfe /form/SV 6SuLbW1OlWYay4 S Take about 10 minutes QR Code
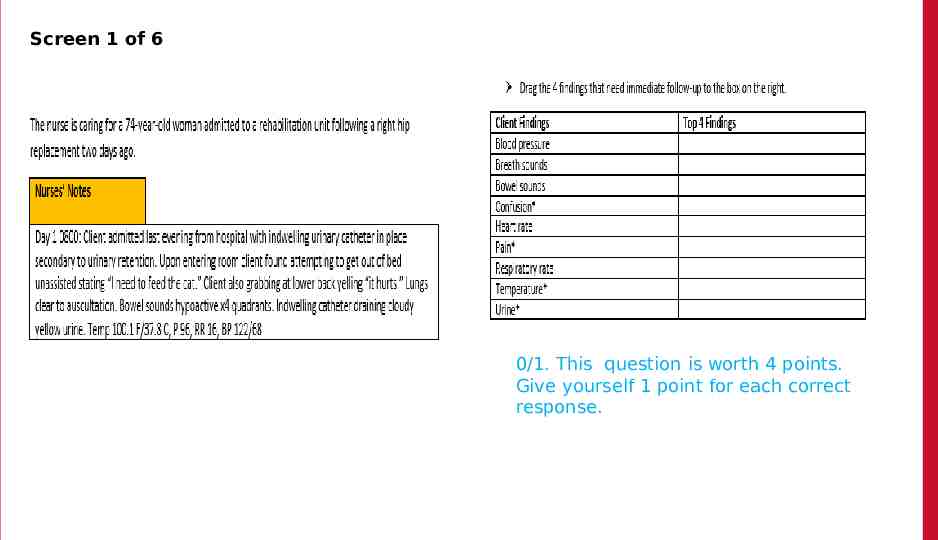
Screen 1 of 6 0/1. This question is worth 4 points. Give yourself 1 point for each correct response.
Rationale Vital signs, with exception of temperature heart rate, are similar to baseline. Heart rate, while elevated, is still within normal parameters and may be the result of the fever. Confusion, fever, cloudy urine, and lower back pain are new symptoms.
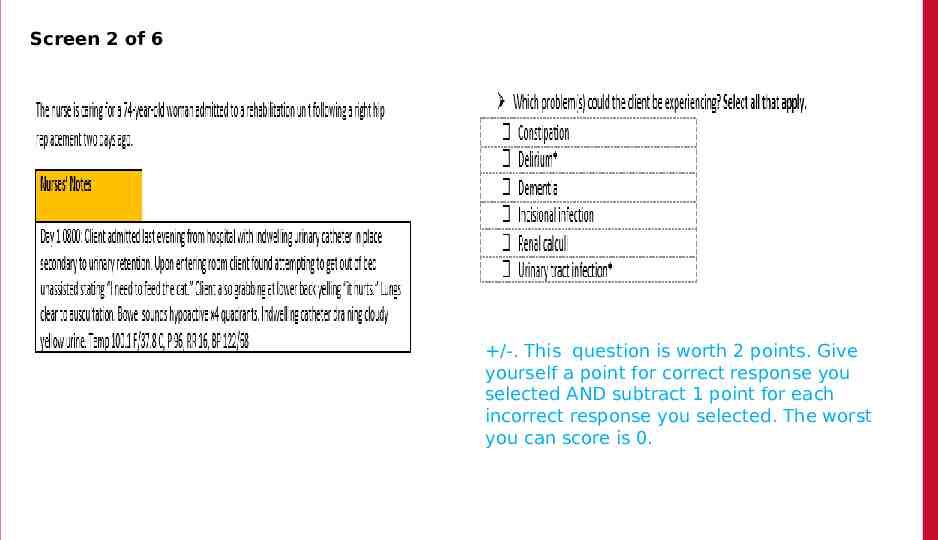
Screen 2 of 6 /-. This question is worth 2 points. Give yourself a point for correct response you selected AND subtract 1 point for each incorrect response you selected. The worst you can score is 0.
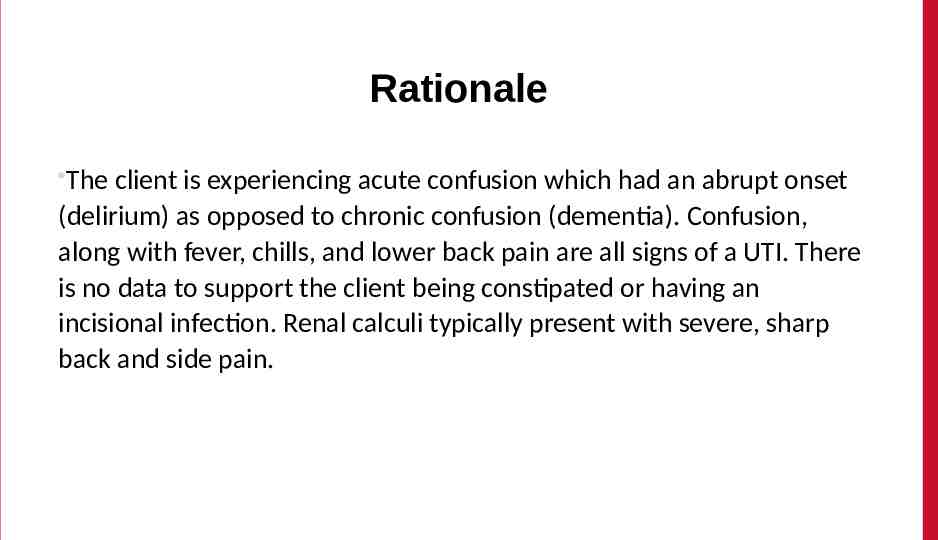
Rationale The client is experiencing acute confusion which had an abrupt onset (delirium) as opposed to chronic confusion (dementia). Confusion, along with fever, chills, and lower back pain are all signs of a UTI. There is no data to support the client being constipated or having an incisional infection. Renal calculi typically present with severe, sharp back and side pain.
