Workshop: Trauma-Informed Integrated Care for Families and Children
67 Slides4.02 MB
Workshop: Trauma-Informed Integrated Care for Families and Children August 9, 2016 Pediatric Integrated Care Collaborative (PICC)
Workshop Objectives Participants will be able to: Define trauma-informed integrated care and identify core components and functions present across different models Identify strengths, challenges, and areas of focus for implementing trauma-informed integrated care in your community Propose next steps to create trauma-informed integrated care programs in your community Pediatric Integrated Care Collaborative (PICC)
Agenda 1. Welcome and Introductions (I hr.) 2. Overview of trauma-informed integrated care (45 min.) 3. Identify challenges/success (15 min.) 4. Smaller group discussions (1.5 hrs.) 5. What is a PDSA? (15 min.) 6. Action planning (1.5 hrs.) 7. Discussion (I hr.) Pediatric Integrated Care Collaborative (PICC)
Welcome Jerry Waukau and Diane Hietpas Pediatric Integrated Care Collaborative (PICC)

Pediatric Integrated Care Collaborative (PICC)
Building a Culture of Health Imagine living in a community making sure the health of all of our children is a matter of fact and not a matter of chance. Imagine knowing that all of our employers, our mayors, our educators and our faith leaders were working together to give everyone the tools and the opportunities they need to make responsible choices. A Culture of Health means living in a society that not only believes but also insists that every person has the chance to be as healthy as they can be. Risa Lavizzo-Mourey, MD, MBA, President & Chief Executive Officer, RWJF (in an interview with AARP, Sept. 2014) Pediatric Integrated Care Collaborative (PICC)
