Burn Mass Casualty and Burn Surge Disaster Preparedness Course THE
72 Slides3.40 MB
Burn Mass Casualty and Burn Surge Disaster Preparedness Course THE SCIENCE OF SURGE CAPACITY SEPTEMBER 2021
Disclosures In relation to this presentation, I declare that there are no conflicts of interest and, no off-label use of medications will be discussed The content of this work focuses on general surge topics is based in part on the research of Hick & Hanfling et al. Terrorism, burn and blast trauma injury information is based on the research of Peleg et al. The burn surge content is based on the research of Kearns et al. Academic sources are included at the end of the presentation. Cases selected for demonstration are based on either personal experiences or extensive research of the event Medical care discussed in this content represents information commonly found in current academic sources at the time it was developed. All medical care and medical practice should be reviewed by a physician for currency and accuracy A conflict of interest is any situation in which a speaker or immediate family members have interests, and those may cause a conflict with the current presentation. Conflicts of interest do not preclude the delivery of the talk, but should be explicitly declared. These may include financial interests (eg. owning stocks of a related company, having received honoraria, consultancy fees), research interests (research support by grants or otherwise), organisational interests and gifts.
What is a surge capacity? Surge capacity is basically an absorption strategy to manage and treat patients from a disaster in quantities and complexity that could potentially overwhelm a hospital.
What is a surge capacity? For a burn mass casualty incident (BMCI), surge capacity will include the space, staff and supplies needed to temporarily manage a surge of patients with burn injuries until they can be admitted or transferred to other hospitals
5 Things from this module 1. Surge capacity is basically an absorption plan 2. Don’t confuse capacity with capability, both are important 3. The time to talk about crisis standards of care are well before the crisis occurs 4. Regardless of your size and the number of resources, all hospitals and EMS agencies reach a point of needing help. Who do you call and when will you need them? 5. Surge resources for a BMCI may change if the disaster is complex and has patients with trauma injuries as well or there is infrastructure damage such as with an earthquake
What is a disaster? Does context matter? Demand for critical resources outstrips availability, exceeding capacity and capability thus putting patients or staff in danger DISAST ER
What is a disaster? Does context matter? Context means; small communities with limited resources may have a lower threshold (patient numbers) which exceed capacity and capability DISAST ER
What is a disaster? Does context matter? Large communities with far greater resources may have a higher threshold, but at some point, all organizations have limited resources when the patient numbers exceed capacity and capability DISAST ER
What is a disaster? Does context matter? Goal is to plan ahead to ensure: More effective use of available resources Mobilization of additional resources Identify resources not commonly available but useful in a disaster or surge event DISAST ER
Defining Surge Capacity (Hick et al., 2004) Few surplus resources to accommodate these casualties exist in our current health care system.
Defining Surge Capacity (Hick et al., 2004) Plans for "surge capacity" must thus be made to accommodate a large number of patients.
Defining Surge Capacity (Hick et al., 2004) Surge planning should allow activation of multiple levels of capacity from the health care facility level to the federal level.
Defining Surge Capacity (Hick et al., 2004) Plans should be scalable and flexible to cope with the many types and varied timelines of disasters.
Defining Surge Capacity cont. (Hick et al., 2004) Incident management systems and cooperative planning processes will facilitate maximal use of available resources.
Defining Surge Capacity cont. (Hick et al., 2004) However, resource limitations may require implementation of triage strategies.
Defining Surge Capacity cont. (Hick et al., 2004) Facility-based or "surge in place" solutions maximize health care facility capacity for patients during a disaster.
Defining Surge Capacity cont. (Hick et al., 2004) When these resources are exceeded, community-based solutions, including the establishment of off-site hospital facilities, may be implemented.
3 Ss of Surge Capacity (Hick et al., 2004) 1. Space 2. Staff 3. Supplies (Also noted as Supplies, Pharmaceuticals and Equipment [SPE]) More will be discussed later about this aspect of Surge Capacity
Types of Surge Events (Kearns et al., 2017) “No Notice” or “Time-Zero” There are two categories of surge events that any jurisdiction or facility may confront. They include the “no notice” (also referred to as “time-zero”) mass casualty incident (MCI) and the more gradual surge associated with scenarios such as a pandemic event. A “no notice MCI event includes examples such as a traffic collision involving a bus, train derailment or a residential building collapse.