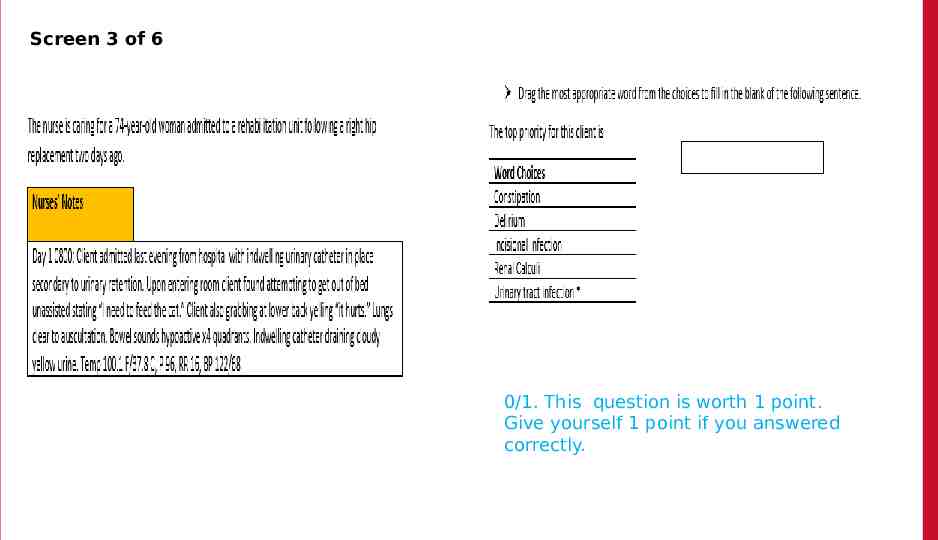
Screen 3 of 6 0/1. This question is worth 1 point. Give yourself 1 point if you answered correctly.
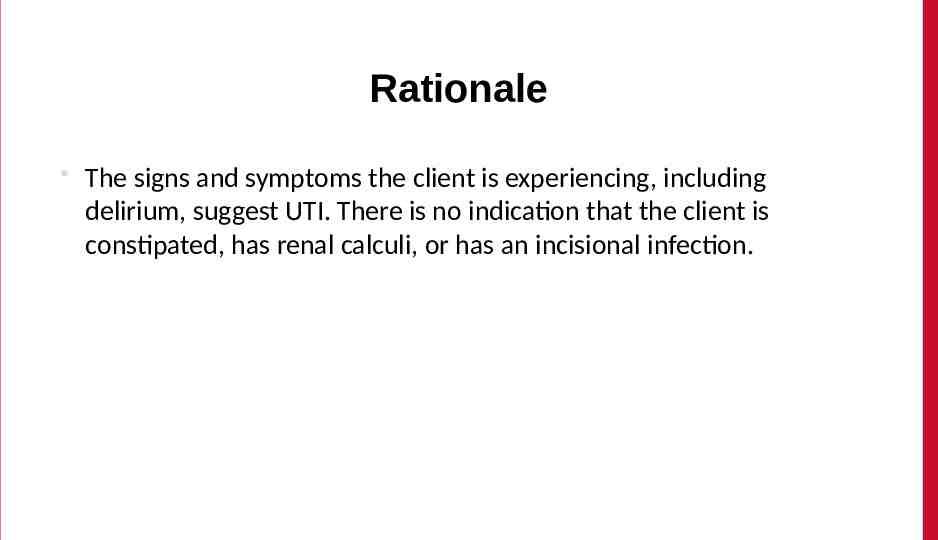
Rationale The signs and symptoms the client is experiencing, including delirium, suggest UTI. There is no indication that the client is constipated, has renal calculi, or has an incisional infection.
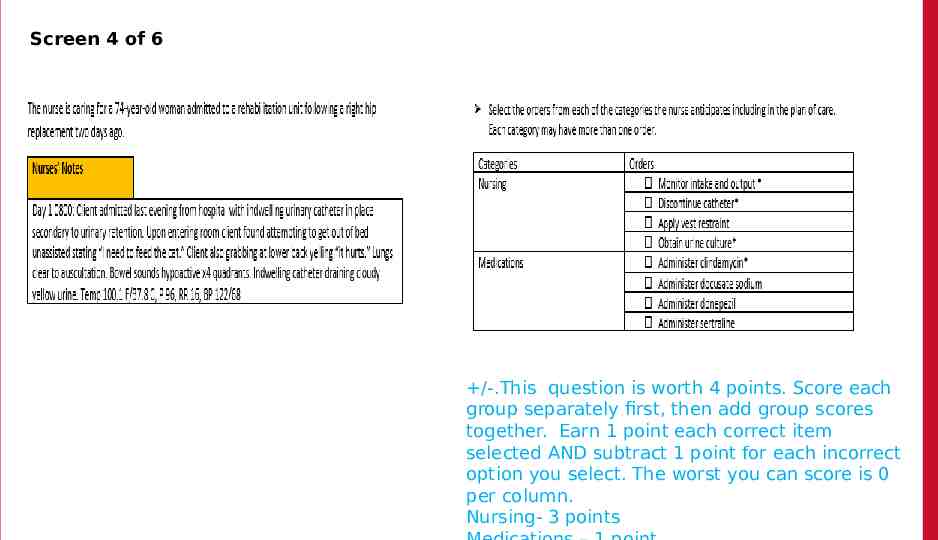
Screen 4 of 6 /-.This question is worth 4 points. Score each group separately first, then add group scores together. Earn 1 point each correct item selected AND subtract 1 point for each incorrect option you select. The worst you can score is 0 per column. Nursing- 3 points
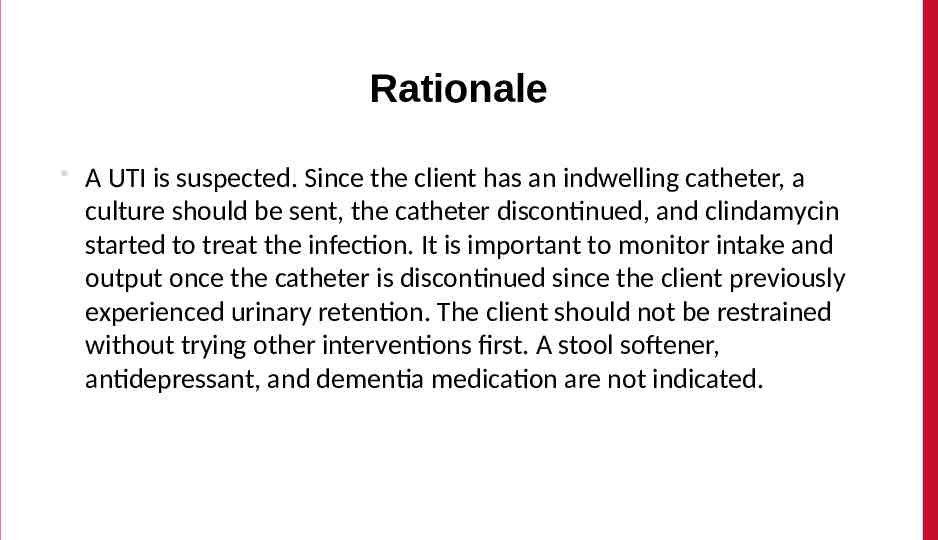
Rationale A UTI is suspected. Since the client has an indwelling catheter, a culture should be sent, the catheter discontinued, and clindamycin started to treat the infection. It is important to monitor intake and output once the catheter is discontinued since the client previously experienced urinary retention. The client should not be restrained without trying other interventions first. A stool softener, antidepressant, and dementia medication are not indicated.