Pediatric Integrated Care Collaborative (PICC)
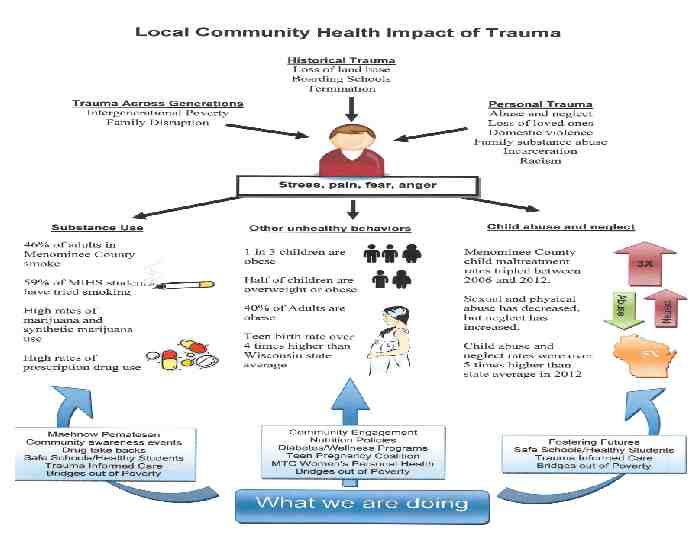
Menominee Nation Wisconsin’s oldest continuous residents Only WI Tribe inhabiting ancestral lands Treaties reduced Tribal lands from 10 million acres to the current 235,523 acres Maintains the country’s largest sustainable forest 9,000 Tribal members, 4000 residing on the reservation Tribal members have shown tremendous resilience Ranked 72 out of 72 WI counties in Public Health Outcomes Pediatric Integrated Care Collaborative (PICC)
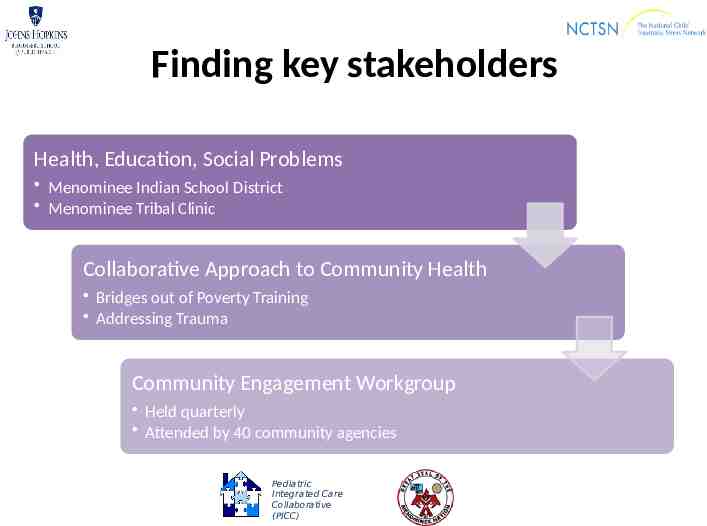
Finding key stakeholders Health, Education, Social Problems Menominee Indian School District Menominee Tribal Clinic Collaborative Approach to Community Health Bridges out of Poverty Training Addressing Trauma Community Engagement Workgroup Held quarterly Attended by 40 community agencies Pediatric Integrated Care Collaborative (PICC)
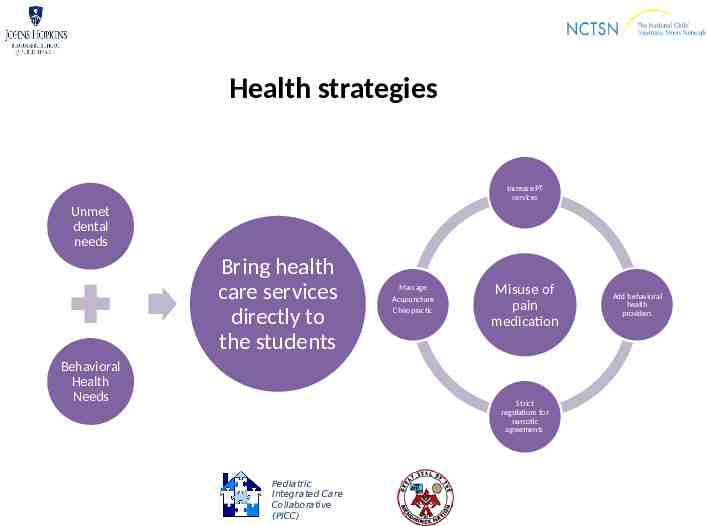
Health strategies Increase PT services Unmet dental needs Bring health care services directly to the students Behavioral Health Needs Massage Acupuncture Chiropractic Misuse of pain medication Strict regulations for narcotic agreements Pediatric Integrated Care Collaborative (PICC) Add behavioral health providers
Pediatric Integrated Care Collaborative (PICC)
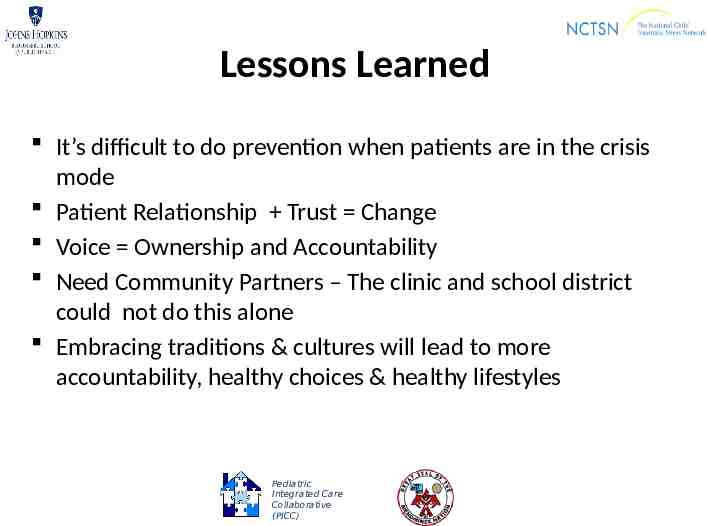
Lessons Learned It’s difficult to do prevention when patients are in the crisis mode Patient Relationship Trust Change Voice Ownership and Accountability Need Community Partners – The clinic and school district could not do this alone Embracing traditions & cultures will lead to more accountability, healthy choices & healthy lifestyles Pediatric Integrated Care Collaborative (PICC)
