Centers for Disease Control and Prevention National Center for
16 Slides2.79 MB
Centers for Disease Control and Prevention National Center for Emerging and Zoonotic Infectious Diseases IPC for Marburg Virus Disease (MVD): Waste Management Part 2: Final Waste Disposal Healthcare Settings with Limited to Intermediate Resources Updated: March 2023
Learning Objectives After this presentation, participants will be able to ‒ Explain why proper waste disposal during a Marburg virus disease outbreak is important ‒ Identify ways to improve final waste disposal at their own facilities.
Discuss Once waste has been collected from the waste bins in your facility, how is waste disposed of? Does waste disposal differ for general waste, infectious waste, or other kinds of waste collected? If so, how?

Waste Disposal
Why Is Waste Disposal Important? Inappropriate waste management poses potential health risks to you, your patients and other staff in your facility, as well as to your community. Potential risks: – Exposure to items contaminated with Marburg virus (e.g., contaminated gloves) – Exposure to sharp items that pose a risk of physical injury as well as exposure to Marburg virus (e.g., used needles)
Waste Disposal Healthcare facilities must have a functional system for the final disposal of waste Infectious and potentially infectious waste must be: – Incinerated OR – Treated with non-burn treatment (autoclaving/grinding or other alternative treatment) before being placed in regular waste stream OR – Buried
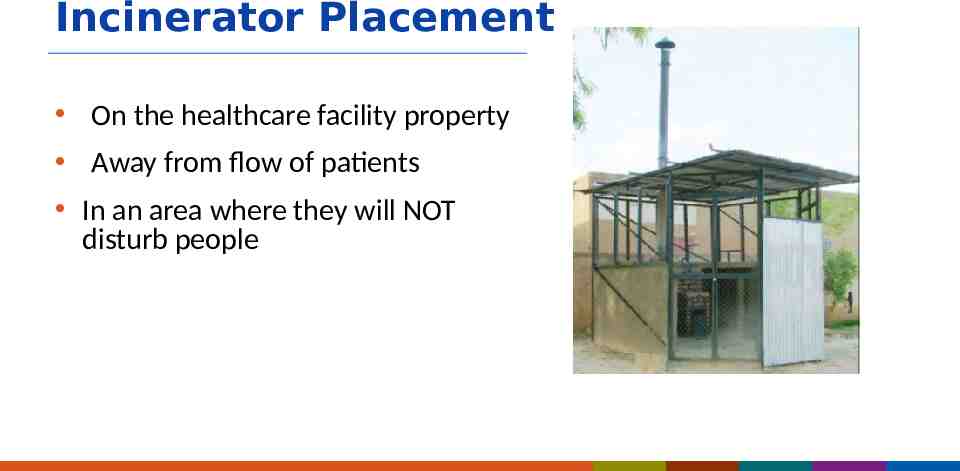
Incinerator Placement On the healthcare facility property Away from flow of patients In an area where they will NOT disturb people
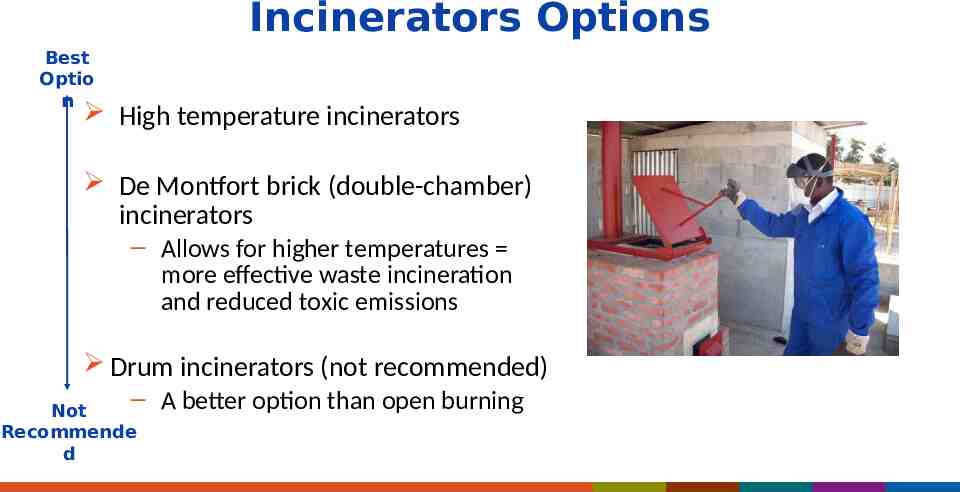
Incinerators Options Best Optio n High temperature incinerators De Montfort brick (double-chamber) incinerators – Allows for higher temperatures more effective waste incineration and reduced toxic emissions Drum incinerators (not recommended) – A better option than open burning Not Recommende d
Interim Option: Burn Pits Generally, it is best to avoid open burning of healthcare waste – releases toxic gases – does not reach high enough temperatures to fully destroy infectious waste In emergencies, burn pits can be used until incinerators or other treatment methods (such as autoclaves) become available.