Types of Surge Events (Kearns et al., 2017) “Time Lag Accumulation” Although more gradual in onset than the “no notice” event, surge capacity is also needed during disasters that extend (or lag) over time and include infectious disease outbreaks. The sudden and immediate demand for medical services by a group of patients is not a new phenomenon. Nevertheless, management of these events have evolved through modeling and real-world events driving process improvement.
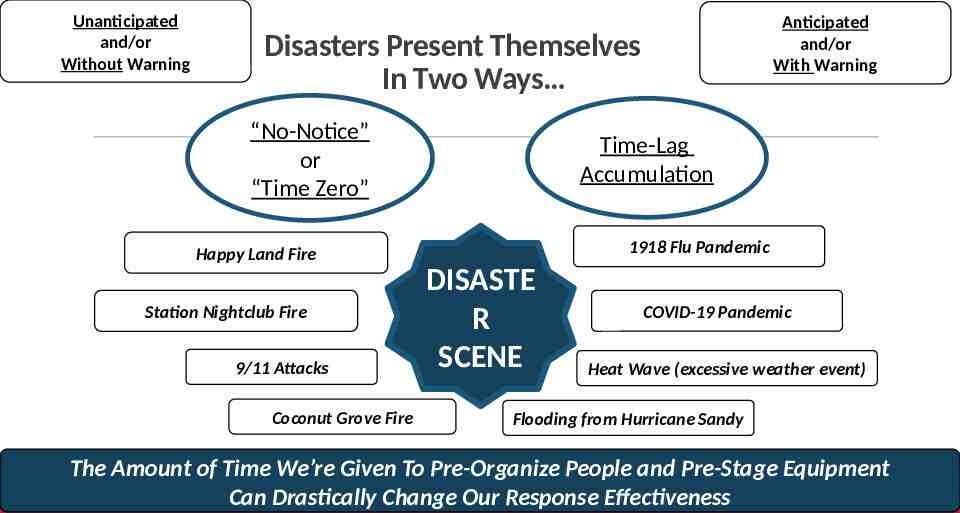
Unanticipated and/or Without Warning Anticipated and/or With Warning Disasters Present Themselves In Two Ways “No-Notice” or “Time Zero” Time-Lag Accumulation 1918 Flu Pandemic Happy Land Fire Station Nightclub Fire 9/11 Attacks Coconut Grove Fire DISASTE R SCENE COVID-19 Pandemic Heat Wave (excessive weather event) Flooding from Hurricane Sandy The Amount of Time We’re Given To Pre-Organize People and Pre-Stage Equipment Can Drastically Change Our Response Effectiveness
Capacity vs. Capability (Barbera & Macintyre, 2007) Surge Capacity – ‘the ability to manage increased patient care volume that otherwise would severely challenge or exceed the existing medical infrastructure’
Capacity vs. Capability (Barbera & Macintyre, 2007) Surge Capability – ‘the ability to manage patients requiring unusual or very specialized medical evaluation and intervention, often for uncommon medical conditions’
Principles of Surge Capacity (Hick et al., 2004) Standardization Incident Management System Multi-Agency Coordination System Public Information Systems Interoperability (eg: personnel and resource typing)
Principles of Surge Capacity (Hick et al., 2004) Scalability
Principles of Surge Capacity (Hick et al., 2004) Flexibility
Principles of Surge Capacity (Hick et al., 2004) Tiers of capacity (spillover to next level)
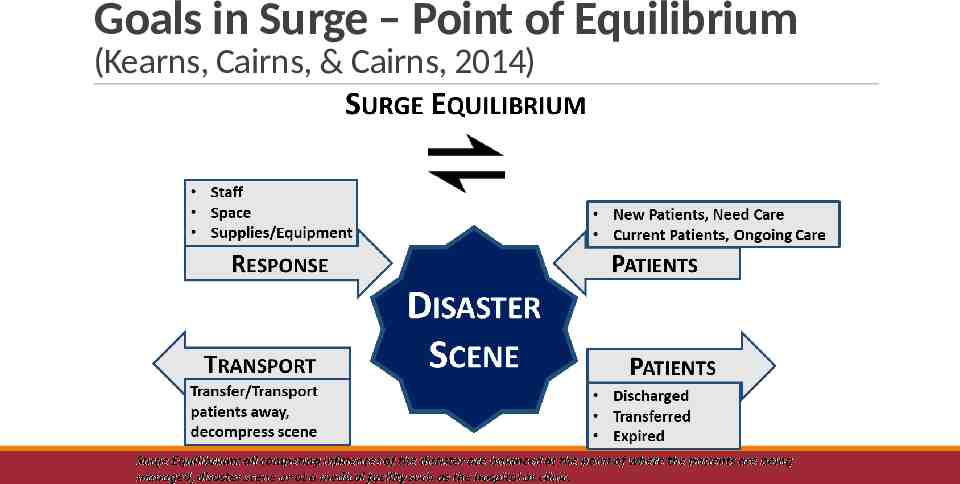
Goals in Surge – Point of Equilibrium (Kearns, Cairns, & Cairns, 2014)
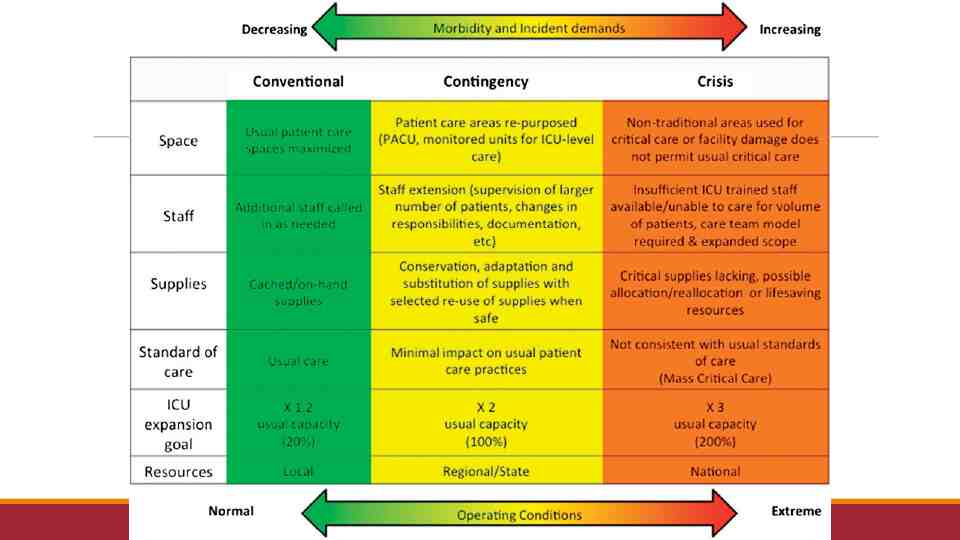
Standards of Care Conventional Care Contingency Care Crisis Care Hick JL, Einav S, Hanfling D, et al. Surge capacity principles: care of the critically ill and injured during pandemics and disasters: CHEST consensus statement. Chest. 2014;146(4 Suppl):e1S-e16S.
