Chapter 24: The Forearm, Wrist, Hand and Finger
76 Slides724.50 KB
Chapter 24: The Forearm, Wrist, Hand and Finger
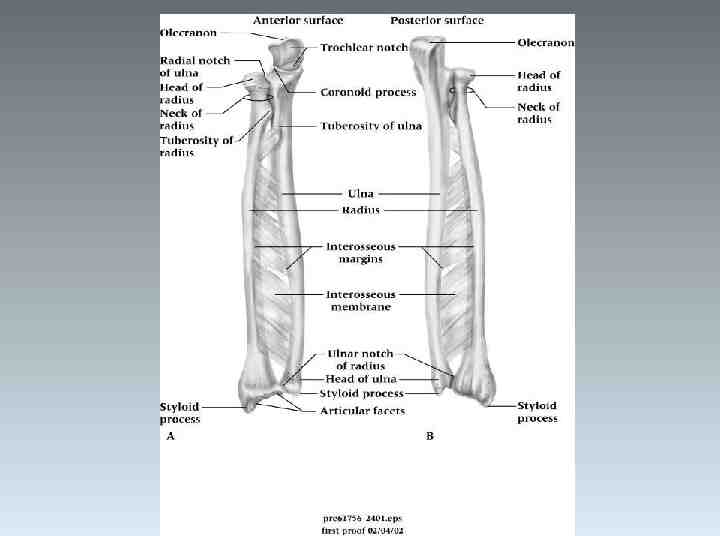
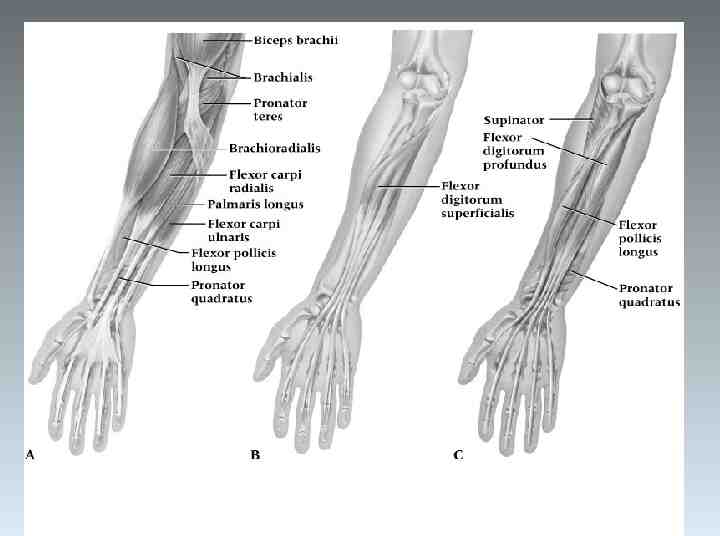
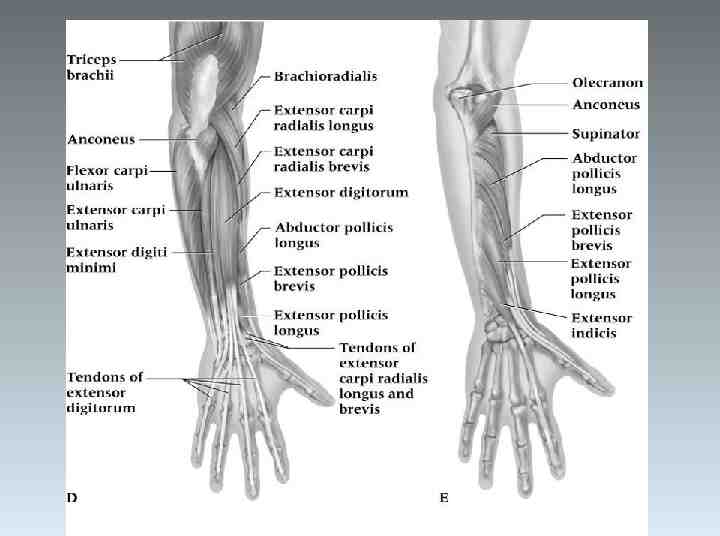
Anatomy of the Forearm
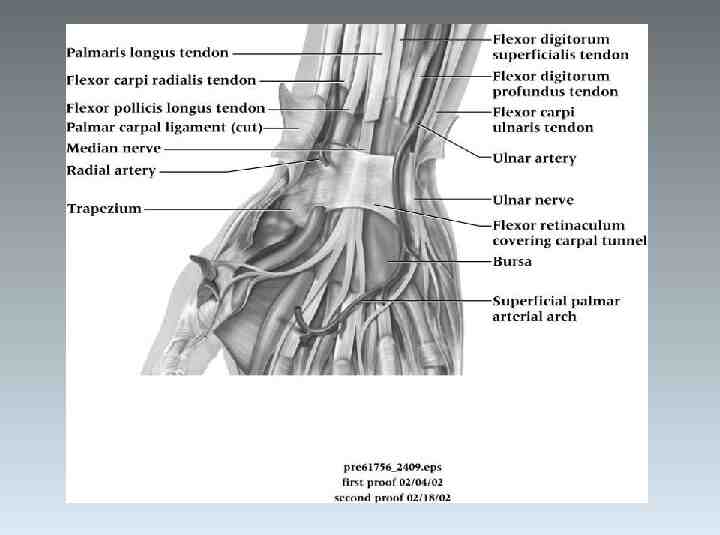
Blood and Nerve Supply Most of the flexors are supplied by the median nerve Most of the extensor are controlled by the radial nerve Blood is supplied by the radial and ulnar arteries
Assessment of the Forearm History – What was the cause? – What were the symptoms at the time of injury, did they occur later, were they localized or diffuse? – Was there swelling and discoloration? – What treatment was given and how does it feel now?