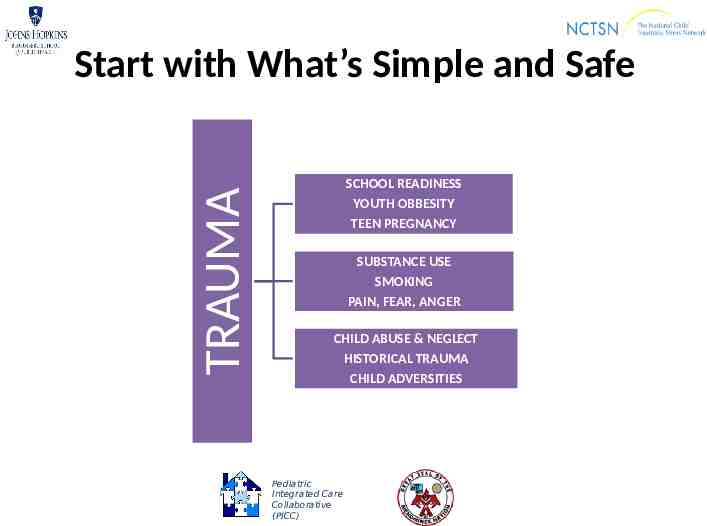
TRAUMA Start with What’s Simple and Safe SCHOOL READINESS YOUTH OBBESITY TEEN PREGNANCY SUBSTANCE USE SMOKING PAIN, FEAR, ANGER CHILD ABUSE & NEGLECT HISTORICAL TRAUMA CHILD ADVERSITIES Pediatric Integrated Care Collaborative (PICC)
Successes Vietnam Combat Veteran taught us to “Connect the Dots” Community Engagement Workgroup including 90 day plans of action Increase community awareness of trauma Training and workforce development with a trauma focus Accountability Pediatric Integrated Care Collaborative (PICC)
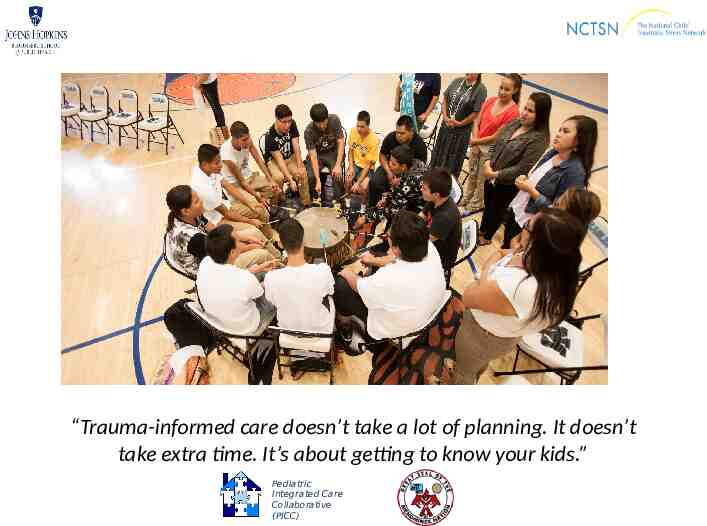
“Trauma-informed care doesn’t take a lot of planning. It doesn’t take extra time. It’s about getting to know your kids.” Pediatric Integrated Care Collaborative (PICC)
https://youtu.be/WOpewNNwwiI Pediatric Integrated Care Collaborative (PICC)
Introductions Jen Agosti Pediatric Integrated Care Collaborative (PICC)
Welcome and Introductions Around your table . Personal Introduction (name and where you’re from) What do you most hope to get from this day? What is your greatest passion/joy in working with children and families? Pediatric Integrated Care Collaborative (PICC)
What Is Trauma? Maegan Rides at the Door Pediatric Integrated Care Collaborative (PICC)
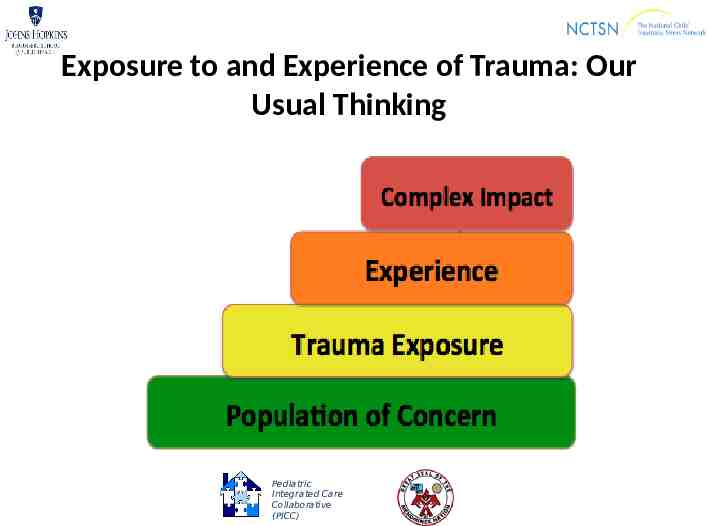
Exposure to and Experience of Trauma: Our Usual Thinking Pediatric Integrated Care Collaborative (PICC)
Complex trauma Victim of violence (physical, sexual, emotional) from caregivers, peers, others Neglect (insecurity with regard to emotional and concrete support from primary caregiver) Witnessing violence within and outside family Living in situation of sustained adversity with threats to safety, security and other basic needs Pediatric Integrated Care Collaborative (PICC)