Surge Capacity and Burn Injuries (Kearns, Holmes, Alson, & Cairns, 2014) In the succeeding years, a consensus has coalesced around stratifying the surge capacity into three distinct tiers: conventional, contingency, and crisis surge capacities. For the purpose of this work, these three distinct tiers were adapted specifically to burn surge for disaster planning activities at hospitals where burn centers are not located. A review was conducted involving published plans, other related academic works, and findings from actual disasters as well as modeling. The aim was to create burn-specific definitions for surge capacity for hospitals where a burn center is not located.
Surge Capacity and Burn Injuries cont. (Kearns, Holmes, Alson, & Cairns, 2014) The three-tier consensus description of surge capacity is delineated in their respective stratifications by what will hereinafter be referred to as the three "S's"; staff, space, and supplies (also referred to as supplies, pharmaceuticals, and equipment). This effort also included the creation of a checklist for nonburn center hospitals to assist in their development of a burn surge plan.
Surge Capacity and Burn Injuries cont. (Kearns, Holmes, Alson, & Cairns, 2014) Patients with serious burn injuries should always be moved to and managed at burn centers, but during a medical disaster with significant numbers of burn injured patients, there may be impediments to meeting this goal. It may be necessary for burn injured patients to remain for hours in an outlying hospital until being moved to a burn center. This work was aimed at aiding local and regional hospitals in developing an extemporizing measure until their burn injured patients can be moved to and managed at a burn center(s).
Conventional Care Hick JL, Einav S, Hanfling D, et al. (2014) The spaces, staff, and supplies used are consistent with daily practices within the institution. These spaces and practices are used during a major mass casualty incident that triggers activation of the facility emergency operations plan. The targets for conventional care (at least 20% beyond usual capacity) are generally achieved using resources immediately available within the facility (vacant beds, discharge of patients to lower-intensity care units, cancellation of procedures) and should be achieved within a 2-h period. Depending on the role of the hospital in community response (eg, the only level I trauma center or pediatric facility in the area) and the hazards identified in the community (eg, risk for earthquake, terrorism), it may be prudent to plan for additional conventional capacity.
