India and Acute Malnutrition in Children Veena Shatrugna
57 Slides1.49 MB
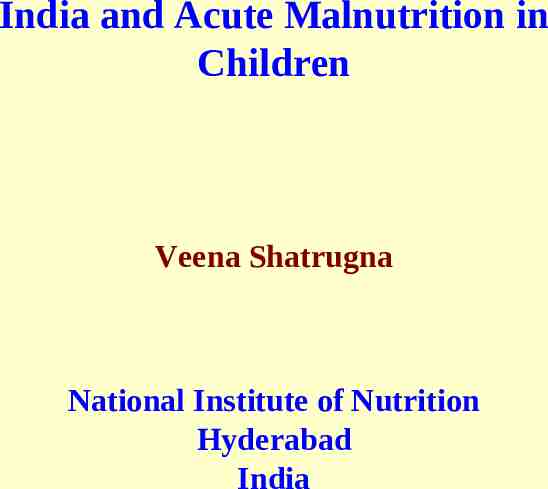
India and Acute Malnutrition in Children Veena Shatrugna National Institute of Nutrition Hyderabad India

-1- Absolute Weights – A 30 year trend (Mean in Kg) Rural Rural 1977 Rural 1996 Rural 2003 NCHS Median 2006 Values Age F M 01 7.5 8.1 8.1 8.7 8.1 8.6 8.3 10.6 10.4 11.3 11.7 11.4 11.9 11.8 13.7 14.1 13.6 14.4 14.1 14.6 22.0 21.6 22.4 22.6 23.1 42.9 48.1 43.5 50.3 43.8 10.2 F M F M F M F M 8.9 9.5 (219-920) 03 12.1 14.1 14.6 (218-916) 05 18.7 14.5 14.7 17.7 23.1 23.9 23.9 32.5 50.9 45.0 56.6 (229-747) 10 31.4 (304-734) 20-24 68.9 (509-3870) 52.2

-2Absolute Heights – A 30 year trend (Mean in cm) Median Values Age Rural 1977 F Rural 1996 M F Rural 2003 M F Rural 2006 M F NCHS M F M 01 71.9 76.1 73.1 72.8 75.0 73.8 75.3 74.0 75.7 74.3 (219-920) 3 85.8 86.4 88.4 90.1 89.8 91.1 89.9 91.1 93.9 94.9 (218-916) 05 109.9 99.6 100.5 100.4 102.1 102.5 103.2 102.4 102.6 108.4 125.7 125.1 126.8 127.9 128.5 128.7 128.9 129.0 138.3 151.2 163.4 151.5 164.0 152.0 164.2 163.7 (229-747) 10 137.5 (304-734) 20-24 176.8 (509-3870) 151.1 163.3

-3% DISTRIBUTION OF ADULTS ACCORDING TO BMI CLASSIFICATION 20 YEAR TREND BMI CLASSES 18.5 (CED) (NORMAL) 1974‑79* (RURAL) 1988‑90* (RURAL) 1996-97** (RURAL) 1993‑94*** (URBAN) 2002* (RURAL) F 51.8 49.3 47.7 36.7 M 55.6 49.0 45.5 42.8 F 44.8 M 42.1 48.3 50.4 51.8 57.2 F 3.4 4.1 6.3 11.6 8.7 M 2.3 2.7 4.1 5.5 6.2 46.6 46.3 38.9 36.6 51.7 52.4 18.5‑25.0 (OBESE) 25 * * NNMB, 1991, quoted by N,Nadamuni Naidu et al, 1994. Rural, 2002

-4a- % DISTRIBUTION OF ADULTS ACCORDING TO BMI CLASSIFICATION - NNMB 2006 16 16-17 (CED III) (CED II) 17-18.5 18.5-20 (CED I) (Low Wt. 20-25 25 (Normal) (Over wt.) Normal) Men 5.7 Women 8.0 7.9 9.0 19.6 21.7 37.3 7.0 19.0 18.7 34.4 9.1