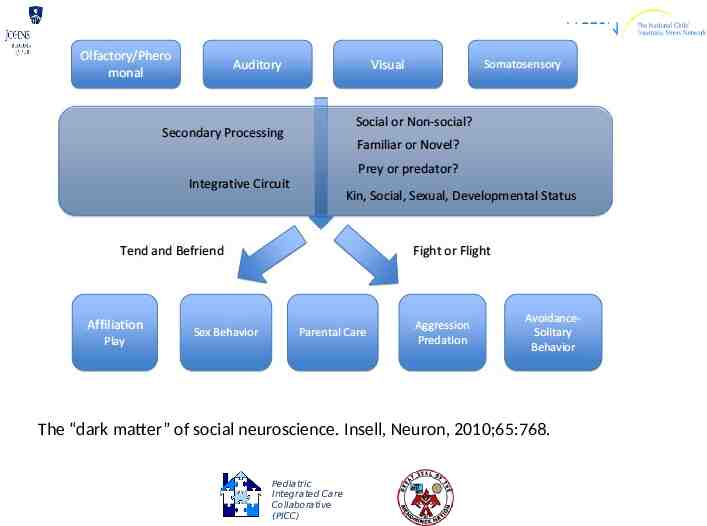
The “dark matter” of social neuroscience. Insell, Neuron, 2010;65:768. Pediatric Integrated Care Collaborative (PICC)
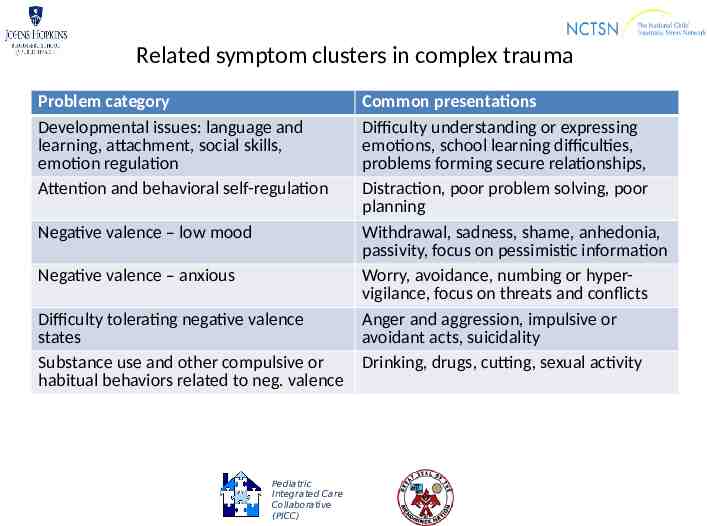
Related symptom clusters in complex trauma Problem category Developmental issues: language and learning, attachment, social skills, emotion regulation Attention and behavioral self-regulation Negative valence – low mood Negative valence – anxious Difficulty tolerating negative valence states Substance use and other compulsive or habitual behaviors related to neg. valence Pediatric Integrated Care Collaborative (PICC) Common presentations Difficulty understanding or expressing emotions, school learning difficulties, problems forming secure relationships, Distraction, poor problem solving, poor planning Withdrawal, sadness, shame, anhedonia, passivity, focus on pessimistic information Worry, avoidance, numbing or hypervigilance, focus on threats and conflicts Anger and aggression, impulsive or avoidant acts, suicidality Drinking, drugs, cutting, sexual activity
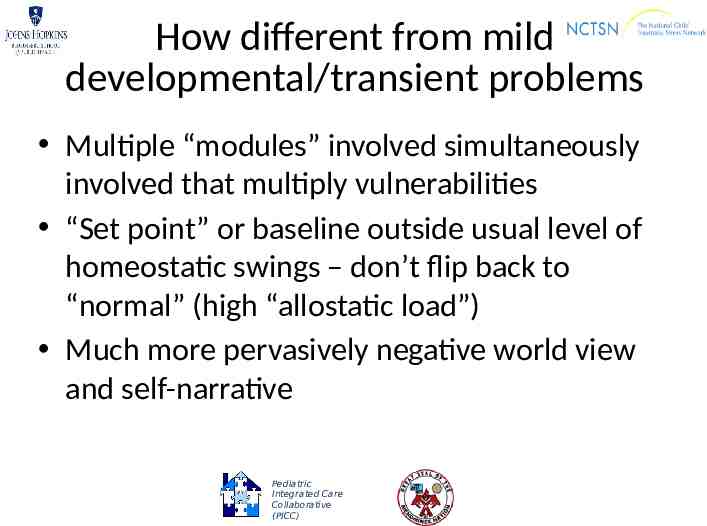
How different from mild developmental/transient problems Multiple “modules” involved simultaneously involved that multiply vulnerabilities “Set point” or baseline outside usual level of homeostatic swings – don’t flip back to “normal” (high “allostatic load”) Much more pervasively negative world view and self-narrative Pediatric Integrated Care Collaborative (PICC)
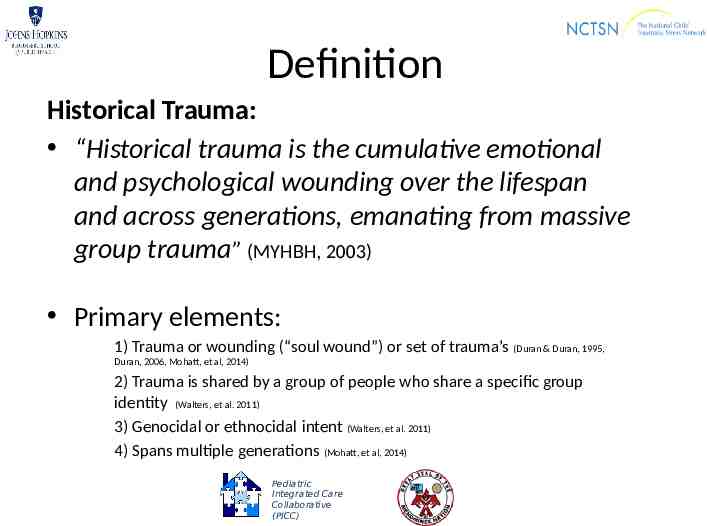