Conventional Care for a BMCI Kearns, Holmes, Alson et al. (2014) For a BMCI; relies on the spaces, staff and supplies within a given ED providing care during an MCI, triggers facility EOP, and may require staff to manage some burn injured patients up to 6 hrs with existing staff and existing SPE. Standard of Care is maintained. Kearns RD, Holmes JH 4th, Alson RL, Cairns BA. Disaster planning: the past, present, and future concepts and principles of managing a surge of burn injured patients for those involved in hospital facility planning and preparedness. J Burn Care Res. 2014;35(1):e33-42.
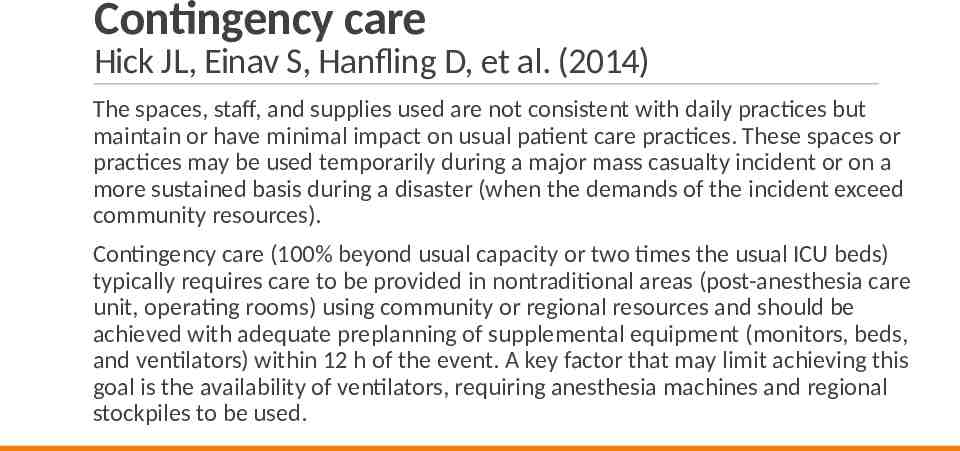
Contingency care Hick JL, Einav S, Hanfling D, et al. (2014) The spaces, staff, and supplies used are not consistent with daily practices but maintain or have minimal impact on usual patient care practices. These spaces or practices may be used temporarily during a major mass casualty incident or on a more sustained basis during a disaster (when the demands of the incident exceed community resources). Contingency care (100% beyond usual capacity or two times the usual ICU beds) typically requires care to be provided in nontraditional areas (post-anesthesia care unit, operating rooms) using community or regional resources and should be achieved with adequate preplanning of supplemental equipment (monitors, beds, and ventilators) within 12 h of the event. A key factor that may limit achieving this goal is the availability of ventilators, requiring anesthesia machines and regional stockpiles to be used.
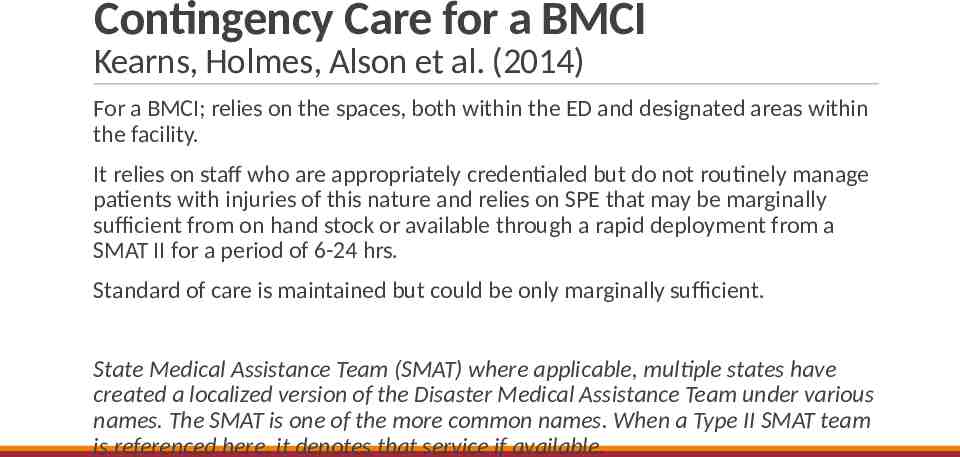
Contingency Care for a BMCI Kearns, Holmes, Alson et al. (2014) For a BMCI; relies on the spaces, both within the ED and designated areas within the facility. It relies on staff who are appropriately credentialed but do not routinely manage patients with injuries of this nature and relies on SPE that may be marginally sufficient from on hand stock or available through a rapid deployment from a SMAT II for a period of 6-24 hrs. Standard of care is maintained but could be only marginally sufficient. State Medical Assistance Team (SMAT) where applicable, multiple states have created a localized version of the Disaster Medical Assistance Team under various names. The SMAT is one of the more common names. When a Type II SMAT team is referenced here, it denotes that service if available.