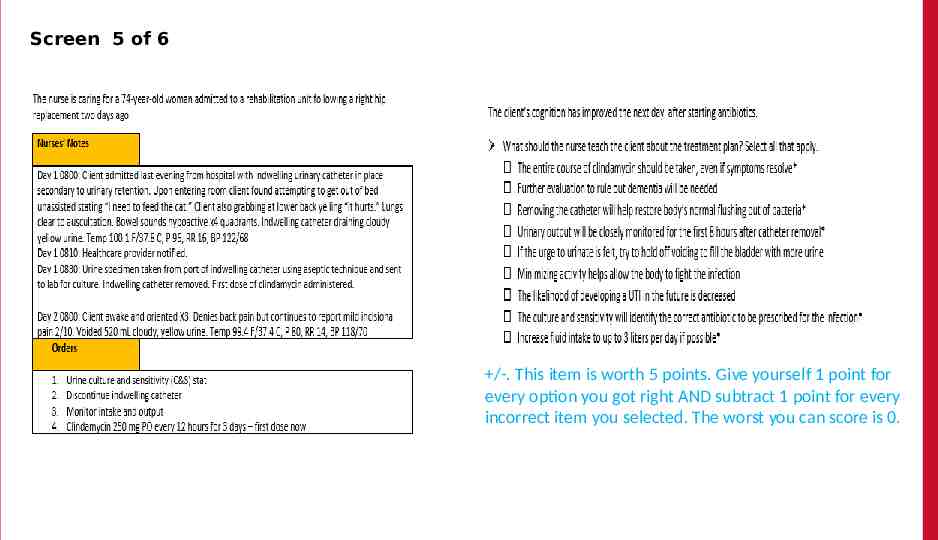
Screen 5 of 6 The /-. This item is worth 5 points. Give yourself 1 point for every option you got right AND subtract 1 point for every incorrect item you selected. The worst you can score is 0.
Rationale The client likely has CAUTI. Sending a C&S will determine 1) if there is an infection and 2) if the appropriate antibiotic is prescribed. Removing the catheter eliminates the mode of transmission and helps to restore the body’s natural flushing out of bacteria. Increased fluid intake will also help to flush out the bacteria. The full course of antibiotics should be taken even if symptoms resolve. The nurse should monitor the client’s voiding pattern to identify potential urinary retention. Evaluation for dementia is not necessary as the client likely had delirium because of the UTI. The client should void when the urge is felt as bacteria can multiply when holding urine.