Observation – Visually inspect for deformities, swelling and skin defects – Range of motion – Pain w/ motion Palpation – Palpated at distant sites and at point of injury – Can reveal tenderness, edema, fracture, deformity, changes in skin temperature, a false joint, bone fragments or lack of bone continuity
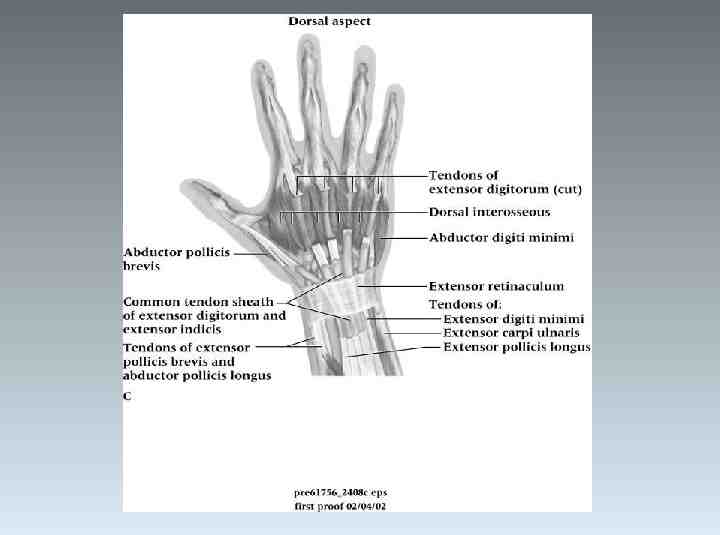
Palpation: Bony and Soft Tissue Proximal head of radius Olecranon process Radial shaft Ulnar shaft Distal radius and ulna Radial styloid Ulnar head Ulnar styloid Distal radioulnar joint Radiocarpal joint Extensor retinaculum Flexor retinaculum Extensor carpi radialis longus and brevis Extensor carpi ulnaris Brachioradialis Extensor pollicis longus and brevis
Palpation (continued) Abductor pollicis longus Extensor indicus supinator Flexor carpi radialis Palmaris longus Flexor digitorum superficialis Flexor digitorum profundus Flexor pollicis longus Pronator quadratus Pronator teres
Recognition and Management of Injuries to the Forearm Contusion – Etiology Ulnar side receives majority of blows due to arm blocks Can be acute or chronic Result of direct contact or blow – Signs and Symptoms Pain, swelling and hematoma If repeated blows occur, heavy fibrosis and possibly bony callus could form w/in hematoma
Contusion (continued) – Management Proper care in acute stage involves RICE for at least one hour and followed up w/ additional cryotherapy Protection is critical - full-length sponge rubber pad can be used to provide protective covering
Forearm Splints – Etiology Forearm strain - most come from severe static contraction Cause of splints - repeated static contractions Difficult to manage – Signs and Symptoms Dull ache between extensors which cross posterior aspect of forearm Weakness and pain w/ contraction Point tenderness in interosseus membrane – Management Treat symptomatically If occurs early in season, strengthen forearm; when it occurs late in season treat w/ cryotherapy, wraps, or heat Can develop compartment syndrome in forearm as well and should be treated like lower extremity
Forearm Fractures – Etiology Common in youth due to falls and direct blows Ulna and radius generally fracture individually Fracture in upper third may result in abduction deformity due pull of pronator teres Fracture in lower portion will remain relatively neutral Older athlete may experience greater soft tissue damage and greater chance of paralysis due to Volkman’s contracture – Signs and Symptoms Audible pop or crack followed by moderate to severe pain, swelling, and disability Edema, ecchymosis w/ possible crepitus