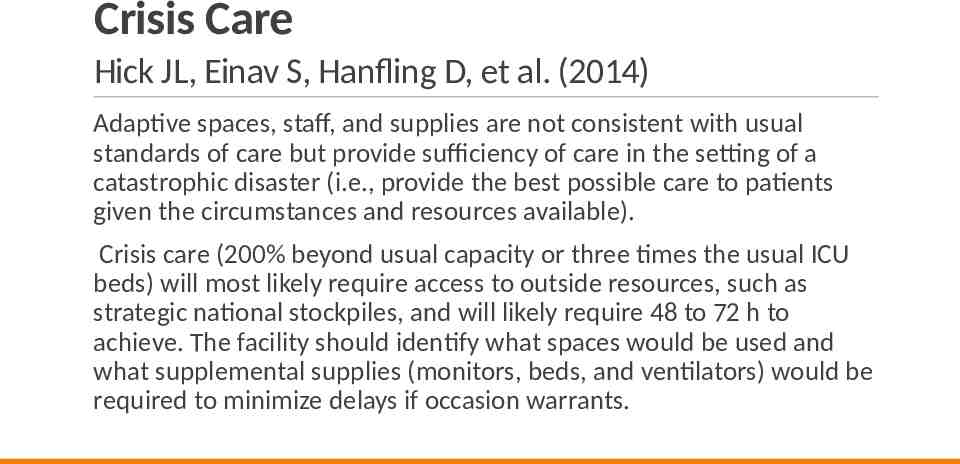
Crisis Care Hick JL, Einav S, Hanfling D, et al. (2014) Adaptive spaces, staff, and supplies are not consistent with usual standards of care but provide sufficiency of care in the setting of a catastrophic disaster (i.e., provide the best possible care to patients given the circumstances and resources available). Crisis care (200% beyond usual capacity or three times the usual ICU beds) will most likely require access to outside resources, such as strategic national stockpiles, and will likely require 48 to 72 h to achieve. The facility should identify what spaces would be used and what supplemental supplies (monitors, beds, and ventilators) would be required to minimize delays if occasion warrants.
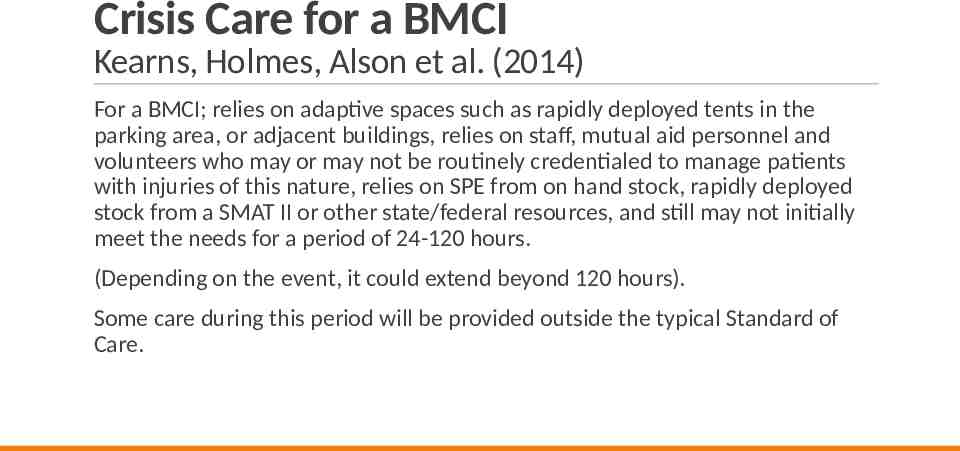
Crisis Care for a BMCI Kearns, Holmes, Alson et al. (2014) For a BMCI; relies on adaptive spaces such as rapidly deployed tents in the parking area, or adjacent buildings, relies on staff, mutual aid personnel and volunteers who may or may not be routinely credentialed to manage patients with injuries of this nature, relies on SPE from on hand stock, rapidly deployed stock from a SMAT II or other state/federal resources, and still may not initially meet the needs for a period of 24-120 hours. (Depending on the event, it could extend beyond 120 hours). Some care during this period will be provided outside the typical Standard of Care.