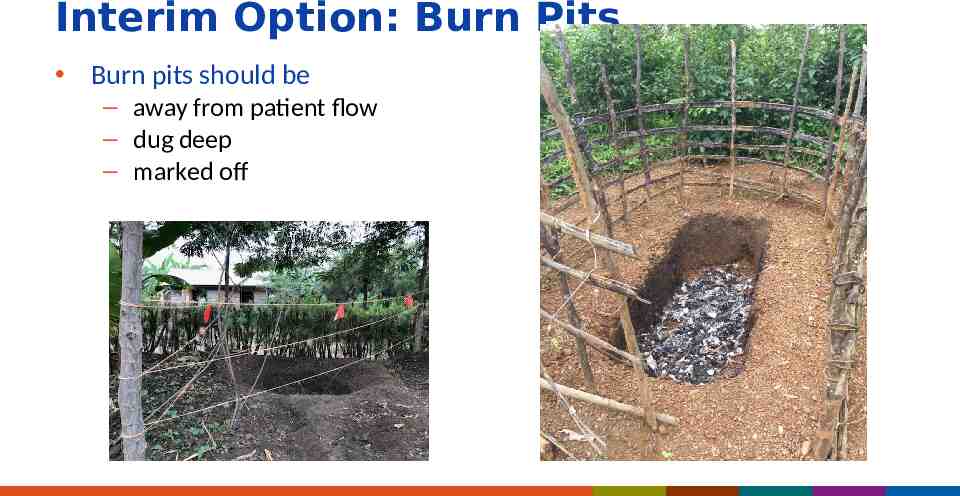
Interim Option: Burn Pits (continued) Burn pits should be – away from patient flow – dug deep – marked off
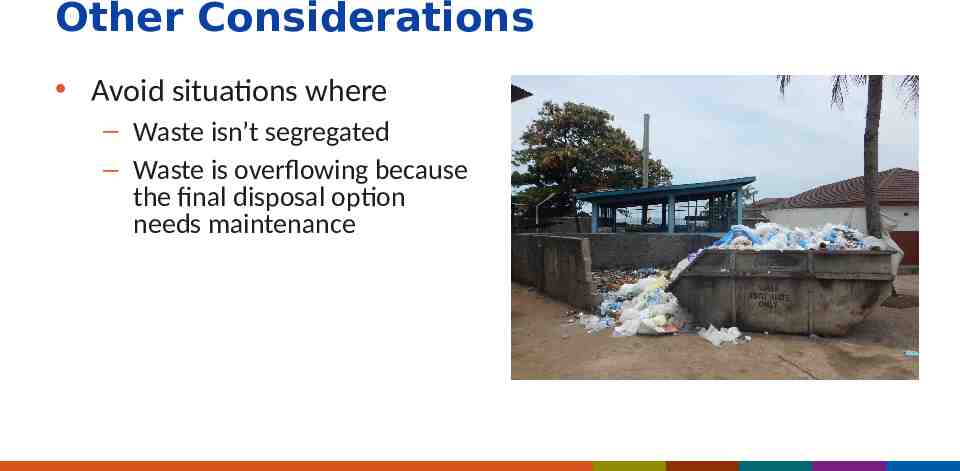
Other Considerations Avoid situations where – Waste isn’t segregated – Waste is overflowing because the final disposal option needs maintenance
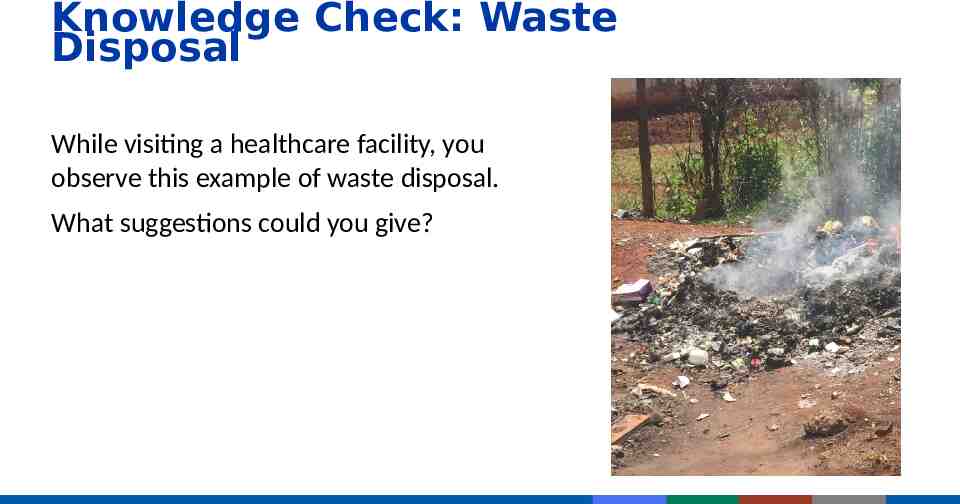
Knowledge Check: Waste Disposal While visiting a healthcare facility, you observe this example of waste disposal. What suggestions could you give?
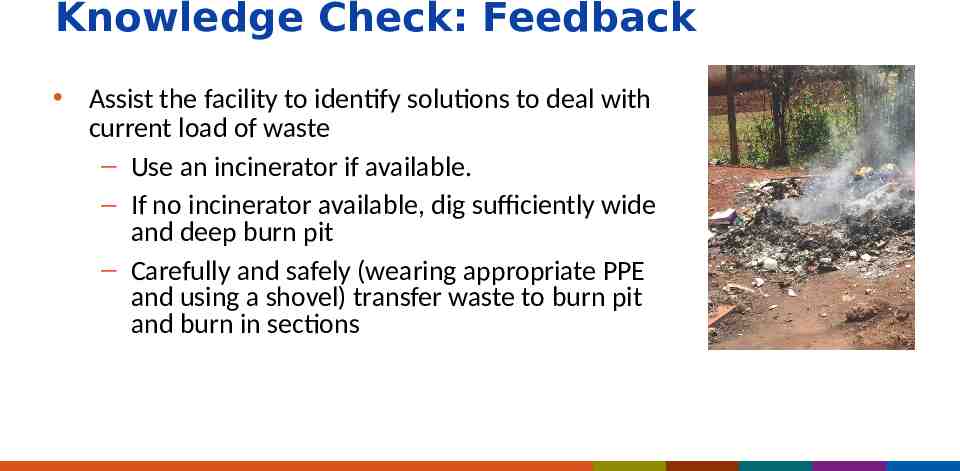
Knowledge Check: Feedback Assist the facility to identify solutions to deal with current load of waste – Use an incinerator if available. – If no incinerator available, dig sufficiently wide and deep burn pit – Carefully and safely (wearing appropriate PPE and using a shovel) transfer waste to burn pit and burn in sections
Reflection Where is final waste disposal at your facility? What maintenance might be needed? Is there capacity to take on additional waste (e.g., isolation units, additional PPE waste)? What resources, such as fuel for burning waste and transport equipment, might be needed?
Key Takeaways Proper medical waste disposal during a Marburg virus disease outbreak is crucial to keep you, others at your facility, and your community safe. A high temperature incinerator is the best option for incinerating medical waste. If a burn pit must be used as an interim option, it should be away from patient flow, dug deep, and marked off.
Thank you! For more information, contact CDC 1-800-CDC-INFO (232-4636) TTY: 1-888-232-6348 www.cdc.gov The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.