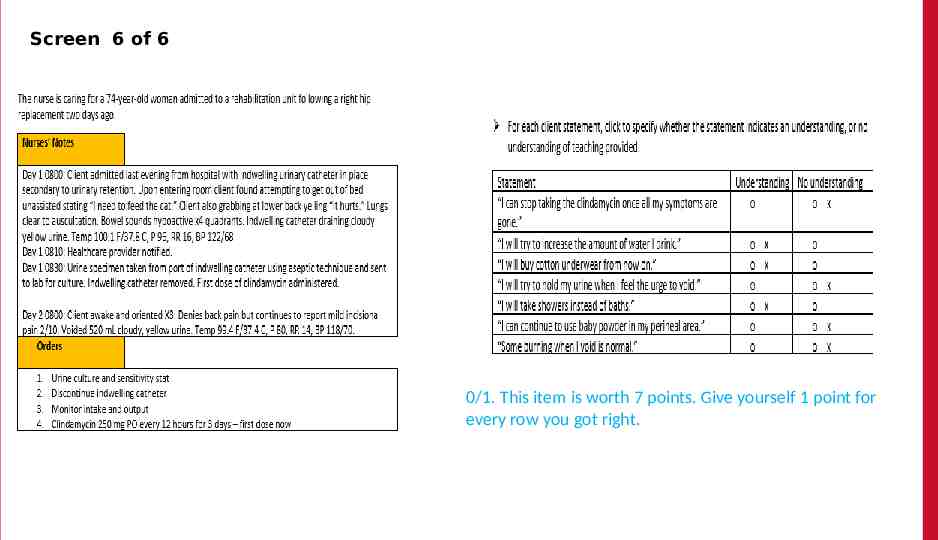
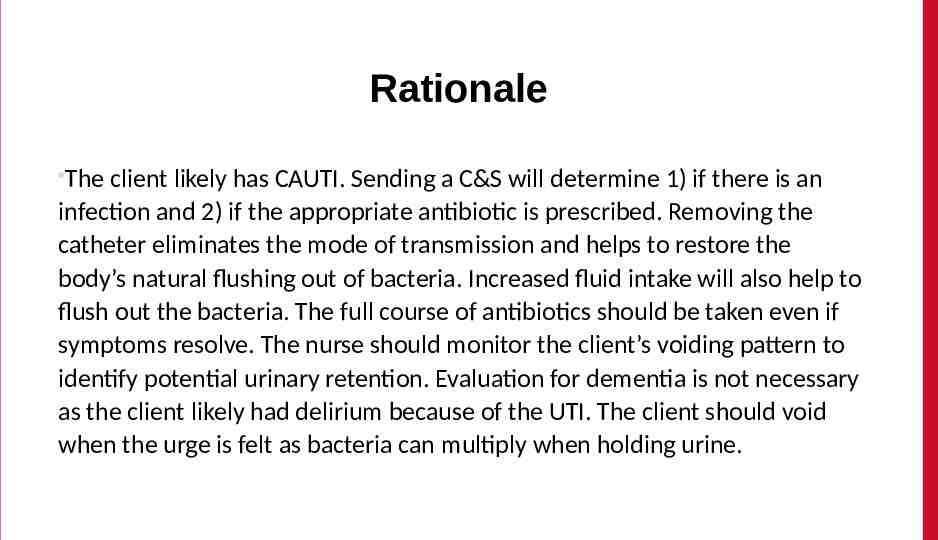
Screen 6 of 6 The 0/1. This item is worth 7 points. Give yourself 1 point for every row you got right.
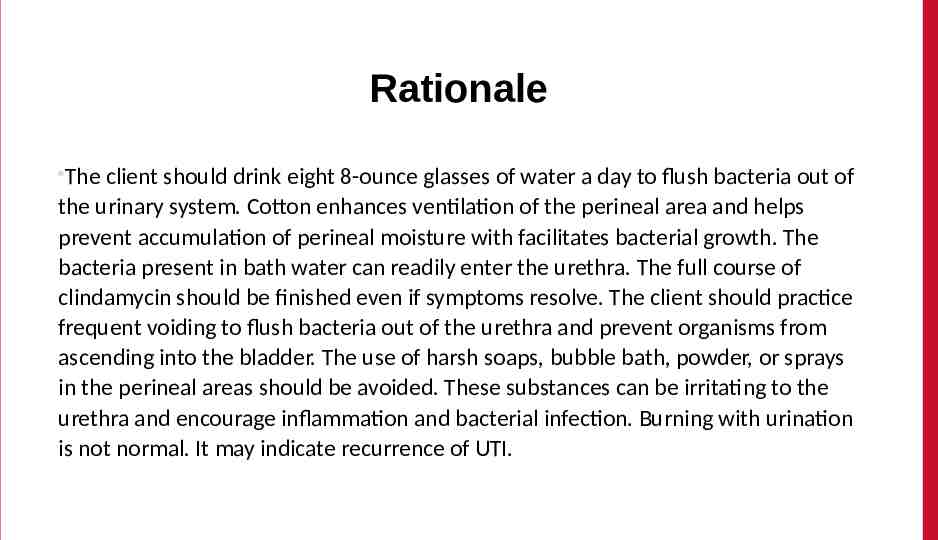
Rationale The client should drink eight 8-ounce glasses of water a day to flush bacteria out of the urinary system. Cotton enhances ventilation of the perineal area and helps prevent accumulation of perineal moisture with facilitates bacterial growth. The bacteria present in bath water can readily enter the urethra. The full course of clindamycin should be finished even if symptoms resolve. The client should practice frequent voiding to flush bacteria out of the urethra and prevent organisms from ascending into the bladder. The use of harsh soaps, bubble bath, powder, or sprays in the perineal areas should be avoided. These substances can be irritating to the urethra and encourage inflammation and bacterial infection. Burning with urination is not normal. It may indicate recurrence of UTI.