- 4b - Distribution (%) of Adults According to BMI Classification 10 year trend BMI Males Males Females 1996 2006 8.6 5.7 11.8 8.0 16.0-17.0 11.0 7.9 12.8 9.0 17.0-18.5 25.9 19.6 23.2 19.0 18.5-20.0 25.3 21.7 20.0 18.7 20.5-25.0 25.2 37.3 26.4 34.4 25 4.1 7.0 6.0 9.1 16.0 Source: NNMB, 1996 & 2006(Rural) 1996 Females 2006

-5- Thinness as a public health problem Low prevalence (warning sign, monitoring required): 5-9% of population with BMI 18.5 Medium prevalence (poor situation): 10-19% of population with BMI 18.5 High prevalence (serious situation): 20-39% of population with BMI 18.5 Very high prevalence (critical situation): 40% of population with BMI 18.5

-6Mean Birth Weights in different parts of the world Region Mean Birth Weight (kg) North America, Western Europe and Australia 3.5-3.6 Eastern Europe 3.1-3.3 Africa and East Asia 2.9-3.1 South Asia 2.7

-7- Mean Birth Weights and LBW in SEAR Country N India 4307 Nepal Rural 2529 Urban 3629 Sri Lanka 1851 Myanmar 3582 Indonesia 1647 Thailand 4124 USA Afro-American 4614 Whites 16481 *Source: WHO, 1993. LBW ( 2500g) Birth weight (Kg) 33.0 2.63 14.3 22.3 18.4 17.8 10.5 9.6 2.78 2.76 2.84 2.85 2.94 3.00 10.6 6.0 3.14 3.36

-8- MATERNAL PARAMETERS (MEANS) ACCORDING TO BMI STATUS BMI CLASSES N 16.0 CED III 81 35.4 2510 53.1 16.0-16.9 CED II 133 38.1 2573 41.4 17.0-18.4 CED I 460 40.9 2653 35.9 18.5-19.9 (NORMAL) 553 44.1 2771 27.7 20.0-24.9 (NORMAL) 717 49.6 2812 26.4 25.0-29.9 (OBESE) 68 60.6 2972 14.7 30 (OBESE) 5 75.5 2972 20.0 45.2 2742 30.5 TOTAL 2017 MOTHER'S (Wt, Kg.) BIRTH (Wt, Kg.) LBW ( 2500 g)% Source : NNMB Repeat Surveys (1991) , Quoted by Nadamuni Naidu et al, 1994.

- 9Birth Weight and Socio-Economic Status Poor income Middle income High income Height (cms) 151.5 154.2 156.3 Weight (kg) 45.7 49.9 56.2 Hb(g/dl) 10.9 11.1 12.2 Birth weight (kg) 2.70 2.90 3.13

-10BIRTH WEIGHTS IN POOR AND WELL TO DO GROUPS IN MADRAS AND COONOR N B.WT Lbs Kg 1949 SPEL.WARD GEN.WARD 1269 1179 7.12 6.3 3.2 2.8 1954 SPEL.WARD GEN.WARD 200 500 6.85 6.01 3.08 2.7 SOURCE : Varkki C, et al, 1955. PREMATURE (%) 12.3 8.4

-11Birth weights (kg) in poor after supplementation 1971 1972 No Supplementation No Supplementation Food 2.704 3.028 Source : L.Iyengar, 1972. Supplementation Folic acid 2.920 Supplementation Iron Iron Folic acid 2.570 2.650 2.899

-12 - Attempts made to increase birth weights in poor socio-economic group 1. Iron 2. Folic acid 3. Iron and Folic acid 4. Zinc 5. Vitamin A 6. N3 fats, fish oils 7. Micro nutrients 8. Reduction of activities

- 13 Distribution (%) of 1-5 years children according to nutritional status (Weight for age) by sex-Gomez classification Nutrition Grades* Boys (n 2011) Girls Pooled (n 1957) (n 3968) Normal 13.1 12.1 12.6 Mild 45.5 45.5 45.5 Moderate 37.4 37.8 37.6 Severe 4.0 4.6 4.3 * NCHS standards Source: NNMB 2005.