Definition Historical Trauma: “Historical trauma is the cumulative emotional and psychological wounding over the lifespan and across generations, emanating from massive group trauma” (MYHBH, 2003) Primary elements: 1) Trauma or wounding (“soul wound”) or set of trauma’s (Duran & Duran, 1995, Duran, 2006, Mohatt, et al, 2014) 2) Trauma is shared by a group of people who share a specific group identity (Walters, et al. 2011) 3) Genocidal or ethnocidal intent (Walters, et al. 2011) 4) Spans multiple generations (Mohatt, et al, 2014) Pediatric Integrated Care Collaborative (PICC)
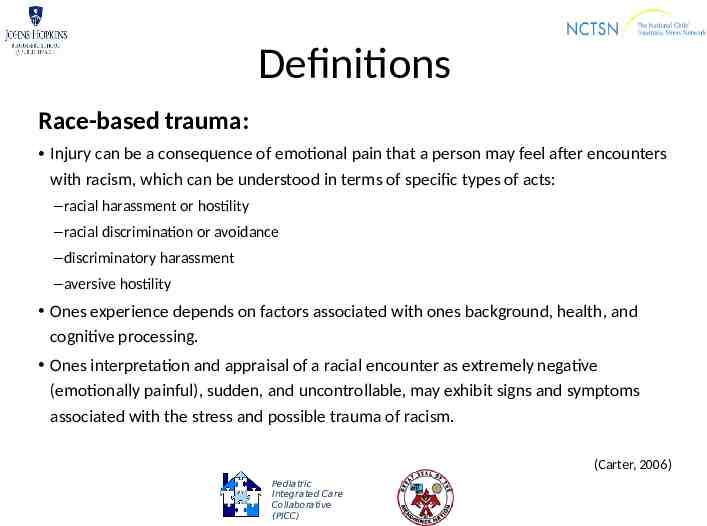
Definitions Race-based trauma: Injury can be a consequence of emotional pain that a person may feel after encounters with racism, which can be understood in terms of specific types of acts: – racial harassment or hostility – racial discrimination or avoidance – discriminatory harassment – aversive hostility Ones experience depends on factors associated with ones background, health, and cognitive processing. Ones interpretation and appraisal of a racial encounter as extremely negative (emotionally painful), sudden, and uncontrollable, may exhibit signs and symptoms associated with the stress and possible trauma of racism. (Carter, 2006) Pediatric Integrated Care Collaborative (PICC)
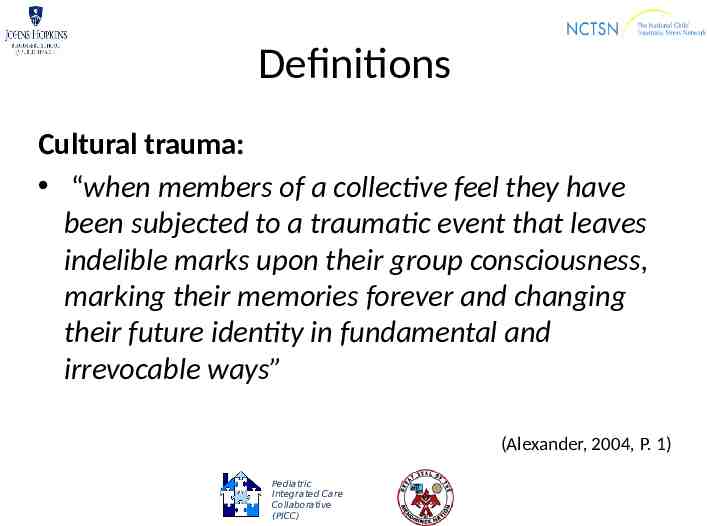
Definitions Cultural trauma: “when members of a collective feel they have been subjected to a traumatic event that leaves indelible marks upon their group consciousness, marking their memories forever and changing their future identity in fundamental and irrevocable ways” (Alexander, 2004, P. 1) Pediatric Integrated Care Collaborative (PICC)
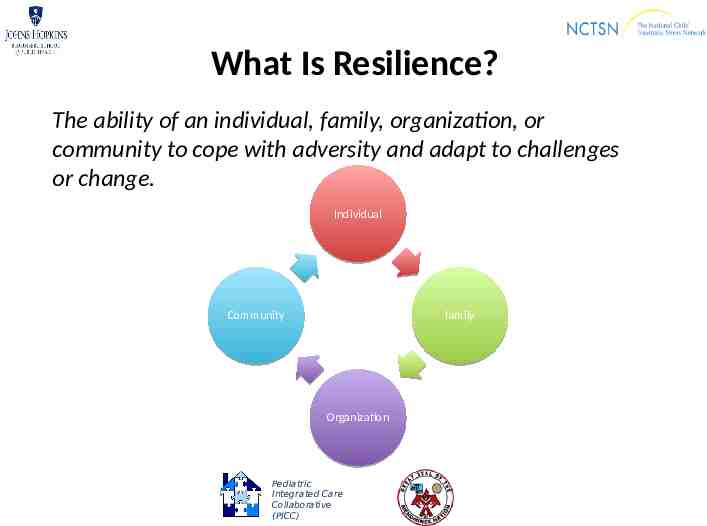
What Is Resilience? The ability of an individual, family, organization, or community to cope with adversity and adapt to challenges or change. Individual Community family Organization Pediatric Integrated Care Collaborative (PICC)