Crisis/Catastrophic Care Kearns, Bettencourt, Hickerson et al. (2020) Most mass casualty incidents can be resolved in a time period that is foreseeable. The consensus for the burn community is a target of 120 hours to return to either conventional or contingency standard of care. During the creation of the burn triage table revisions, the authors discussed events that offer less certainty for a conclusion and return to a conventional standard of care. For the rare scenario with potentially hundreds of thousands with burn injuries such as hostile military action leading to the detonation of a thermonuclear weapon, or where the American healthcare system is overwhelmed such as a pandemic event, the catastrophe could create an austere environment for an extended period. Thus, we identified this higher-order crisis type event as catastrophic care. Catastrophic care during this austere setting may include recycling and reusing materials, off label use of medications, adaptation of over-the-counter products, goods, and services, and other creative measures needed to meet the need for a potentially overwhelming number of patients for an undermined period.
3 Ss of Surge Capacity (Hick et al., 2004) 1. Space 2. Staff 3. Supplies (Also noted as Supplies, Pharmaceuticals and Equipment [SPE])
1. Space Have you preplanned surge inside your hospital or on the campus of your medical center, identified soft space with utilities, gasses, etc.?
1. Space Have you identified and preplanned an Alternate Care Facility? Institute of Medicine (2010). Medical Surge Capacity: Workshop Summary. Washington, DC, The National Academies Press.
1. Space Do you have access to a Mobile Hospital, and have you planned on how to use it to augment your services? Kearns, R. D., et al. (2014). "Deployable, portable, and temporary hospitals; one state's experiences through the years." Am J Disaster Med 9(3): 195-210.
1. Space cont. Anticipate need and duration, short term or long term? Surge is about absorption strategies Where can you put the patients? Are you attached to an office complex, medical school, other structure with space that can be adapted?
1. Space cont. Clear beds and use space (Immediate Bed Availably) Who can come back? Clinic Outpatient Cancel elective procedures Convert procedure/PACU areas to patient care Discharges and transfers (e.g.: nursing home) Discharge holding area
1. Space cont. Board patients in halls Accommodate vents on floor (or BVM or austere O2 flow powered ventilators) Alternative ambulatory care areas (lobbies, clinics, etc.)
1. Space cont. Most no-notice or time-zero surge events also have a short duration for surge needs. Most time-lag surge events tend to have an extended duration for surge needs. The first thoughts typically focus on immediate space needs, e.g., victims from the crash
1. Space cont. Don’t overlook private space needs for patient/family reunification, notification for the families of the missing or dead to include behavioral health and counseling services Also consider space for local, state and federal officials who may show up as well as public information, press conferences, staging of the press
1. Space cont. If a second (remote) location is needed, it should be preidentified and preplanned (these facility types are identified by various names such as; alternate care facility, federal medical shelters, surge hospital, etc.)
1. Space cont. Off site facility should include: Food/Water Restrooms Staff rehab areas Parking HVAC system specifications Are medical gases available or can they be easily deployed in the facility? (and suction) Communications phone/radio/internet (broadband) Power with alternate power or quick connect for alternate power City/County/State Owned Secure facility (preferred secured perimeter)
3 Ss of Surge Capacity (Hick et al., 2004) 1. Space 2. Staff 3. Supplies (Also noted as Supplies, Pharmaceuticals and Equipment [SPE])
2. Staff Different events different staff needs e.g.: Trauma, Medical, infectious disease, HazMat, etc. Scope of event scope of staff recalled Notification system or mechanism to recall staff Support staff – e.g.: housekeeping, dietary, central supply, behavioral/psychosocial/clergy, clerical, finance
2. Staff cont. Labor pool unit leader Just in Time (JIT) trainers Rely on specialists to be team leaders; ie burn nurse working with other (non-burn) nurses, can serve as force multipliers Assign staff to specific areas when possible Specialty Physician or Specialty Nursing staff typically most scarce
2. Staff cont. (force multipliers) Hospital personnel Clinic personnel Non-clinical practice professionals Retired or other volunteer professionals (eg: ESAR-VHP) Trainees in health professions
2. Staff cont. (force multipliers) Service organizations Lay public / faith-based / family members Government personnel Veterinarian and other veterinary staff (Essential to address these situations well before the disaster for rapid granting of privileges, scope and range of practice, Ethics Committee for Crisis Standards of Care, Legal advice, etc.)