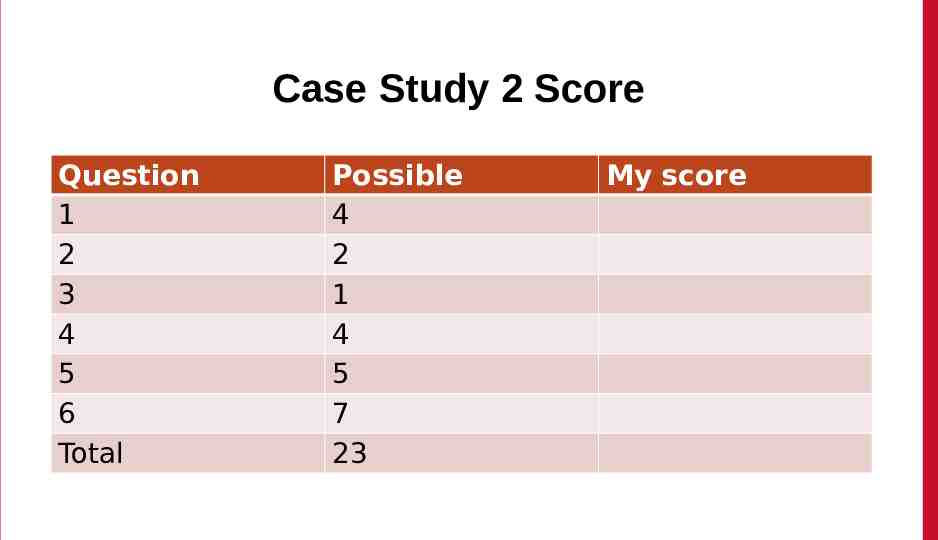
Case Study 2 Score Question 1 2 3 4 5 6 Total Possible 4 2 1 4 5 7 23 My score

Trend # 1 URL https://umaryland.az1.qualtrics.com / jfe/form/SV efcwkK8NCyL231Y Take 2-3 minutes QR Code
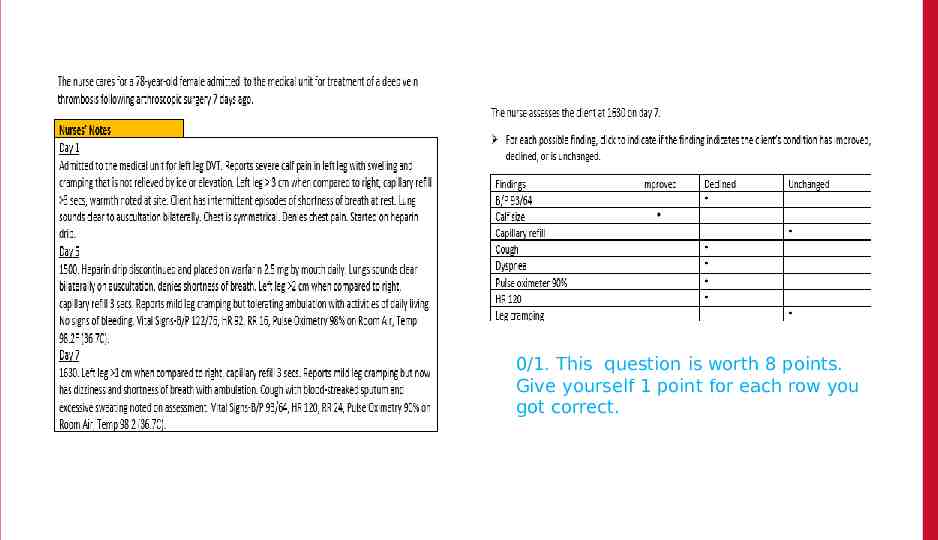
0/1. This question is worth 8 points. Give yourself 1 point for each row you got correct.
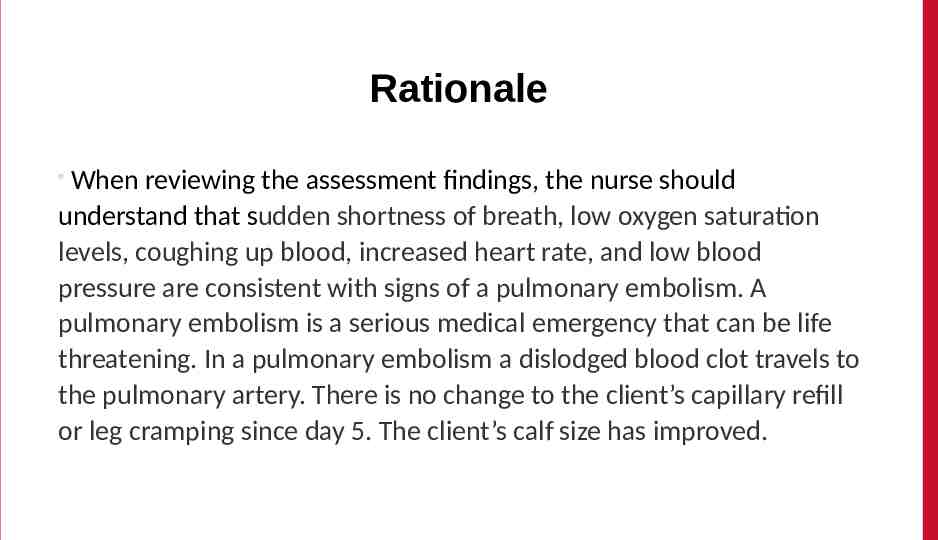
Rationale When reviewing the assessment findings, the nurse should understand that sudden shortness of breath, low oxygen saturation levels, coughing up blood, increased heart rate, and low blood pressure are consistent with signs of a pulmonary embolism. A pulmonary embolism is a serious medical emergency that can be life threatening. In a pulmonary embolism a dislodged blood clot travels to the pulmonary artery. There is no change to the client’s capillary refill or leg cramping since day 5. The client’s calf size has improved.