Management – Initially RICE followed by splinting until definitive care is available – Long term casting followed by rehab plan
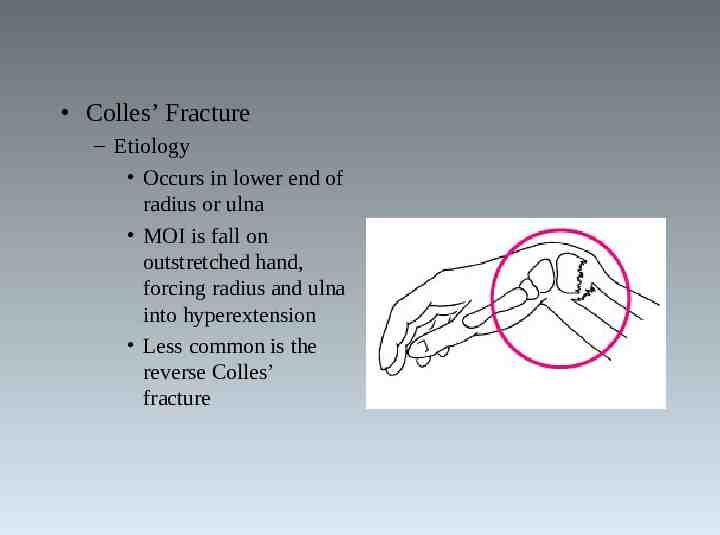
Colles’ Fracture – Etiology Occurs in lower end of radius or ulna MOI is fall on outstretched hand, forcing radius and ulna into hyperextension Less common is the reverse Colles’ fracture
– Signs and Symptoms Forward displacement of radius causing visible deformity (silver fork deformity) When no deformity is present, injury can be passed off as bad sprain Extensive bleeding and swelling Tendons may be torn/avulsed and there may be median nerve damage – Management Cold compress, splint wrist and refer to physician X-ray and immobilization Severe sprains should be treated as fractures Without complications a Colles’ fracture will keep an athlete out for 1-2 months In children, injury may cause lower epiphyseal separation

Madelung Deformity – Etiology Developmental deformity of the wrist Associated with changes in radius, ulna and carpal bone results in palmar and ulnar wrist subluxations Common in female athletes – particularly gymnasts Carpals become wedged between radius and ulna following epiphyseal plate changes – Signs and Symptoms Bowing of radius and ulna evident on X-ray Wrist pain and loss of forearm rotation Palmar subluxation with prominence of radius and ulnar styloid processes
Madelung Deformity (continued) – Management Therapeutic modalities and NSAID’s for pain Wrist can be taped or braced to prevent wrist extension Typically corrected surgically in athletes with chronic pain and disability
Anatomy of the Wrist, Hand and Fingers
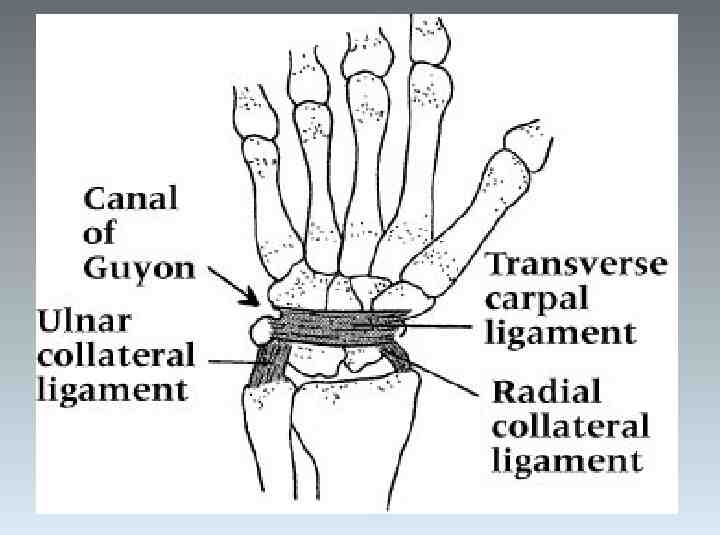
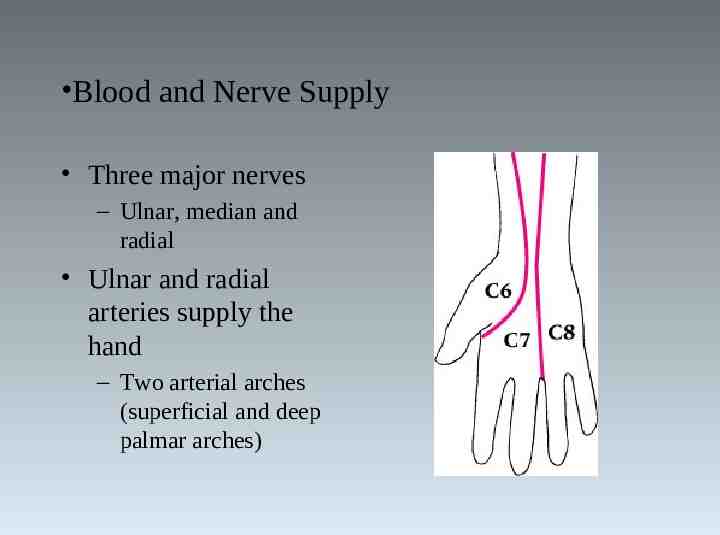
Blood and Nerve Supply Three major nerves – Ulnar, median and radial Ulnar and radial arteries supply the hand – Two arterial arches (superficial and deep palmar arches)
Assessment of the Wrist, Hand and Fingers History – – – – – – – – Past history Mechanism of injury When does it hurt? Type of, quality of, duration of, pain? Sounds or feelings? How long were you disabled? Swelling? Previous treatments?