-14 aDistribution (%) of 1-5 years according to Weight for age – standard deviation (SD) classification by gender Weight for age* Median Boys (n 2011) Girls Pooled (n 1957) (n 3968) 3.5 3.6 3.6 -1SD to Median 11.4 10.1 10.8 -2SD to -1SD 31.4 31.1 31.2 -3SD to -2SD 38.2 37.7 37.9 Median - 3SD 15.5 17.5 16.5 * NCHS standards

- 14b Distribution (%) of 1-5 years according to Weight for age – standard deviation (SD) classification by Age groups Weight for age* 1 1-3 3-5 Median -1SD to Median -2SD to -1SD -3SD to-2SD Median -3SD 23.1 26.7 27.9 16.2 6.1 4.5 11.5 28.8 35.0 20.2 2.7 10.9 31.7 39.9 14.9 * NCHS standards Source: NNMB 2005.

- 15 a Distribution (%) of 1-5 years children according to Height for age standard deviation (SD) classification by gender Height for age* Median Boys (n 2011) Girls Pooled (n 1957) (n 3968) 8.0 6.6 7.3 -1SD to Median 15.5 13.4 14.5 -2SD to -1SD 26.4 25.5 26.0 -3SD to -2SD 26.6 27.9 27.2 Median - 3SD 23.5 26.6 25.0 * NCHS standards Source: NNMB 2005.

- 15 b Distribution (%) of 1-5 years according to Height for age – standard deviation (SD) classification by Age groups Height for age* 1 1-3 3-5 Median -1SD to Median -2SD to -1SD -3SD to-2SD Median -3SD 28.3 27.6 25.5 12.8 5.7 9.4 16.3 23.0 24.8 26.5 6.2 14.0 28.2 28.2 23.5 * NCHS standards Source: NNMB 2005.

-16 a Distribution (%) of 1-5 years children according Weight for Height standard deviation (SD) classification by gender Weight for Height * Median Boys (n 2457) Girls Pooled (n 2399) (n 4856) 10.8 13.2 12.0 -1SD to Median 31.5 31.1 31.3 -2SD to -1SD 41.8 41.6 41.7 -3SD to -2SD 13.3 11.8 12.6 Median - 3SD 2.5 2.3 2.4 * NCHS standards Source: NNMB 2005-06.

-16 b Distribution (%) of 1-5 years according to Weight for Height– standard deviation (SD) classification by Age groups Weight for Height * 1 1-3 3-5 Median -1SD to Median -2SD to -1SD -3SD to-2SD Median -3SD 23.5 39.4 24.1 8.6 4.4 11.7 30.2 43.6 11.8 2.6 12.2 32.4 39.9 13.3 2.2 * NCHS standards Source: NNMB 2005.

-17 - ICMR Balanced diet for adults (1 Cu) Cereals 460 Pulses 40 Veg Roots Flesh Milk foods 40 60 - 150 Fats 25 Sugar 30 Nuts Fruits Condiments - - -

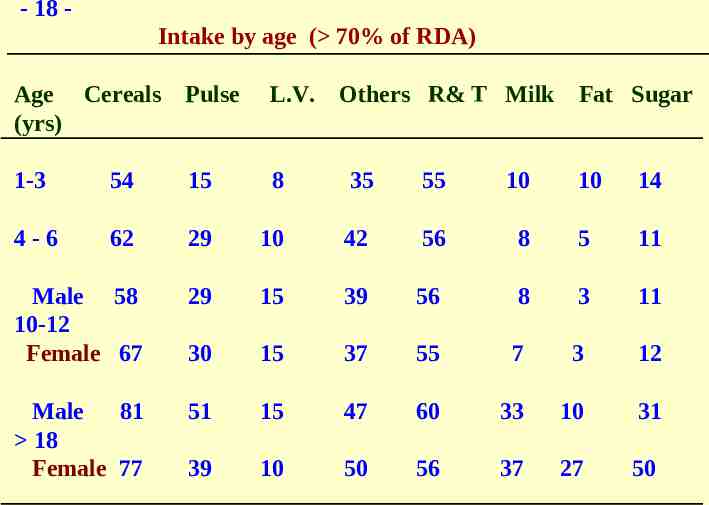
- 18 Intake by age ( 70% of RDA) Age Cereals (yrs) Pulse L.V. Others R& T Milk Fat Sugar 1-3 54 15 8 35 55 10 10 14 4-6 62 29 10 42 56 8 5 11 Male 58 10-12 Female 67 29 15 39 56 8 3 11 30 15 37 55 7 3 12 Male 81 18 Female 77 51 15 47 60 33 10 31 39 10 50 56 37 27 50

