Behavioral Health and Primary Care Integration
11 Slides61.50 KB

Behavioral Health and Primary Care Integration Administrative Infrastructure Issues Diana Knaebe, President/CEO Heritage Behavioral Health Center Decatur, IL
So you want to integrate primary and behavioral health care Things to consider – What are you hoping to achieve – For what purpose – What is it going to take – What do you need to consider – Have you identified partner entities
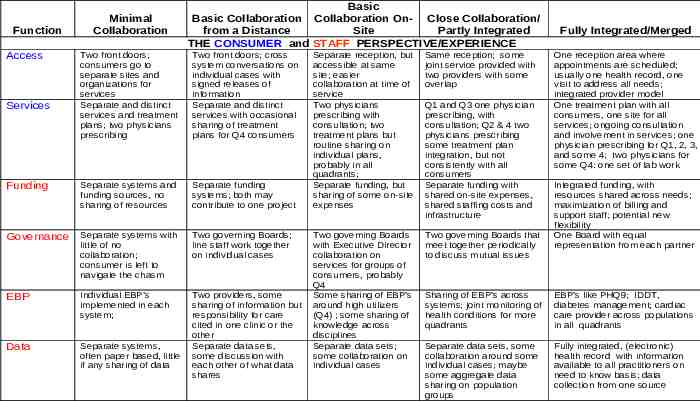
Function Access Minimal Collaboration Basic Basic Collaboration Collaboration On- Close Collaboration/ from a Distance Site Partly Integrated THE CONSUMER and STAFF PERSPECTIVE/EXPERIENCE Two front doors; consumers go to separate sites and organizations for services Separate and distinct services and treatment plans; two physicians prescribing Two front doors; cross system conversations on individual cases with signed releases of information Separate and distinct services with occasional sharing of treatment plans for Q4 consumers Funding Separate systems and funding sources, no sharing of resources Separate funding systems; both may contribute to one project Governance Separate systems with little of no collaboration; consumer is left to navigate the chasm Two governing Boards; line staff work together on individual cases EBP Individual EBP’s implemented in each system; Data Separate systems, often paper based, little if any sharing of data Two providers, some sharing of information but responsibility for care cited in one clinic or the other Separate data sets, some discussion with each other of what data shares Services Separate reception, but accessible at same site; easier collaboration at time of service Two physicians prescribing with consultation; two treatment plans but routine sharing on individual plans, probably in all quadrants; Separate funding, but sharing of some on-site expenses Same reception; some joint service provided with two providers with some overlap Two governing Boards with Executive Director collaboration on services for groups of consumers, probably Q4 Some sharing of EBP’s around high utilizers (Q4) ; some sharing of knowledge across disciplines Separate data sets; some collaboration on individual cases Two governing Boards that meet together periodically to discuss mutual issues Q1 and Q3 one physician prescribing, with consultation; Q2 & 4 two physicians prescribing some treatment plan integration, but not consistently with all consumers Separate funding with shared on-site expenses, shared staffing costs and infrastructure Fully Integrated/Merged One reception area where appointments are scheduled; usually one health record, one visit to address all needs; integrated provider model One treatment plan with all consumers, one site for all services; ongoing consultation and involvement in services; one physician prescribing for Q1, 2, 3, and some 4; two physicians for some Q4: one set of lab work Integrated funding, with resources shared across needs; maximization of billing and support staff; potential new flexibility One Board with equal representation from each partner Sharing of EBP’s across systems; joint monitoring of health conditions for more quadrants EBP’s like PHQ9; IDDT, diabetes management; cardiac care provider across populations in all quadrants Separate data sets, some collaboration around some individual cases; maybe some aggregate data sharing on population groups Fully integrated, (electronic) health record with information available to all practitioners on need to know basis; data collection from one source
Administrative Infrastructure Issues Ready, Set, Go? – Maybe we better make sure we understand where each organization is coming from first Levels of Integration – Does each organization have a goal in mind? Has this been articulated? – Does not have to be total integration/merger
Administrative Infrastructure Issues Intentions – What is each organization hoping to achieve? – May need to spend a considerable amount of time determining this up front. – Different languages/cultures – Corporate values/philosophies – What does the partnership mean to each entity?
Identifying your Target Population How was the population identified? – Four Quadrant – Looking at payer source What common characteristic(s) does your target population share besides their SMI status? – Usually economically disadvantaged – indigent, Medicaid, complicated physical issues – diagnoses

Administrative Infrastructure Issues Physical Space – Where located – Co-location Some primary care services at behavioral health center Some behavioral health services at primary care Total shared space
Administrative Infrastructure Issues Establishment of Expectations, Outcomes – Financial Benchmarks Who bills for what services How much revenue is currently anticipated/actual If working to maximize revenue, will this be shared, how?
Administrative Infrastructure Issues – Clinical Expectations – what is the expected volume encounters/productivity – Staffing – what is the model Who hires whom, philosophy of staff if at off site How many hours at site How are staff regarded Supervision On-going clinical meetings – Conflict resolution pathways – Clinical Protocols – Standardized Care » Best Practices
Administrative infrastructure continued Process is Developmental and Incremental – Takes some risk on parties involved – Lots of patience – Trust – going back to intention – Continues to Evolve – Keep going back to your intentions, which may also change and evolve over time
Resource The SAMHSA-HRSA Center for Integrated Health Solutions, run by the National Council for Community Behavioral Healthcare under a cooperative agreement from the U.S. Department of Health and Human Services, is funded jointly by the Substance Abuse and Mental Health Services Administration and the Health Resources Services Administration. The CIHS promotes the development of integrated primary and behavioral health services to better address the needs of individuals with mental health and substance use conditions, whether seen in specialty behavioral health or primary care provider settings. – http://www.thenationalcouncil.org/cs/ center for integrated health solutions