Observation – – – – – Postural deviations Is the part held still, stiff or protected? Wrist or hand swollen or discolored? General attitude What movements can be performed fully and rhythmically? – Thumb to finger touching – Color of nailbeds
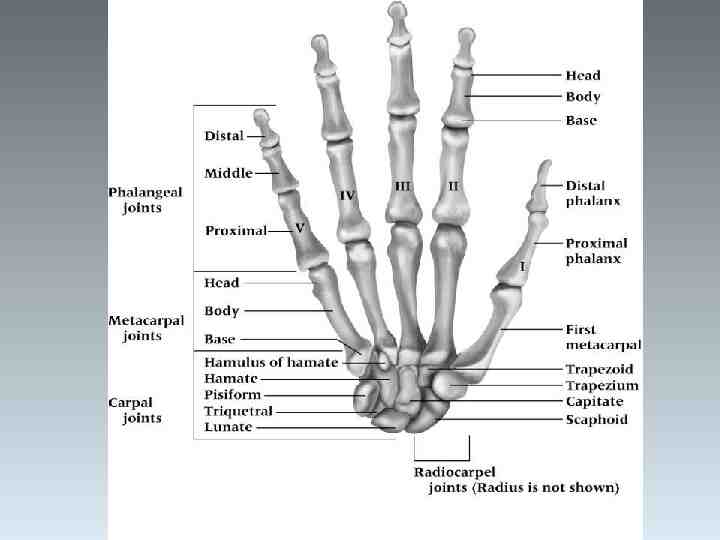
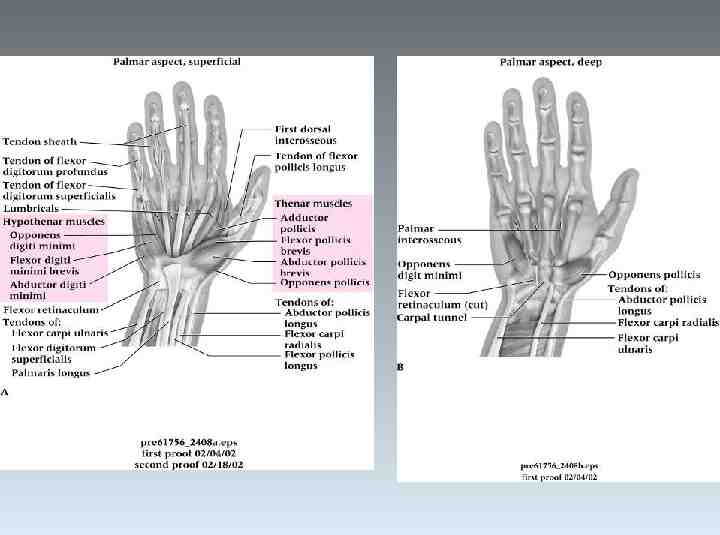
Palpation: Bony Scaphoid Trapezoid Trapezium Lunate Capitate Triquetral Pisiform Hamate (hook) Metacarpals 1-5 Proximal, middle and distal phalanges of the fingers Proximal and distal phalanges of the thumb
Palpation: Soft Tissue Triangular fibrocartilage Ligaments of the carpals Carpometacarpal joints and ligaments Metacarpophylangeal joints and ligaments Proximal and distal interphylangeal joints and ligaments Flexor carpi radialis Flexor carpi ulnaris Lumbricale muscles Flexor digitorum superficialis and profundus Palmer interossi Flexor pollicis longus and brevis Abductor pollicis brevis Opponens pollicis Opponens digiti minimi
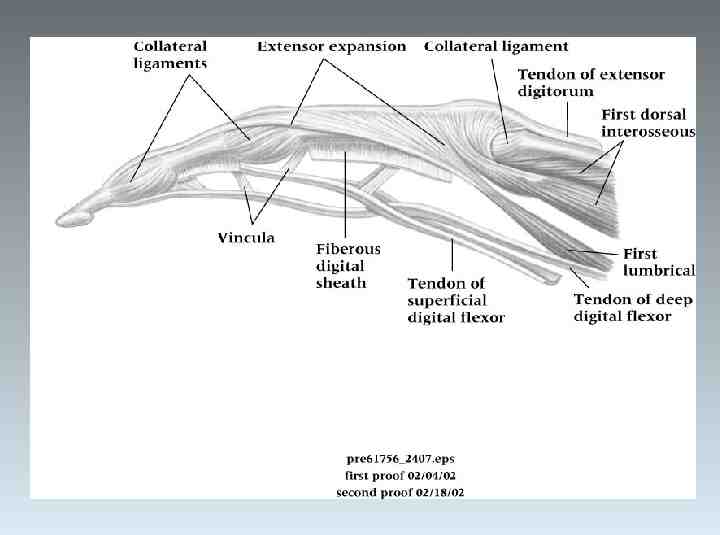
Palpation: Soft Tissue Extensor carpi radialis longus and brevis Extensor carpi ulnaris Extensor digitorum Extensor indicis Extensor digiti minimi Dorsal interossi Extensor pollicis brevis and longus Abductor pollicis longus
Special Tests – Finklestein’s Test Test for de Quervain’s syndrome Athlete makes a fist w/ thumb tucked inside Wrist is ulnarly deviated Positive sign is pain indicating stenosising tenosynovitis Pain over carpal tunnel could indicate carpal tunnel syndrome – Tinel’s Sign Produced by tapping over transverse carpal ligament Tingling, paresthesia over sensory distribution of the median nerve indicates presence of carpal tunnel syndrome
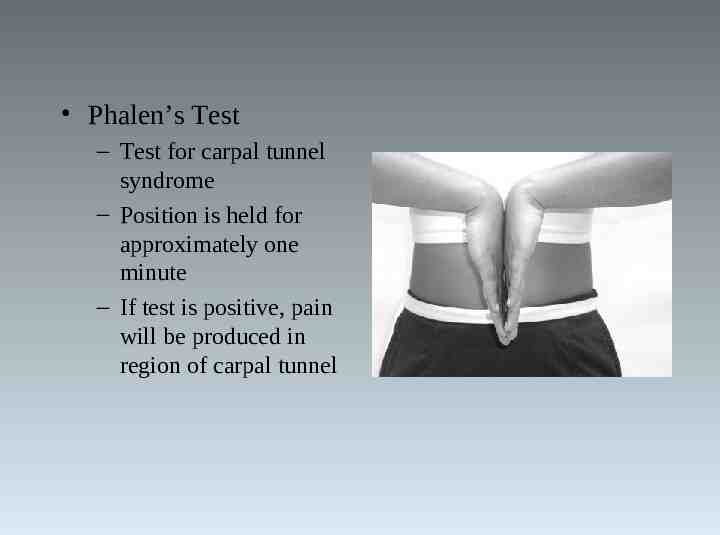
Phalen’s Test – Test for carpal tunnel syndrome – Position is held for approximately one minute – If test is positive, pain will be produced in region of carpal tunnel
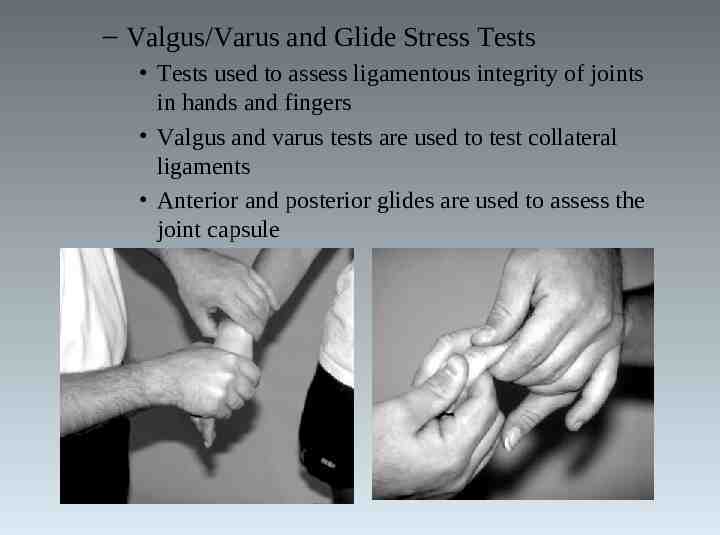
– Valgus/Varus and Glide Stress Tests Tests used to assess ligamentous integrity of joints in hands and fingers Valgus and varus tests are used to test collateral ligaments Anterior and posterior glides are used to assess the joint capsule
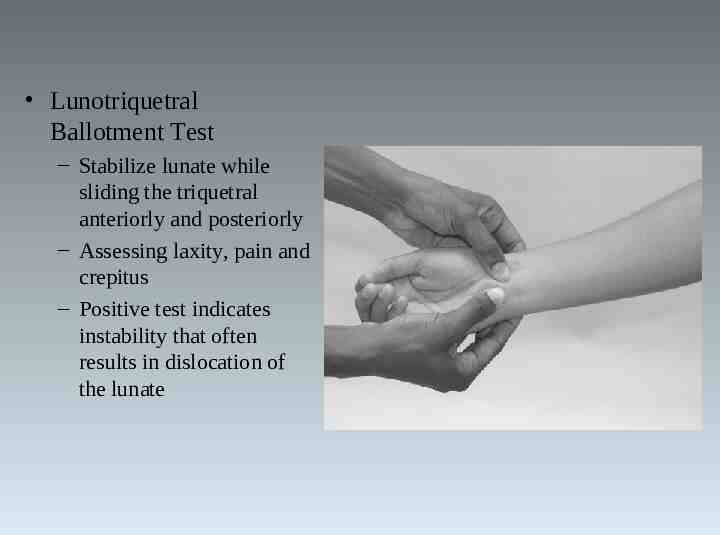
Lunotriquetral Ballotment Test – Stabilize lunate while sliding the triquetral anteriorly and posteriorly – Assessing laxity, pain and crepitus – Positive test indicates instability that often results in dislocation of the lunate
– Circulatory and Neurological Evaluation Hands should be felt for temperature – Cold hands indicate decreased circulation Pinching fingernails can also help detect circulatory problems (capillary refill) Allen’s test can also be used – – – – Athlete instructed to clench fist 3-4 times, holding it on the final time Pressure applied to ulnar and radial arteries Athlete then opens hand (palm should be blanched) One artery is released and should fill immediately (both should be checked) Hand’s neurological functioning should also be tested (sensation and motor functioning)
Functional Evaluation – Range of motion in all movements of wrist and fingers should be assessed – Active, resistive and passive motions should be assessed and compared bilaterally Wrist - flexion, extension, radial and ulnar deviation MCP joint - flexion and extension PIP and DIP joints - flexion and extension Fingers - abduction and adduction MCP, PIP and DIP of thumb - flexion and extension Thumb - abduction, adduction and opposition 5th finger - opposition
Recognition and Management of Injuries to the Wrist, Hand and Fingers Wrist Sprains – Etiology Most common wrist injury Arises from any abnormal, forced movement Falling on hyperextended wrist, violent flexion or torsion Multiple incidents may disrupt blood supply – Signs and Symptoms Pain, swelling and difficulty w/ movement