- 19 - Nutrient intakes ( 70% of RDA) by Age Age (yrs) Energy 1-3 4 -6 7- 9 Male 10-12 Female Male 13-15 Female Male 16-17 Female Male Protein Fat Calcium Iron Vitamin A 30 31 38 45 62 73 61 50 23 30 36 54 19 28 37 24 15 15 13 9 8 10 7.5 9 57 41 51 22 11 9 55 40 65 32 10 11 70 39 58 25 15 9 70 40 60 32 12 9 70 43 62 35 14 10 80 77 85 70 29 11 89 78 77 61 15 11 18 Female
- 20 – Other nutritional problems Apart from stunting and under weight – 1. Anaemia - 60-90% 2. Iodine Deficiency - endemic most parts of the country 3. Goitre - endemic in North East, sub Himalayan range, many tribal belts in central India 4. Fluorosis - endemic many parts of the country

-21 – According to Recommended Dietary Guidelines 60-65% Calories from Carbohydrates 25-30% from Fat 10-12% from Protein Each of these calories, proteins and fats must be derived from as many foods as possible In the rural area of India 80% of Calories are derived from from Cereals Those with adequate calories from cereals have high iron intakes, but because almost All the calories come from cereals, the iron is not available this population must derive its calories from other sources such as pulse, meat, vegetable, milk egg to use this iron.

- 22 Children Only 30% have calorie adequacy (from cereals). They are deficient in all the other nutrient rich foods recommended for children. The WHO Recommendation Calories - 30-40% must come from fats (low volumes and energy densities) Vitamin A, calcium, iron - from milk, eggs, flesh foods, vegetables, fruit etc. (will also contribute additional calories), Cereals, pulse to be used to bridge the calorie gap. In India – it is reversed, cereal load has resulted in simple minded diagnosis of micronutrient deficiencies.

- 23 - How did we reach this Cereal – Calorie Trap ? RDA, Consumption units Minimum Wages Poverty Line Green Revolution---PDS story The consumption unit

- 24RDA ICMR Balanced diet for adults (1 Cu) Cereals Pulses Veg 460 40 40 Roots Flesh Milk foods 60 - 150 Fats 25 Sugar Nuts Fruits Condiments 30 - - -

- 25 Coefficient for computing calorie requirement of different groups* Group Cu-Units Adult male (sedentary worker) 1.0 Adult male (moderate worker) 1.2 Adult male (heavy worker) 1.6 Adult female (sedentary worker) 0.8 Adult female (moderate worker) 0.9 Adult female (heavy worker) 1.2 Adolescents 12 – 21 years 1.0 Children 9 to 12 years 0.8 Children 7 to 9 years 0.7 Children 5 to 7 years 0.6 Children 3 to 5 years 0.5 Children 1 to 3 years 0.4 *Source: Gopalan et al (1991)

- 26 Minimum Wages - Criteria 1. 3 consumption units * for one wage earner 2. 2700 cals per average Indian adult 3. ? Clothing - 72 yards per annum per family 4. ? House rent 5. ? Fuel, Lighting etc - 20% of wages 6. ? Education, Medical and other expenses

