Specialized Nutrition Support: Enteral & Parenteral Nutrition Chapter
29 Slides767.50 KB
Specialized Nutrition Support: Enteral & Parenteral Nutrition Chapter 16 Nutrition & Diet Therapy (7th Edition)
Need for Nutrition Support Nutrition support may be required to meet patient’s nutritional needs – Patients often too ill to obtain energy & nutrients by consuming foods – Or illness may interfere with eating, digestion or absorption Nutrition & Diet Therapy (7th Edition) Nutrition support: delivery of formulated nutrients by feeding tube or intravenous infusion Enteral nutrition: supplying nutrients using GI tract, including tube feedings & oral diets Parenteral nutrition: intravenous provision of nutrients, bypassing the GI tract
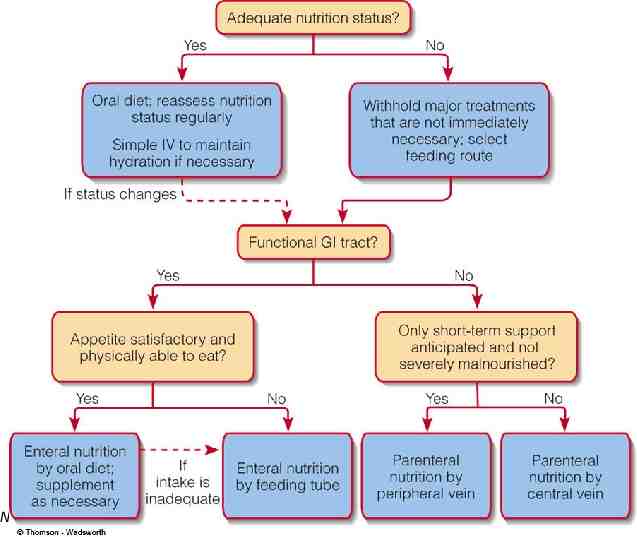
Selecting a Feeding Route Nutrition & Diet Therapy (7th Edition)
Enteral Nutrition Support Wide selection of enteral formulas, designed to meet variety of medical & nutritional needs May be used alone or in conjunction with other foods Many formulas can provide all of nutrient requirements if consumed in sufficient volume Classified according to macronutrient composition Preferred over intravenous feedings Enteral nutrition requires intact & normal GI function Nutrition & Diet Therapy (7th Edition)
Types of Enteral Formulas Standard formula: for patients who can digest & absorb nutrients without difficulty; contains protein & carbohydrate sources Hydrolyzed formulas: used for patients with compromised digestive or absorptive functions— macronutrients are partially or fully broken down & require little, if any, digestion before absorption Disease-specific formulas: designed to meet nutrient needs of patients with particular disorders: liver, kidney, lung diseases, glucose intolerance, metabolic stress Modular formulas: contain only one or two macronutrients; used to enhance other formulas Nutrition & Diet Therapy (7th Edition)
Enteral Nutrition in Medical Care Oral use – Supplement diet when food consumption does not meet need – Reliable source of nutrients & energy – Taste important consideration Tube feedings – Used when patient cannot consume enough food or formula orally – Feeding delivered directly to stomach or intestine Nutrition & Diet Therapy (7th Edition) Patients can drink enteral formulas when they are unable to consume enough food from a conventional diet
Enteral Nutrition in Medical Care (con’t) Candidates for tube feedings: – Severe swallowing difficulties – Little or no appetite for extended periods, especially if malnourished – GI obstructions, impaired motility of the upper GI tract – After intestinal resection, beginning enteral feedings – Mentally incapacitated due to confusion, dementia, neurological disorders – Individuals in coma – Individuals with extremely high nutrient requirements – Individuals on mechanical ventilators Nutrition & Diet Therapy (7th Edition)
Enteral Nutrition in Medical Care (con’t) Feeding routes – Selected on basis of medical condition, expected duration, potential complications of a particular route – Main routes: Transnasal (temporary) – Nasogastric – Nasoduodenal – Nasojejunal Gastrostomy Jejunostomy Nutrition & Diet Therapy (7th Edition)
Enteral Nutrition in Medical Care (con’t) Formula selected after assessment of the diagnosis, patient’s age, medical problems, nutritional status, ability to digest & absorb nutrients Nutrition-related factors influencing formula selection – Energy, protein & fluid requirements – Need for fiber modifications – Individual tolerances (food allergies & sensitivities) Nutrition & Diet Therapy (7th Edition)
Enteral Nutrition in Medical Care (con’t) Administration of tube feedings – Safe handling Open feeding system Closed feeding system Safety guidelines – Review of procedure with patient & family – Verification of tube placement (Xray) – Formula delivery Intermittent feedings (bulk over 20-40 min) Continuous feedings (pump) Bolus feeding (one or several “shots”) Nutrition & Diet Therapy (7th Edition) Open feeding system: requires formula to be transferred from original packaging to feeding container Closed feeding system: formula prepackaged in ready-to-use containers Intermittent feeding: delivery of prescribed volume over 2040 minutes Continuous feeding: slow delivery at constant rate over 8-24 hour period Bolus feeding: delivery of prescribed volume in less than 15 minutes