– Management Refer to physician for X-ray if severe RICE, splint and analgesics Have athlete begin strengthening soon after injury Tape for support can benefit healing and prevent further injury

Triangular Fibrocartilage Complex (TFCC) Injury – Etiology Occurs through forced hyperextension, falling on outstretched hand Violent twist or torque of the wrist Often associated w/ sprain of UCL – Signs and Symptoms Pain along ulnar side of wrist, difficulty w/ wrist extension, possible clicking Swelling is possible, not much initially Athlete may not report injury immediately
– Management Referred to physician for treatment Treatment will require immobilization initially for 4 weeks Immobilization should be followed by period of strengthening and ROM activities Surgical intervention may be required if conservative treatments fail
Tenosynovitis – Etiology Cause of repetitive wrist accelerations and decelerations Repetitive overuse of wrist tendons and sheaths – Signs and Symptoms Pain w/ use or pain in passive stretching Tenderness and swelling over tendon – Management Acute pain and inflammation treated w/ ice massage 4x daily for first 48-72 hours, NSAID’s and rest When swelling has subsided, ROM is promoted w/ contrast bath Ultrasound and phonphoresis can be used PRE can be instituted once swelling and pain subsided
Tendinitis – Etiology Repetitive pulling movements of (commonly) flexor carpi radialis and ulnaris; repetitive pressure on palms (cycling) can cause irritation of flexor digitorum Primary cause is overuse of the wrist – Signs and Symptoms Pain on active use or passive stretching Isometric resistance to involved tendon produces pain, weakness or both – Management Acute pain and inflammation treated w/ ice massage 4x daily for first 4872 hours, NSAID’s and rest When swelling has subsided, ROM is promoted w/ contrast bath PRE can be instituted once swelling and pain subsided (high rep, low resistance)
Nerve Compression, Entrapment, Palsy – Etiology Median and ulnar nerve compression Result of direct trauma to nerves – Signs and Symptoms Sharp or burning pain associated w/ skin sensitivity or paresthesia May result in benediction/ bishop’s deformity (damage to the ulnar nerve) or claw hand deformity (damage to both nerves) Palsy of radial nerve produces drop wrist deformity caused by paralysis of extensor muscles Palsy of median nerve can cause ape hand (thumb pulled back in line w/ other fingers) – Management Chronic entrapment may cause irreversible damage Surgical decompression may be necessary
Carpal Tunnel Syndrome – Etiology Compression of median nerve due to inflammation of tendons and sheaths of carpal tunnel Result of repeated wrist flexion or direct trauma to anterior aspect of wrist – Signs and Symptoms Sensory and motor deficits (tingling, numbness and paresthesia); weakness in thumb – Management Conservative treatment - rest, immobilization, NSAID’s If symptoms persist, corticosteroid injection may be necessary or surgical decompression of transverse carpal ligament
de Quervain’s Disease (Hoffman’s disease) – Etiology Stenosing tenosynovitis in thumb (extensor pollicis brevis and abductor pollicis longus Constant wrist movement can be a source of irritation – Signs and Symptoms Aching pain, which may radiate into hand or forearm Positive Finklestein’s test Point tenderness and weakness during thumb extension and abduction; painful catching and snapping

de Quervain’s Disease (Hoffman’s disease) – Management Immobilization, rest, cryotherapy and NSAID’s Ultrasound and ice are also beneficial Joint mobilizations have been recommended to maintain ROM