- 27 - Since Minimum wages are based on calories Cheapest source of 2000 calories (Gm) Cost (Rs.) Sugar 520 8.00 Rice 571.4 11.0 Oil 225 ml 18.0 Dals 500.0 22.0 Potato 2000 20.0 Sapota, banana 1740 25 Milk 3250ml 60 Chicken 2000 120 Dry fruits 400 200

- 28 - Micironutrients essential for man Vitamins Trace minerals A. Micronutrients known to be essential for man and animals Vitamin A Thiamin Iron Selenium Vitamin D Riboflavin Iodine Manganese Vitamin K Nicotinic acid Zinc Chromium Copper Cobalt Vitamin E Pyridoxine Essential fatty acid Folic acid ( -6 and -3) Biotin (?) Vitamin B12 Pantothenic acid (?) Ascorbic acid B. Micronutrients essential for animals and not yet established as essential for man Choline p-Aminobenzoic acid Source: Narasinga Rao BS. Silicon Molybdenum Fluorine Arsenic Nickel

- 29 - Phytonutrients for Health Promotion Phytonutrient class Carotenoids Glucosinolates, Isothiocyanates, Indoles Inositol phosphates Phenolics, cyclic compounds Phytoestrogens Phytosterols Polyphenols Protease inhibitor Saponins Sulfides and thiols Source: Beecher

- 30 - Dietary antioxidants Nutrients Non-nutrients -Carotene-provitamin A Carotenoids (lycopene,xanthophyls) Ascorbic acid-vitamin C (cryptoxanthine, Lutein, -and -carotenes zeaxanthine) Tocopherols Flavonoids (quercetin, myricetin, quercetagatin, gossypetin) Tocotrienols Riboflavin Sulfur amino acids Anthocyanins Cysteine and methionine Isoflavones Selenium Phenolic compounds (catechin) Indoles

- 31 - Phytonutrients act synergistically with micronutrients – as part of an orchestra. Example - -carotene, vitamin C, vitamin E and selenium act as Antioxidants with flavonoids, carotenoids and phenolic compounds. An orchestra cannot be converted to a solo. -carotene supplementation to prevent lung cancer did not lower rates of lung cancer – it increased it among high risk groups. Single agents can be counter productive.

- 32 - Distribution (%) of children by protein –calorie adequacy status Age (yrs) % with adequate % with adequate calories Vitamins Minerals 1-3 31.8 8.0 15.0 4-6 28.2 10.0 20.0 7-9 28.1 7.5 20.0 10-12 26.0 (B) 9.0 15.0 32.9 (G) Source: NNMB Reports, 2002

-33 – Mean intake of one Nutrient iron (mg) by levels of percentage RDA of energy Details % RDA of energy Mean SD Iron (n) 70 9.6 7.50 (9.2 – 10.0) (1081) 70 – 100 13.2 8.07 12.9 - 13.5) (2567) 100 17.0 9.64 16.3 – 17.1) (2034) 13.8 8.94 (5682) Women Pooled

-34 – Mean intake of one nutrient iron (mg) by levels of percentage RDA of energy Details % RDA of energy Mean SD (n) 70 5.9 4.57 (5.7 – 6.1) (2898) 70 – 100 9.7 6.46 (9.3 – 10.2) (856) Children 1-6 yrs 100 Pooled Iron 14.0 9.19 (234) (12.9 – 15.2) 7.2 5.87 (3988)

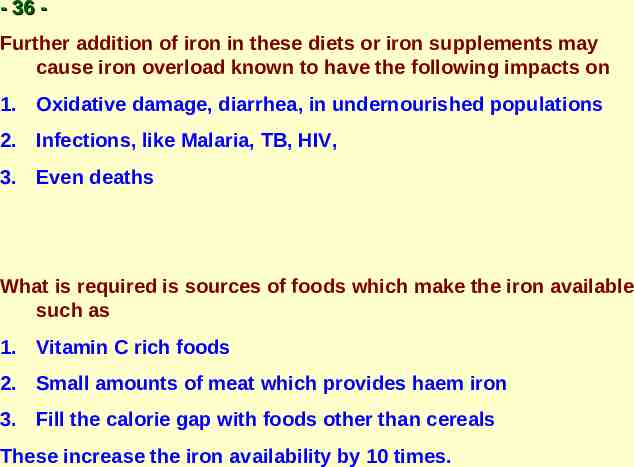
- 35 Supplying additional iron would reduce anemia only if iron is very deficient and only up to the point where another factor becomes rate limiting. In the case of poor societies, other factors- both nutritional and environmental- are as important. Therefore, management of nutritional anemia requires Health and food (providing many nutrients, not just iron). Instead of putting all nutrients into one food (cereal) Cereal should be eaten with nutrient rich foods.