Enteral Nutrition in Medical Care (con’t) Formula volume & strength – Procedures vary by institution – Almost all patients can receive undiluted isotonic or hypertonic formulas – Generally started slowly and volume gradually increased Rate & amount of increase depend on patient’s tolerance Continuous feedings may be better tolerated than intermittent feedings Checking gastric residual volume (vol. of formula in stomach after fdg.) – Volume of formula remaining in stomach from previous feeding – Evaluate if gastric residual 200 mL – If tendency to retain persists, physician may consider intestinal feedings or drug therapy to stimulate gastric emptying Nutrition & Diet Therapy (7th Edition)
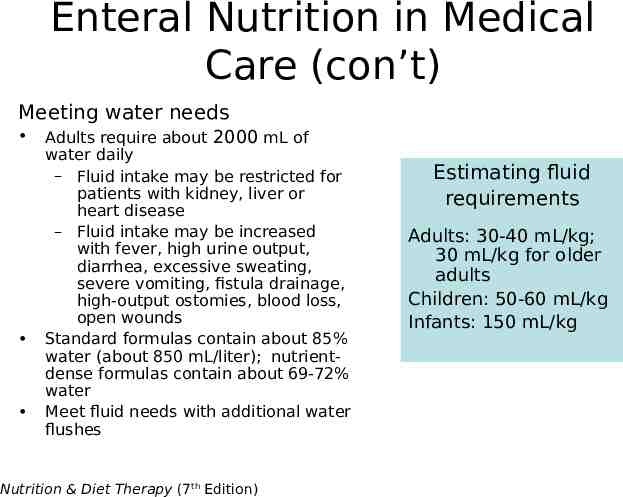
Enteral Nutrition in Medical Care (con’t) Meeting water needs Adults require about 2000 mL of water daily – Fluid intake may be restricted for patients with kidney, liver or heart disease – Fluid intake may be increased with fever, high urine output, diarrhea, excessive sweating, severe vomiting, fistula drainage, high-output ostomies, blood loss, open wounds Standard formulas contain about 85% water (about 850 mL/liter); nutrientdense formulas contain about 69-72% water Meet fluid needs with additional water flushes Nutrition & Diet Therapy (7th Edition) Estimating fluid requirements Adults: 30-40 mL/kg; 30 mL/kg for older adults Children: 50-60 mL/kg Infants: 150 mL/kg
Enteral Nutrition in Medical Care (con’t) Transition to table foods – Volume of formula is tapered off as condition improves – Gradual shift to oral diet Begin drinking same formula that is delivered by tube Oral intake should supply about 2/3 of nutrient needs before tube feedings discontinued Nutrition & Diet Therapy (7th Edition)
Enteral Nutrition in Medical Care (con’t) Giving Medication through feeding tubes – Potential for diet-drug interactions must be considered before administration – Continuous feeding halted for approximately 15 minutes before & 15 minutes following medication delivery (longer for some medications) – Type of medication may make tube administration impossible—require change to alternate route Generally best to administer medications by mouth whenever possible Nutrition & Diet Therapy (7th Edition)
Enteral Nutrition in Medical Care (con’t) Complications of tube feedings – Gastrointestinal problems: nausea, diarrhea – Mechanical problems related to tube feeding process – Metabolic problems: biochemical alterations & nutrient deficiencies Many complications preventable with appropriate feeding route, formula & delivery method Close attention to patient’s medical condition & medication use is important (follow up/reassessment) – Monitor weight, hydration status – Verify lab test results Nutrition & Diet Therapy (7th Edition)
Parenteral Nutrition Support Indicated for patients who do not have functioning GI tract & who are malnourished (or likely to become so) Used when enteral formulas cannot be used or intestinal function is inadequate Life-saving option for critically-ill persons Two main access sites: central or peripheral vein Nutrition & Diet Therapy (7th Edition) – – – – – – – – Indications Short-bowel syndrome Severe pancreatitis Malabsorption disorders Intestinal obstruction or fistula Severe burns or trauma Critical illnesses or wasting disorders Bone marrow transplant Malnourished with high risk for aspiration
Venous Access Peripheral parenteral nutrition (PPN) – Can only provide limited amounts of energy & protein – Peripheral veins can be damaged by overly concentrated solutions – Limited to patients who do not have high nutrient needs or fluid restrictions – Used most often for short-term nutrition support (7-10 days) – Rotation of vein sites may be necessary Nutrition & Diet Therapy (7th Edition)
Venous Access (con’t) Total parenteral nutrition (TPN) – Can reliably meet complete nutrient requirements – Provides nutrient-dense solutions for patients with high nutrient needs or fluid restrictions – Preferred for long-term intravenous feedings – Inserted directly into a large central vein Nutrition & Diet Therapy (7th Edition)
Parenteral Solutions Customized formulations to meet patients’ nutrient needs Highly individualized; often recalculated on daily basis until patient’s condition stabilizes Contents: – – – – – Amino acids (both essential and non-essential for protein) Carbohydrates (dextrose) Lipid emulsions Fluid & electrolytes Vitamins & trace minerals Nutrition & Diet Therapy (7th Edition)
Administering Parenteral Nutrition Multidisciplinary nutrition support team of health care professionals – – – – Physicians Nurses Dietitians Pharmacist Potential complications related to venous line & metabolic problems Nutrition & Diet Therapy (7th Edition)