3 Ss of Surge Capacity (Hick et al., 2004) 1. Space 2. Staff 3. Supplies (Also noted as Supplies, Pharmaceuticals and Equipment [SPE])
3. Supplies (on site) Patient care supplies – may vary by type of event Medical Gases – oxygen (other gases as needed) and suction
3. Supplies (on site) Pharmacy – blood products, analgesia, sedation, antidotes, (inventory of what’s available and what do you have access to) PPE – masks, gloves, gowns
3. Supplies (on site) Supply and staffing issues (72 to 96 hour) Supply chain management, logistics and planning sections Nonmedical supplies; cleaning, food/nutrition, etc.
3. Supplies (for a BMCI) Do you push supplies to the scene? Put in a basket stretcher or secure to a flat stretcher (basket stretcher works best) Total weight for basket and items should not exceed 198 lbs. (90kg) and can be added to the stretcher for an outbound/responding helicopter
3. Supplies (for a BMCI) Do you push supplies to the scene? (Easy items) Intravenous fluids (Ringers Lactate) Endotracheal Tubes, common adult and children's sizes Burn dressings or bandages can be problematic, maybe best to use simply large clean sheets but just remember, whatever goes on, will be the first to come off
3. Supplies (for a BMCI) Do you push supplies to the scene? (difficult to impossible) Pain medications
All Disasters are Local. Capabilities and Resources Tiered Response Strategy National Response State Response Regional / Mutual Response Systems Local Response Minimal Low Medium High Increasing Magnitude and Severity Catastrophic
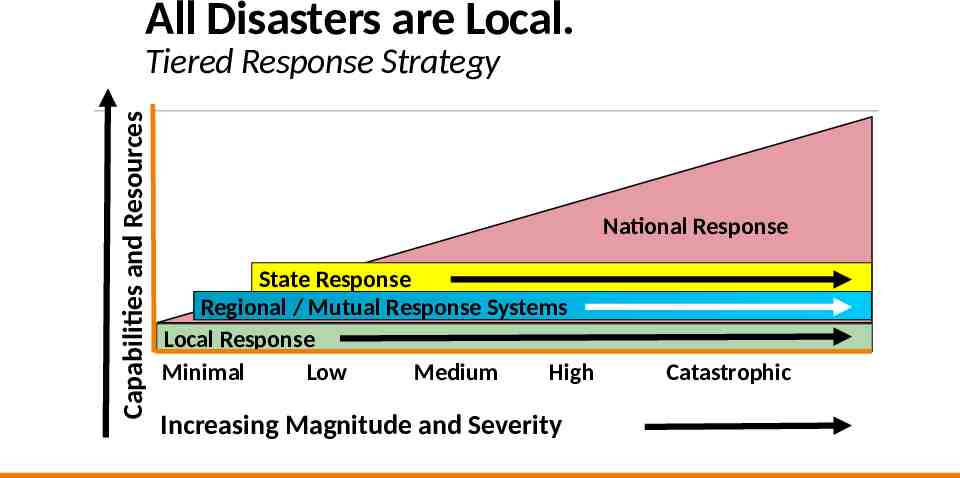
Conclusion All disasters are local, initially answered by local responders and managed by local hospitals. Don’t design solutions that overlooks those facts. Before the disaster, is your strategy to take your “disaster” to the hospital and re-triage there or do you have the resources to distribute the patients effectively from the scene? A BMCI has obvious limitations simply based on the traditional capacity and capability of burn centers both locally and regionally Surge planning includes staff, space and supplies. However, an often-overlooked component is the role of transportation. Transportation services can vary from ground to air, but all must consider the impact of distance, geography, topography, and meteorology.