Dislocation of Lunate Bone – Etiology Forceful hyperextension or fall on outstretched hand – Signs and Symptoms Pain, swelling, and difficulty executing wrist and finger flexion Numbness/paralysis of flexor muscles due to pressure on median nerve – Management Treat as acute, and sent to physician for reduction If not recognized, bone deterioration could occur, requiring surgical removal Usual recovery is 1-2 months
Scaphoid Fracture – Etiology Caused by force on outstretched hand, compressing scaphoid between radius and second row of carpal bones Often fails to heal due to poor blood supply – Signs and Symptoms Swelling, severe pain in anatomical snuff box Presents like wrist sprain Pain w/ radial flexion – Management Must be splinted and referred for X-ray prior to casting Immobilization lasts 6 weeks and is followed by strengthening and protective tape Wrist requires protection against impact loading for 3 additional months
Hamate Fracture – Etiology Occurs as a result of a fall or more commonly from contact while athlete is holding an implement – Signs and Symptoms Wrist pain and weakness, along w/ point tenderness Pull of muscular attachment can cause non-union – Management Casting wrist and thumb is treatment of choice Hook of hamate can be protected w/ doughnut pad to take pressure off area
Wrist Ganglion – Etiology Synovial cyst (herniation of joint capsule or synovial sheath of tendon) Generally appears following wrist strain – Signs and Symptoms Appear on back of wrist generally Occasional pain w/ lump at site Pain increases w/ use May feel soft, rubbery or very hard – Management Old method was to first break down the swelling through distal pressure and then apply pressure pad to encourage healing New approach includes aspiration, chemical cauterization w/ subsequent pressure from pad Ultrasound can be used to reduce size Surgical removal is most effective treatment method
Contusion and Pressure Injuries of Hand and Fingers – Etiology Result of blow or compression of bones w/in hand and fingers – Signs and Symptoms Pain and swelling of soft tissue – Management Cold compression until hemorrhaging has ceased Follow w/ gradual warming - soreness may still be present -padding may also be necessary Bruising of distal phalanx can result in subungual hematoma extremely painful due to build-up of pressure under nail – Pressure must be released once hemorrhaging has ceased
Bowler’s Thumb – Etiology Perineural fibrosis of subcutaneous ulnar digital nerve of thumb Pressure from bowling ball on thumb – Signs and Symptoms Pain, tingling during pressure on irritated area and numbness – Management Padding, decrease amount of bowling If condition continues, surgery may be required
Trigger Finger or Thumb – Etiology Repeated motion of fingers may cause irritation, producing tenosynovitis Inflammation of tendon sheath (extensor tendons of wrist, fingers and thumb, abductor pollicis) Thickening occurs w/in the sheath, forming a nodule that does not slide easily – Signs and Symptoms Resistance to re-extension, produces snapping that is palpable, audible and painful Palpation produces pain and lump can be felt w/in tendon sheath – Management Same treatment as de Quervain’s disease -- if unsuccessful, injection and splinting are last options
Mallet Finger (baseball or basketball finger) – Etiology Caused by a blow that contacts tip of finger avulsing extensor tendon from insertion – Signs and Symptoms Pain at DIP; X-ray shows avulsed bone on dorsal proximal distal phalanx Unable to extend distal end of finger (carrying at 30 degree angle) Point tenderness at sight of injury – Management RICE and splinting for 6-8 weeks
Boutonniere Deformity – Etiology Rupture of extensor tendon dorsal to the middle phalanx Forces DIP joint into extension and PIP into flexion – Signs and Symptoms Severe pain, obvious deformity and inability to extend DIP joint Swelling, point tenderness – Management Cold application, followed by splinting Splinting must be continued for 5-8 weeks Athlete is encouraged to flex distal phalanx