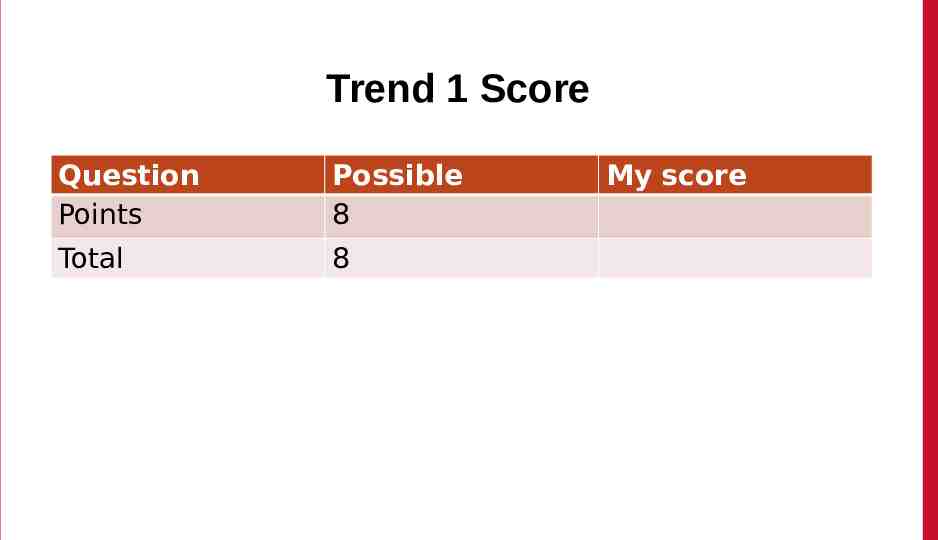
Trend 1 Score Question Points Possible 8 Total 8 My score
Case Study # 3 URL https://umaryland.az1.qualtrics.com / jfe/form/SV 5dt5N3y7rCEg7mS Take about 10 minutes QR Code
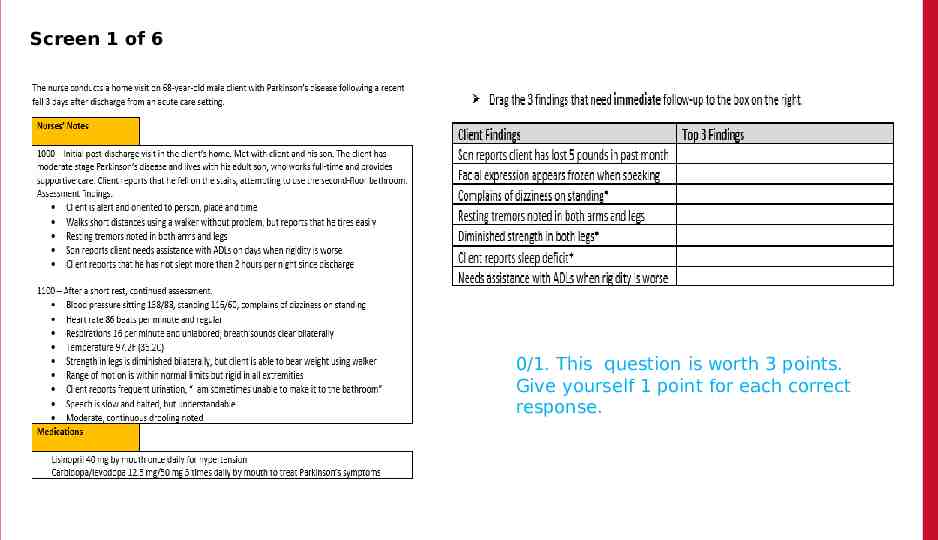
Screen 1 of 6 0/1. This question is worth 3 points. Give yourself 1 point for each correct response.
Rationale Dizziness is symptom related to orthostatic hypotension and can be a side effect of lisinopril. This puts the client at increased risk for falls. Sleep disturbance is not a normal part of aging and needs additional assessment, as fatigue can increase fall risk. The diminished strength in the client’s legs also increases his risk for falls.
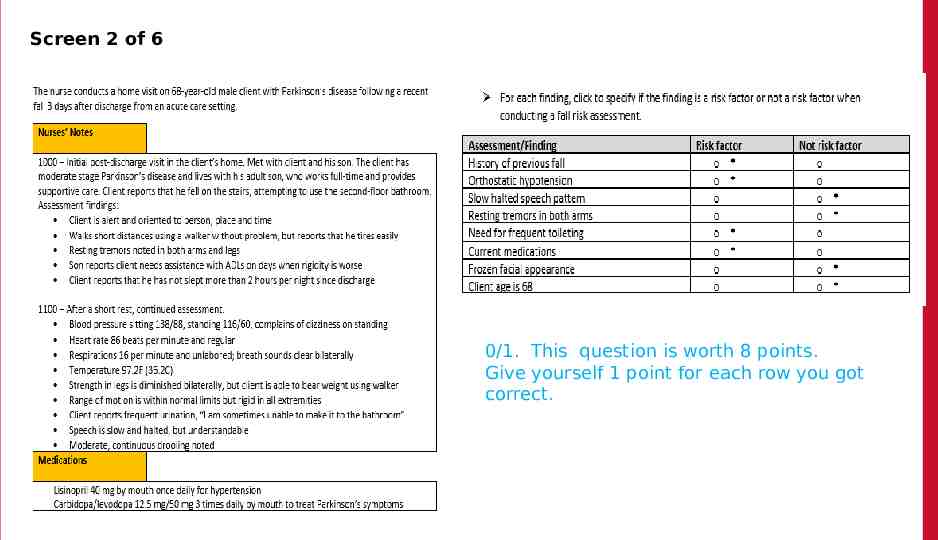
Screen 2 of 6 0/1. This question is worth 8 points. Give yourself 1 point for each row you got correct.
Rationale Medications causing orthostatic hypotension may increase the risk for falls, need for frequent toileting increases need for mobility and use of stairs, history of a fall is a known risk factor for additional falls; advanced age, 80, is considered a fall risk.
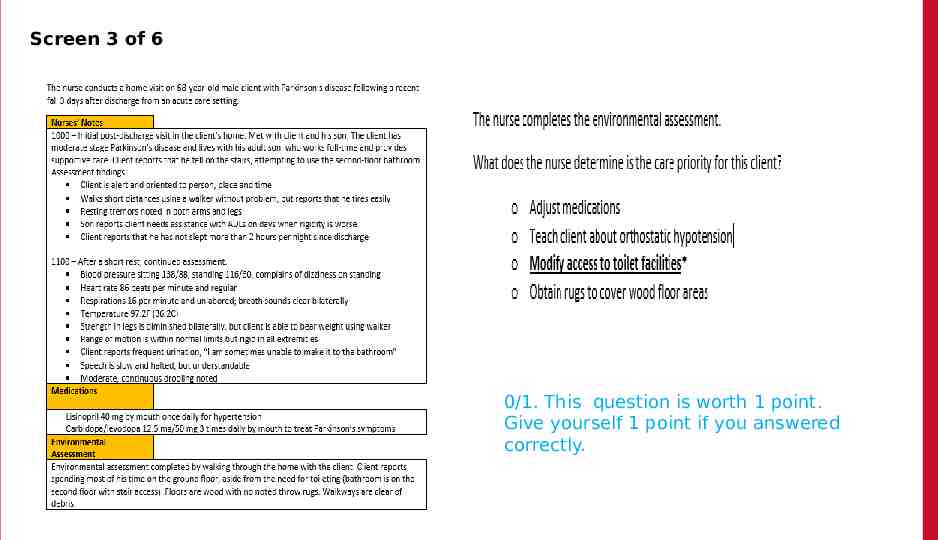
Screen 3 of 6 0/1. This question is worth 1 point. Give yourself 1 point if you answered correctly.