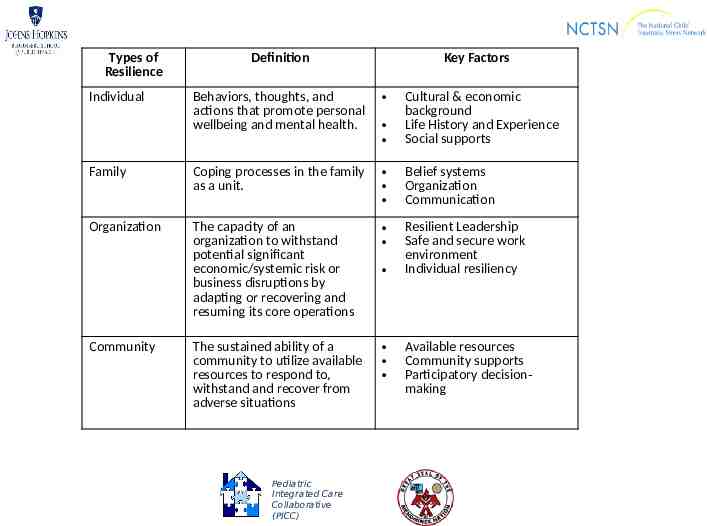
Types of Resilience Definition Key Factors Behaviors, thoughts, and actions that promote personal wellbeing and mental health. Cultural & economic background Life History and Experience Social supports Family Coping processes in the family as a unit. Belief systems Organization Communication Organization The capacity of an organization to withstand potential significant economic/systemic risk or business disruptions by adapting or recovering and resuming its core operations Resilient Leadership Safe and secure work environment Individual resiliency The sustained ability of a community to utilize available resources to respond to, withstand and recover from adverse situations Individual Community Pediatric Integrated Care Collaborative (PICC) Available resources Community supports Participatory decisionmaking
What Is Trauma-Informed Integrated Care? Larry Wissow, Maegan Rides at the Door, Jerry Waukau, and Diane Hietpas Pediatric Integrated Care Collaborative (PICC)
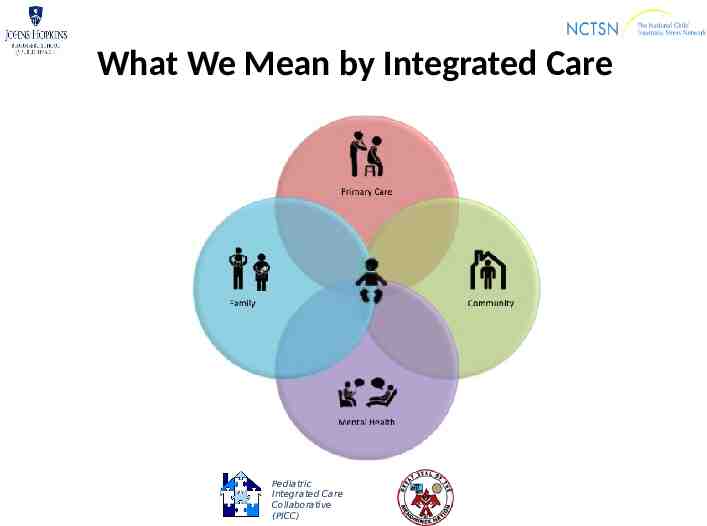
What We Mean by Integrated Care Pediatric Integrated Care Collaborative (PICC)
What Is the Pediatric Integrated Care Collaborative (PICC)? Goal of PICC: Improve access to trauma prevention and treatment services for families with young children Part of the National Child Traumatic Stress Network (NCTSN, www.nctsn.org), funded by the Substance Abuse and Mental Health Services Administration (SAMHSA) NCTSN grant focused on: – Integrated Care Collaborative (I-Care) – One BSC two LCs PICC Toolkit Pediatric Integrated Care Collaborative (PICC)