- 36 Further addition of iron in these diets or iron supplements may cause iron overload known to have the following impacts on 1. Oxidative damage, diarrhea, in undernourished populations 2. Infections, like Malaria, TB, HIV, 3. Even deaths What is required is sources of foods which make the iron available such as 1. Vitamin C rich foods 2. Small amounts of meat which provides haem iron 3. Fill the calorie gap with foods other than cereals These increase the iron availability by 10 times.

-37 Wheat flour fortification To increase intakes of iron – using whole wheat flour (cereal) - iron availability is only – 1-2% Other option - chemical addition to whole wheat flour NaEDTA – to increase iron availability by 2-3 times However, it increases viscosity of the flour ? Toxicity – and binding with other metal ions Costly – four times Ferrous sulfate - without EDTA low bioavailability alters taste – with EDTA – iron amount have to be decreased net iron intake the same Elemental iron – Low bioavailability Fortification of flour in the West is carried out using MAIDA (refined flour)
- 38 Options – whole country to switch to Refined flour (MAIDA) or Tolerate Toxicity of EDTA Safe levels to be calculated in undernourished populations Intake should not be more than 2.5 mg / kg body weight At this level of EDTA it does not provide adequate iron for children No studies on the use of fortified flour in children

- 39 St.John’s study (Kurpad) Role of school lunch programme on anemia status of school children Government school children – given the usual vitamin A and anti-helmenthic Had the regular school lunch programme (cooked rice, dal, some vegetables) No iron tablets were distributed Anemia reduced from 60% to 20% Important role of providing food on Anemia

- 40 Millions of tons of cereals will be processed so that a few mg quantities of a nutrient is added– and only 1-5% is available to humans Need to re-look at strategy Studies done in the following countries did not show improvements in haemoglobin after the distribution of iron fortified wheat flour. Srilanka Bangladesh Thailand Morocco Ivory coast India

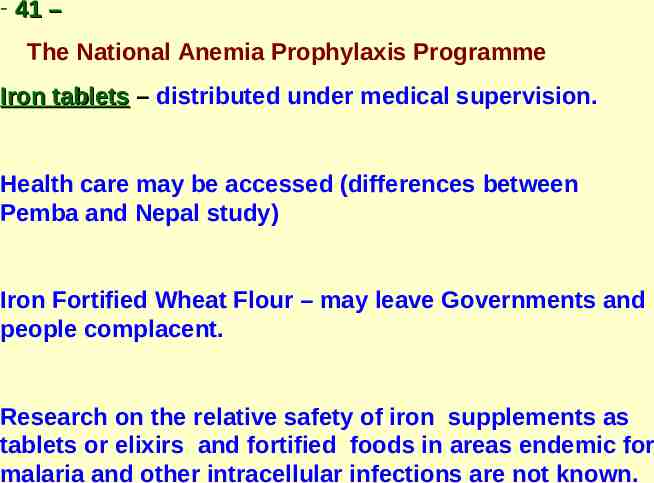
- 41 – The National Anemia Prophylaxis Programme Iron tablets – distributed under medical supervision. Health care may be accessed (differences between Pemba and Nepal study) Iron Fortified Wheat Flour – may leave Governments and people complacent. Research on the relative safety of iron supplements as tablets or elixirs and fortified foods in areas endemic for malaria and other intracellular infections are not known.