Jersey Finger – Etiology Rupture of flexor digitorum profundus tendon from insertion on distal phalanx Often occurs w/ ring finger when athlete tries to grab a jersey – Signs and Symptoms DIP can not be flexed, finger remains extended Pain and point tenderness over distal phalanx – Management Must be surgically repaired Rehab requires 12 weeks and there is often poor gliding of tendon, w/ possibility of re-rupture
Dupuytren’s Contracture – Etiology Nodules develop in palmer aponeurosis, limiting finger extension - ultimately causing flexion deformity – Signs and Symptoms Often develops in 4th or 5th finger (flexion deformity) – Management Tissue nodules must be removed as they can ultimately interfere w/ normal hand function
Sprains, Dislocations and Fractures of Phalanges – Etiology Phalanges are prone to sprains caused by direct blows or twisting MOI is also similar to that which causes fractures and dislocations – Signs and Symptoms Recognition primarily occurs through history Sprain symptoms - pain, severe swelling and hematoma Gamekeeper’s Thumb – Etiology Sprain of UCL of MCP joint of the thumb Mechanism is forceful abduction of proximal phalanx occasionally combined w/ hyperextension
– Signs and Symptoms Pain over UCL in addition to weak and painful pinch – Management Immediate follow-up must occur If instability exists, athlete should be referred to orthopedist If stable, X-ray should be performed to rule out fracture Thumb splint should be applied for protection for 3 weeks or until pain free Splint should extend from wrist to end of thumb in neutral position Thumb spica should be used following splinting for support
Sprains of Interphalangeal Joints of Fingers – Etiology Can include collateral ligament, volar plate, extensor slip tears Occurs w/ axial loading or valgus/varus stresses – Signs and Symptoms Pain, swelling, point tenderness, instability Valgus and varus tests may be positive – Management RICE, X-ray examination and possible splinting Splint at 30-40 degrees of flexion for 10 days If sprain is to the DIP, splinting for a few days in full extension may assist healing process Taping can be used for support
Swan Neck Deformity and PsuedoBoutonniere Deformity – Etiology Distal tear of volar plate may cause Swan Neck deformity; proximal tear may cause PsuedoBoutonniere deformity – Signs and Symptoms Pain, swelling w/ varying degrees of hyperextension Tenderness over volar plate of PIP Indication of volar plate tear passive hyperextension – Management RICE and analgesics Splint in 20-30 degrees of flexion for 3 weeks; followed by buddy taping and then PRE
PIP Dorsal Dislocation – Etiology Hyperextension that disrupts volar plate at middle phalanx – Signs and Symptoms Pain and swelling over PIP Obvious deformity, disability and possible avulsion – Management Treated w/ RICE, splinting and analgesics followed by reduction After reduction, finger is splinted at 20-30 degrees of flexion for 3 weeks -- followed by buddy taping
PIP Palmar Dislocation – Etiology Caused by twist while digit is semiflexed – Signs and Symptoms Pain and swelling over PIP; point tenderness over dorsal side Finger displays angular or rotational deformity – Management Treat w/ RICE, splinting and analgesics followed by reduction Splint in full extension for 4-5 weeks after which it is protected for 6-8 weeks during activity
MCP Dislocation – Etiology Caused by twisting or shearing force – Signs and Symptoms Pain, swelling and stiffness at MCP joint Proximal phalanx is angulated at 60-90 degrees – Management RICE, splinting following reduction Buddy taping and given early ROM following splinting