Overall Frame for PICC Collaborative Change Framework (CCF) Mission “ find practical, sustainable ways to integrate trauma/chronic stress prevention, detection, and early intervention into primary care for young children.” Pediatric Integrated Care Collaborative (PICC)
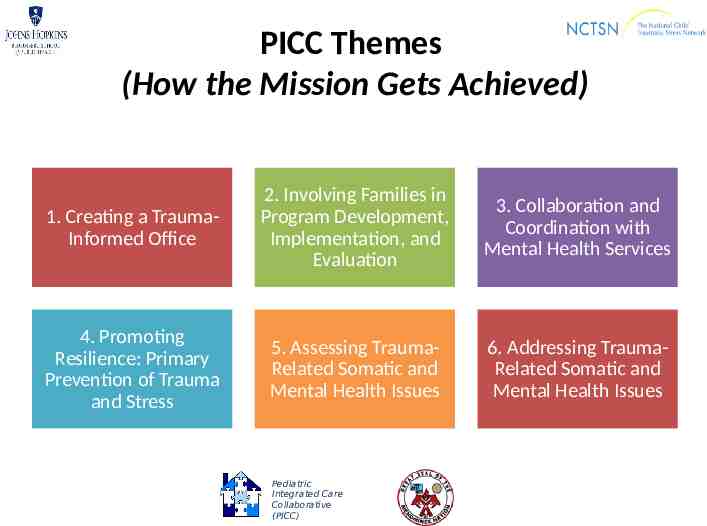
PICC Themes (How the Mission Gets Achieved) 1. Creating a TraumaInformed Office 2. Involving Families in Program Development, Implementation, and Evaluation 3. Collaboration and Coordination with Mental Health Services 4. Promoting Resilience: Primary Prevention of Trauma and Stress 5. Assessing TraumaRelated Somatic and Mental Health Issues 6. Addressing TraumaRelated Somatic and Mental Health Issues Pediatric Integrated Care Collaborative (PICC)
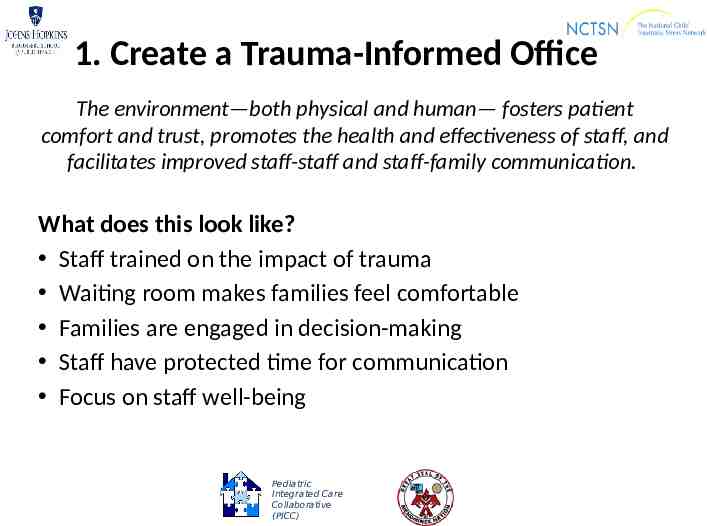
1. Create a Trauma-Informed Office The environment—both physical and human— fosters patient comfort and trust, promotes the health and effectiveness of staff, and facilitates improved staff-staff and staff-family communication. What does this look like? Staff trained on the impact of trauma Waiting room makes families feel comfortable Families are engaged in decision-making Staff have protected time for communication Focus on staff well-being Pediatric Integrated Care Collaborative (PICC)
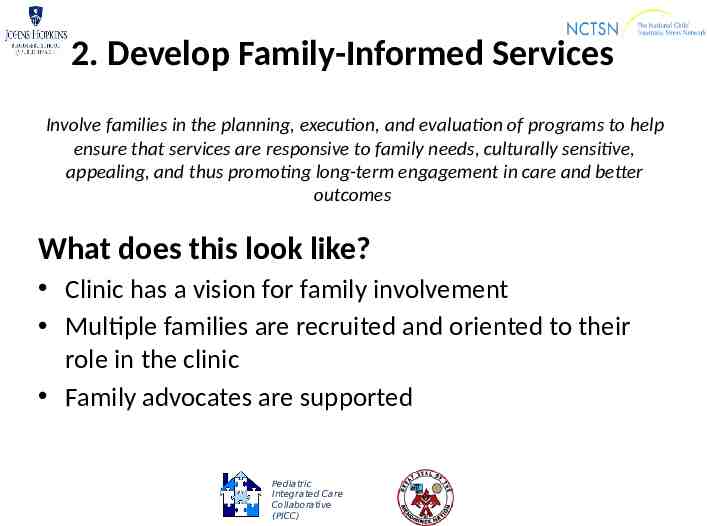
2. Develop Family-Informed Services Involve families in the planning, execution, and evaluation of programs to help ensure that services are responsive to family needs, culturally sensitive, appealing, and thus promoting long-term engagement in care and better outcomes What does this look like? Clinic has a vision for family involvement Multiple families are recruited and oriented to their role in the clinic Family advocates are supported Pediatric Integrated Care Collaborative (PICC)