Rationale Modifying access to toilet facilities will address the client’s only need to use the stairs and reduce his risk for falls. This is an intervention that will increase client’s quality of life and have limited associated expense.
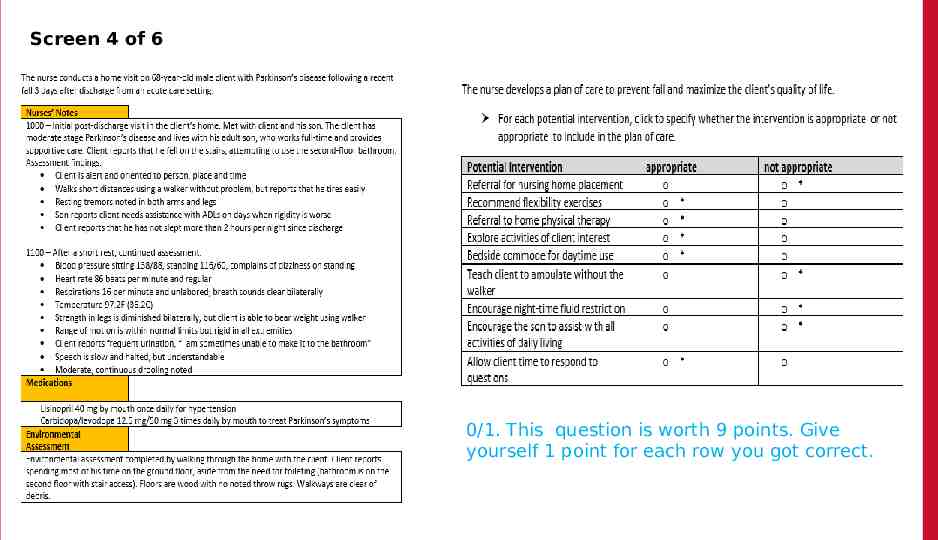
Screen 4 of 6 0/1. This question is worth 9 points. Give yourself 1 point for each row you got correct.
Rationale The client is not ready for extended care facility placement. Flexibility exercises, such as yoga or tai chi, will help promote range-of-motions and balance. Home physical therapy will help maintain strength and flexibility. A bedside commode will enable the client to use the toilet without climbing stairs. Exploring activities of interest and allowing the client time to respond to questions will help keep client engaged and prevent social isolation. A fluid restriction is not indicated, based on signs of dehydration. Promoting as much independence as possible in self-care is important to client self-esteem. Due to client’s decreased strength and orthostatic hypotension, he should be encouraged to use the walker when ambulating.
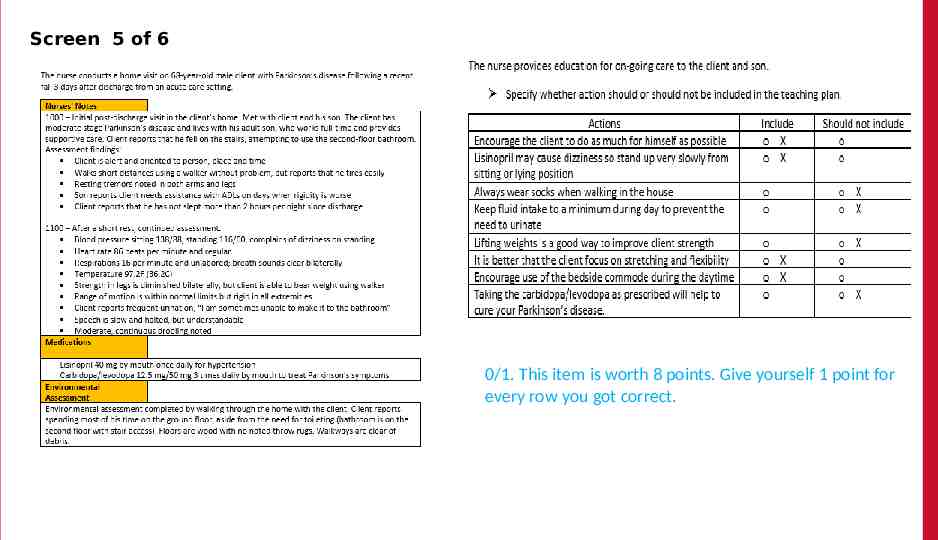
Screen 5 of 6 The 0/1. This item is worth 8 points. Give yourself 1 point for every row you got correct.
Rationale Clients with Parkinson’s disease should be encouraged to participate in self-care for as long as possible. This helps with both motor skills and self-esteem. Lisinopril can cause orthostatic hypotension, so instruction on standing up slowly is important. Wearing socks on the wood floor increases the risk for falls. Instead, the client should always wear shoes. Making the toilet more accessible is a healthier option to decreasing fluid because dehydration can contribute to the risk for falls. Weightlifting is not considered a safe activity for clients with decreased strength. Focus on flexibility and stretching is more beneficial that strength training in Parkinson’s disease. Using the bedside commode is a safety intervention to prevent the use of stairs when unattended. Parkinson’s disease is a progressive degenerative disease that will not be cured by medication. Carbidopa/levodopa can help with symptoms of shakiness and trouble moving, but will not prevent disease progression.