5 Things from this module 1. Surge capacity is basically an absorption plan 2. Don’t confuse capacity with capability, both are important 3. The time to talk about crisis standards of care are well before the crisis occurs 4. Regardless of your size and the number of resources, all hospitals and EMS agencies reach a point of needing help. Who do you call and when will you need them? 5. Surge resources for a BMCI may change if the disaster is complex and has patients with trauma injuries as well or there is infrastructure damage such as with an earthquake
Thanks For questions; please contact: Randy Kearns, DHA, MSA, FACHE, FRSPH, CEM [email protected], [email protected], or randy [email protected]
References Barbera JA, Macintyre AG. Medical Surge Capacity and Capability: A Management System for Integrating Medical and Health Resources During Large-Scale Emergencies. In: Services USDoHaH, ed. Second ed. https://www.phe.gov/preparedness/planning/mscc/handbook/documents/mscc080626.pdf: The CNA Corporation, Institute for Public Research; 2007:274. Hick JL, Hanfling D, Burstein JL, et al. Health care facility and community strategies for patient care surge capacity. Annals of emergency medicine. 2004;44(3):253-261. Hick JL, Barbera JA, Kelen GD. Refining surge capacity: conventional, contingency, and crisis capacity. Disaster medicine and public health preparedness. 2009;3(2 Suppl):S59-67. Kearns RD, Cairns BA, Cairns CB. Surge Capacity and Capability. A Review of the History and Where the Science is Today Regarding Surge Capacity during a Mass Casualty Disaster. Front Public Health. 2014;2:29.
References Kearns RD, Holmes JHt, Alson RL, Cairns BA. Disaster planning: the past, present, and future concepts and principles of managing a surge of burn injured patients for those involved in hospital facility planning and preparedness. J Burn Care Res. 2014;35(1):e33-42. Kearns RD, Skarote MB, Peterson J, et al. Deployable, portable, and temporary hospitals; one state's experiences through the years. Am J Disaster Med. 2014;9(3):195-210. Kearns RD, Marcozzi DE, Barry N, Rubinson L, Hultman CS, Rich PB. Disaster Preparedness and Response for the Burn Mass Casualty Incident in the Twenty-first Century. Clinics in plastic surgery. 2017;44(3):441-449. Kearns RD, Bettencourt AP, Hickerson WL, et al. Actionable, Revised (v.3), and Amplified American Burn Association Triage Tables for Mass Casualties: A Civilian Defense Guideline Journal of Burn Care & Research. 2020;41(4):770-779. Institute of Medicine. Medical Surge Capacity: Workshop Summary. Washington, DC: The National Academies Press; 2010.
Content for this Presentation was Created or Developed by Randy Kearns for All Clear Emergency Management Group to be used for the State of Vermont Dr. Kearns began his career as a paramedic, rescue chief and firefighter and instructor. Over 30 years, he taught emergency services programs at several community colleges in the Carolinas, spent 8 years in hospital administration and led multiple emergency service and emergency management organizations. Dr. Kearns has been a responder to 25 presidentially declared disasters as a local, state and federal representative. In 2014, Dr. Kearns retired (from the State of North Carolina) as a Clinical Assistant Professor at the University of North Carolina, School of Medicine. After spending four years as the Healthcare Management Program Chair and an Associate Professor at the University of Mount Olive, Dr. Kearns joined the faculty here at the University of New Orleans in the College of Business Administration, August 2018. Publication Indexes: PubMed Scopus ResearchGate ORCID Dr. Kearns has 81 publications in various forms. And, according to Expertscape ( www.expertscape.com an academic artificial intelligence analysis software) is ranked 4rd internationally for research in “Surge Capacity” 5th internationally for research in “Mass Casualty Incidents” and 11th for his work in “Disaster Planning.” All Clear Emergency Management Group, LLC is an experienced consulting firm that provides an array of emergency management services and conference management services. Our team of dedicated professionals will exceed our clients’ expectations.
Assignment of Rights This content was developed for the All Clear Emergency Management Group for use with the State of Vermont. Content used for this presentation, where applicable, has been sourced from various public documents or from the author’s personal materials. Copyright for papers published in academic journals, in their final form, are maintained by those respective journals. The purpose of this project is to provide education for those involved in emergency care for those with a burn injury. Reuse of this material in their current format is restricted to All Clear Emergency Management Group for use with the State of Vermont. All other rights to the materials are retained by the author.
Fair Use and Disclaimer Images and other content found throughout this presentation are either cited for their original source, are owned by the author of this work or were commonly found on the world wide web and not identified as being protected images (copyright). These images and this content are used and protected based on the Fair Use Doctrine. Copyright Disclaimer Under Section 107 of the Copyright Act 1976, allowance is made for "fair use" for purposes such as criticism, comment, news reporting, teaching, scholarship, and research. Fair use is a use permitted by copyright statute that might otherwise be infringing. Non-profit, educational or personal use tips the balance in favor of fair use. If for any reason you see an image that may in fact be copyrighted or you find objectionable, please notify us immediately.