Metacarpal Fracture – Etiology Direct axial force or compressive force Fractures of the 5th metacarpal are associated w/ boxing or martial arts (boxer’s fracture) – Signs and Symptoms Pain and swelling; possible angular or rotational deformity – Management RICE, analgesics are given followed by X-ray examinations Deformity is reduced, followed by splinting 4 weeks of splinting after which ROM is carried out
Bennett’s Fracture – Etiology Occurs at carpometacarpal joint of the thumb as a result of an axial and abduction force to the thumb – Signs and Symptoms CMC may appeared to be deformed - X-ray will indicate fracture Athlete will complain of pain and swelling over the base of the thumb – Management Structurally unstable and must be referred to an orthopedic surgeon
Distal Phalangeal Fracture – Etiology Crushing force – Signs and Symptoms Complaint of pain and swelling of distal phalanx Subungual hematoma is often seen in this condition – Management RICE and analgesics are given Protective splint is applied as a means for pain relief Subungual hematoma is drained
Middle Phalangeal Fracture – Etiology Occurs from direct trauma or twist – Signs and Symptoms Pain and swelling w/ tenderness over middle phalanx Possible deformity; X-ray will show bone displacement – Management RICE and analgesics No deformity - buddy tape w/ thermoplastic splint for activity Deformity - immobilization for 3-4 weeks and a protective splint for an additional 9-10 weeks during activity
Proximal Phalangeal Fracture – Etiology May be spiral or angular – Signs and Symptoms Complaint of pain, swelling, deformity Inspection reveals varying degrees of deformity – Management RICE and analgesics are given as needed Fracture stability is maintained by immobilization of the wrist in slight extension, MCP in 70 degrees of flexion and buddy taping
PIP Fractures and Dislocation – Etiology Combination of fracture and dislocation is the result of an axial load on a partially flexed finger – Signs and Symptoms Condition causes pain and swelling in the region of the PIP joint Localized tenderness over the PIP – Management RICE, analgesics, followed by reduction of the fracture If there is a small fragment, buddy taping is used Large fragments - splint at 30-60 degrees of flexion
Fingernail Deformities – Changes in normal appearance of the fingernail can be indicative of a number of different diseases Scaling or ridging psoriasis Ridging and poor development hyperthyroidism Clubbing and cyanosis congenital heart disorders or chronic respiratory disease Spooning or depression chronic alcoholism or vitamin deficiency
Rehabilitation of Injuries to the Forearm, Wrist, Hand and Fingers General Body Conditioning – Must maintain pre-injury level of conditioning – Cardiorespiratory, strength, flexibility and neuromuscular control – Many exercise options (particularly lower extremity) Joint Mobilizations – Wrist and hand respond to traction and mobilization techniques
Flexibility – Full pain free ROM is a major goal of rehabilitation – The program should include active assisted and active pain free stretching Strength – Exercises should not aggravate condition or disrupt healing process – A variety of exercises are available for strength (wrist and hand)
Neuromuscular Control – Hand and fingers require restoration of dexterity Pinching, fine motor activities (buttoning buttons, tying shoes, and picking up small objects) – Customized bracing, splints and taping techniques are available to protect the injured wrist and hand Return to Activity – Grip strength must be equal bilaterally, full range of motion and dexterity – Thumb has unique strength requirements – Manual resistance can be instituted to strengthen major motions; intrinsic muscles can be strengthened w/ rubber band