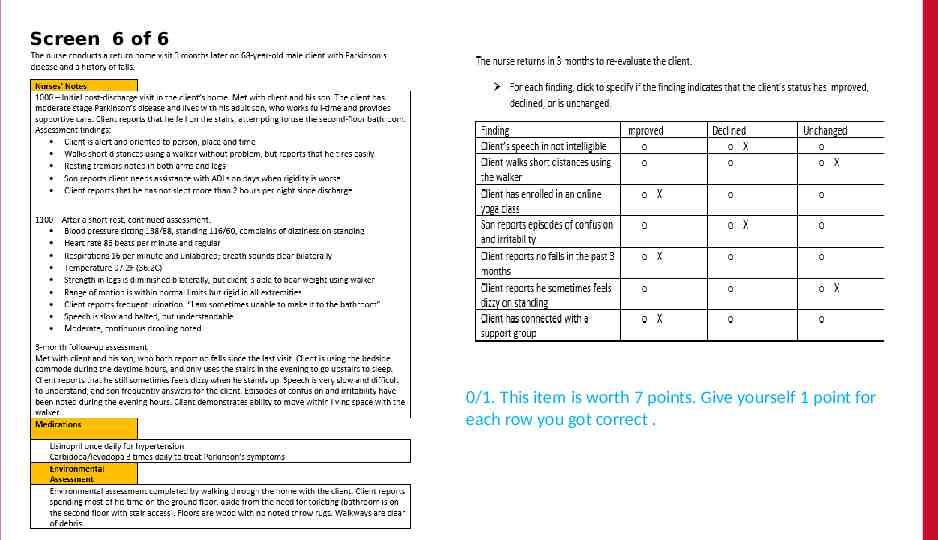
Screen 6 of 6 The 0/1. This item is worth 7 points. Give yourself 1 point for each row you got correct .
Rationale Changes in cognition such as confusion and irritability and declining speech capability are signs of progressing disease. No fall shows in 3 months shows interventions have been effective. Joining a support group and an online yoga class demonstrate an understanding of disease progression and positive interventions. The client was using a walker and had dizziness upon standing at the initial visit.
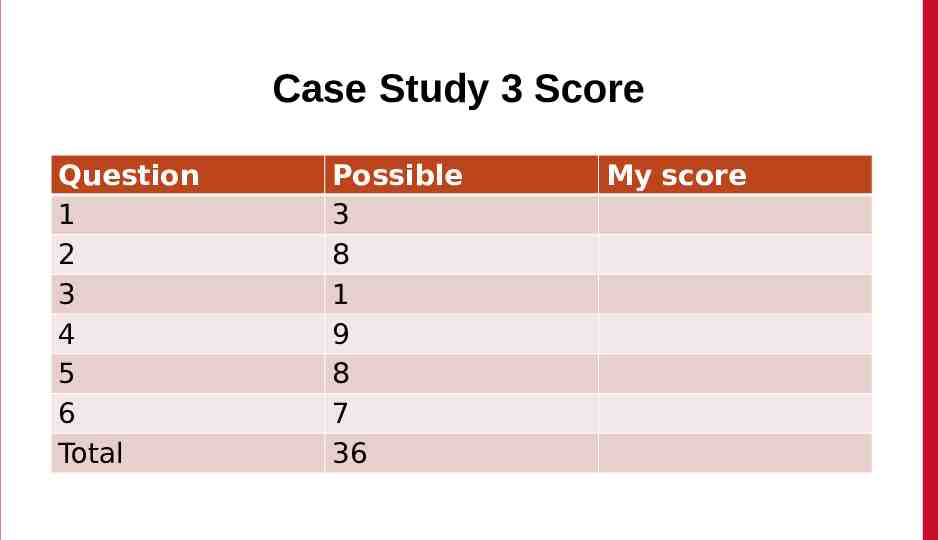
Case Study 3 Score Question 1 2 3 4 5 6 Total Possible 3 8 1 9 8 7 36 My score
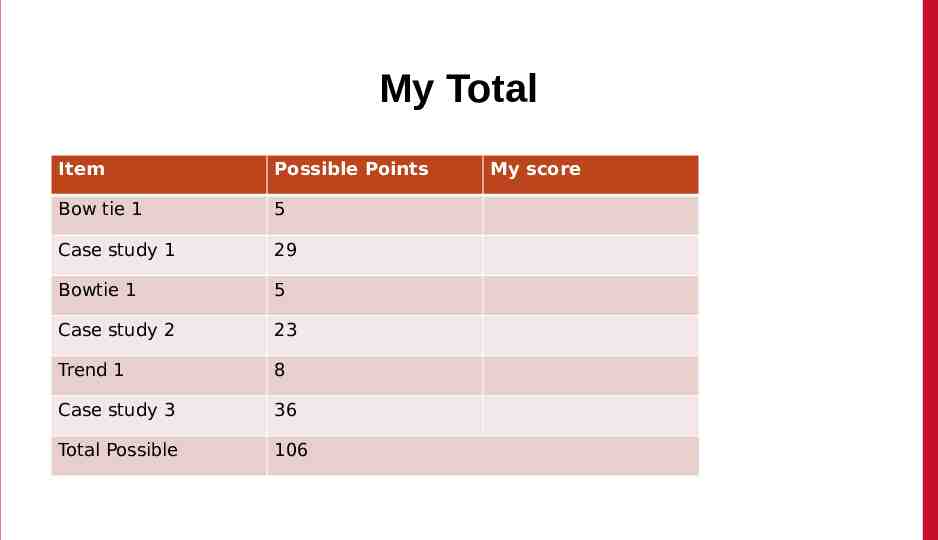
My Total Item Possible Points Bow tie 1 5 Case study 1 29 Bowtie 1 5 Case study 2 23 Trend 1 8 Case study 3 36 Total Possible 106 My score
Please Complete the Mini Review Evaluation https://umaryland.az1.qua ltrics.com/ jfe /form/SV 1ZYu3gxvlMDzi MS This evaluation will take approximately less than 2 minutes to complete.