Administering Parenteral Nutrition (con’t) Administration procedures – Insertion & care of intravenous catheters – Administration of parenteral solutions Continuous administration -24 hours/day Cyclic administration – 10 to 16 hour periods – Monitoring patient condition, nutritional status, complications – Discontinuing of feedings-when GI function returns Nutrition & Diet Therapy (7th Edition)
Nutrition Support at Home Continuation of nutritional support (tube feedings or parenteral nutrition) after medical condition has stabilized Candidates for home nutrition support – Long-term nutrition care required for chronic conditions – Users intellectually capable of learning procedures, monitoring treatment & managing complications Planning for home nutrition – Involvement of users in decision making to ensure longterm compliance & satisfaction – Assessment & evaluation of type of feeding, equipment, resources, ability to perform procedures Nutrition & Diet Therapy (7th Edition)
Nutrition Support at Home (con’t) Quality of life issues – Lifestyle adjustments may cause struggle for patients & families – Economic impact – Time & other demands associated with treatment – Physical difficulties, including disrupted sleep – Social issues – Life-sustaining therapy associated with serious complications Nutrition & Diet Therapy (7th Edition) Portable pumps & convenient carrying cases allow people who require home nutrition support to move about freely
Nutrition in Practice—Inborn Errors of Metabolism Inborn error of metabolism: inherited trait, caused by genetic mutation Results in absence, deficiency or malfunction of a protein that has a critical metabolic role Nutrition & Diet Therapy (7th Edition)
Nutrition in Practice—Inborn Errors of Metabolism (con’t) Medical nutrition therapy is primary treatment for many inborn errors that involve nutrient metabolism Dietary intervention generally involves restriction of substances that cannot be metabolized or supplying substances that cannot be produced Dietary changes may improve outcomes – Preventing accumulation of toxic metabolites – Replacing deficient nutrients – Providing a diet that supports normal growth & development & maintains health Some inborn errors may require treatment other than or in addition to dietary changes Nutrition & Diet Therapy (7th Edition)
Nutrition in Practice—Inborn Errors of Metabolism (con’t) Phenylketonuria (PKU) – Metabolic disorder affecting amino acid metabolism – Missing or defective protein is liver enzyme that converts the essential amino acid phenylalanine to tyrosine – Phenylalanine & metabolites accumulate and damage developing nervous system—most debilitating effect is on brain development – Diagnosed within first few days following birth—infants routinely screened in all 50 states – Treatment consists of lifelong diet restricting phenylalanine & supplying tyrosine; allowing blood levels of these amino acids to be maintained within safe ranges Nutrition & Diet Therapy (7th Edition)
Nutrition in Practice—Inborn Errors of Metabolism (con’t) Managing PKU – Central to PKU diet is enteral formula that is phenylalanine-free & supplies energy, amino acids, vitamins & minerals – Formula requirements must be recalculated periodically to accommodate growing infant’s shifting needs for protein, phenylalanine, tyrosine & energy Careful monitoring of foods containing phenylalanine Monitoring of growth rates & nutrition status – Parents & children may need to develop creative ways to make diet enjoyable Nutrition & Diet Therapy (7th Edition)
Nutrition in Practice—Inborn Errors of Metabolism (con’t) Galactosemia – Inborn error of carbohydrate metabolism – Deficiency of enzyme needed to metabolize galactose – Accumulation of galactose can result in damage to multiple tissues Reaction with severe vomiting & jaundice within days of initial feeding of infant Serious liver damage may result, progressing to symptomatic cirrhosis Other complications: kidney failure, cataracts, brain damage – Delay in treatment can result in irreversible brain damage Nutrition & Diet Therapy (7th Edition)
Nutrition in Practice—Inborn Errors of Metabolism (con’t) Managing galactosemia – Main focus of diet is exclusion of milk & milk products (elimination of galactose) – Avoidance or restriction of other galactosecontaining foods Organ meats Some legumes, fruits & vegetables – Food lists help patients to identify galactose content of common foods – Complications may develop despite compliance with diet therapy Nutrition & Diet Therapy (7th Edition)