- 42 15th ILC - Dr.Aykroyd’s Recommended Diet (1957) gr. Cereals- 14 oz - 420 Pulses 03oz - 90 Vegetables 10 oz - 300 Milk 10 oz - 300 Sugar/ 02oz - 60 Oil / ghee 02oz - 60 Fruits 02 oz - 60 Fish / meat 03 oz - 90 Eggs 01 oz - 30
- 43 - Average Intake of Nutrients (per day) (Boys and Girls) Age (yrs) 1–3 4-6 Mean RDA Mean RDA Protein (g) 20.2 22.0 28.7 30.0 Total fat (g) 10.7 25.0 12.7 25.0 Energy (Kcal) 719 1240 1020 1690 Calcium (mg) 245 400 272 400 Iron (mg) 5.7 12 8.6 18 Vit.A (µg) 129 400 166 400 Thiamin (mg) 0.5 0.6 0.7 0.9 Riboflavin (mg) 0.3 0.7 0.4 1.0 Niacin (mg) 5.2 8.0 7.9 11.0 Vit.C (mg) 17 30 25 40 Free folic acid (µg) 20.3 30 28.8 40

- 44 Nutrition Rehabilitation Centre (National Institute of Nutrition) Average intake in hospital of a 7 kg child Bread Rice Milk Oil Dal sugar Banana Eggs 40 gms 50 gms 500 ml 20 ml 25 gms 10 gms 1 1 1100 cal, 35 gms protein Approximate cost of a 1000 Kcal diet – Rs 15 /-

- 45 Rehabilitation diet for undernourished children Diet - as close to the home diet as possible Routine Diet at Nutrition ward for children 6 AM 8.30 am 11 AM 1.30pm 4pm 7pm 10pm Milk Khichri Bread and Milk / egg Lunch Rice, Dal,etc Milk / Egg Dinner Rice Dal etc Milk Extra milk given during night if required

- 46 The need to provide regular food, familiar as close to home food as possible vs high density packaged food. 1. Problems of processed food which is not produced locally. 2. Half the children of this country will require this 3. Assured supply for years is hard to imagine 4. Local populations will learn to trust only packaged food 5. Women will forget how to feed their children 6. Local employments of millions of women will be affected

- 47 Iron content (mg) of common foods in 100g of edible portion Cereal Iron (mg) Bajra 8.0 Jowar 4.1 Ragi 3.9 Rice, raw, hand pounded 3.2 Rice, bran 35.0 Rice, flakes 20.0 Rice, puffed 6.6 Wheat, bulgar (parboiled) 4.9 Wheat, whole 5.3 Wheat flour (whole) 4.9 Wheat flour (refined) 2.7 Wheat germ 6.0 Wheat bread (brown) 2.2

- 48 Contd/- Pulses Iron (mg) Bengal gram dhal 5.3 Bengal gram roasted 9.5 Cow pea 8.6 Horse gram whole 6.77 Lentil 7.58 Moth beans 9.5 Rajmah 5.1 Soya bean 10.4 Leafy Vegetables Amaranth polygonoides 27.3 Cauliflower greens 40.0 Manathakkali leaves 20.5 Mint 15.6 Mustard leaves 16.3 Parsley 17.9 Radish leaves table 18.0

- 49 Contd/- Other vegetables Iron (mg) Karonda dry 39.1 Lotus stem dry 60.6 Plantain green 6.27 Sundakai dry 22.2 Nuts and oilseeds Almond 5.09 Cashewnut 5.81 Walnut 2.64 Condiments and spices Asafoetida 39.4 Mango powder 45.2 Omum 12.5 Pepper dry (black) 12.4 Poppy seeds 15.9 Tamarind pulp 17.0 Turmeric 67.8

- 50 Contd/- Fruits Iron (mg) Ambada 3.9 Apricot dry 4.6 Raisins 7.7 Seethaphal 4.31 Fishes and other sea foods Bombay duck dried 19.1 Chingri goda, dried 49.6 Crab muscle 21.2 Meat and poultry Beef meat 18.8 Liver sheep 6.3 Mutton muscle 2.5 Pork muscle 2.2