3. Enhance Collaboration Between Behavioral Health and Primary Care Services Positive relationships between primary care and behavioral health providers has the potential to promote engagement in treatment necessary for positive outcomes and create pathways across which information can flow safely and efficiently, so that services are most likely to meet patients’ needs and preferences. What does this look like? Identified partnership between behavioral health and primary care providers Integrated behavioral health partner into primary care practice Coordinated communication system Pediatric Integrated Care Collaborative (PICC)
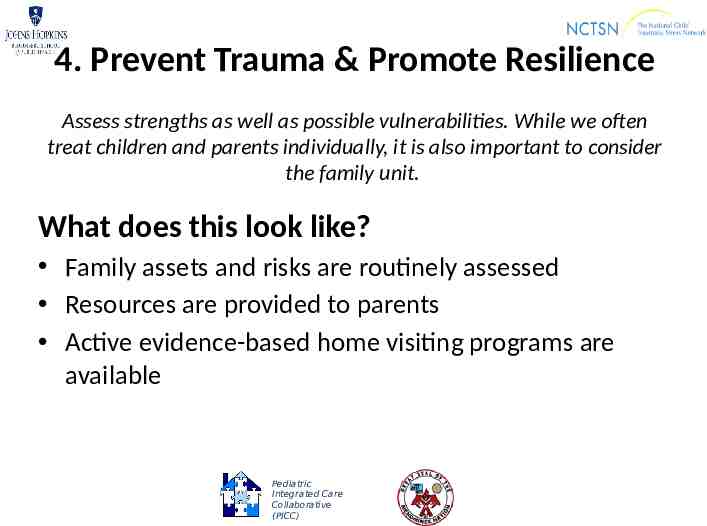
4. Prevent Trauma & Promote Resilience Assess strengths as well as possible vulnerabilities. While we often treat children and parents individually, it is also important to consider the family unit. What does this look like? Family assets and risks are routinely assessed Resources are provided to parents Active evidence-based home visiting programs are available Pediatric Integrated Care Collaborative (PICC)
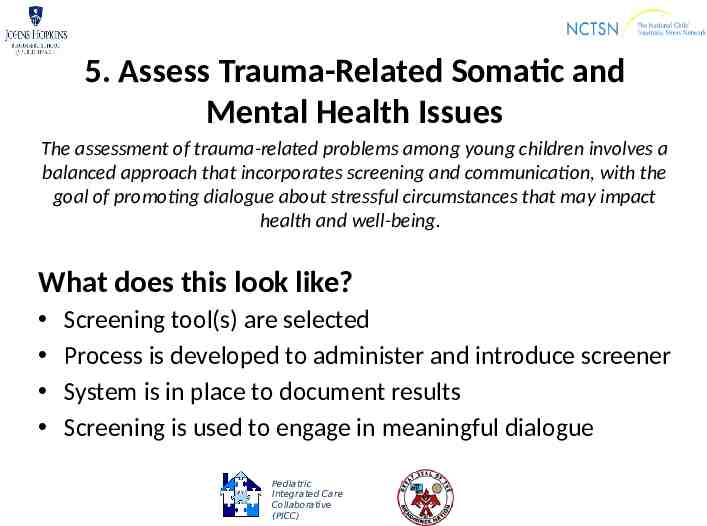
5. Assess Trauma-Related Somatic and Mental Health Issues The assessment of trauma-related problems among young children involves a balanced approach that incorporates screening and communication, with the goal of promoting dialogue about stressful circumstances that may impact health and well-being. What does this look like? Screening tool(s) are selected Process is developed to administer and introduce screener System is in place to document results Screening is used to engage in meaningful dialogue Pediatric Integrated Care Collaborative (PICC)
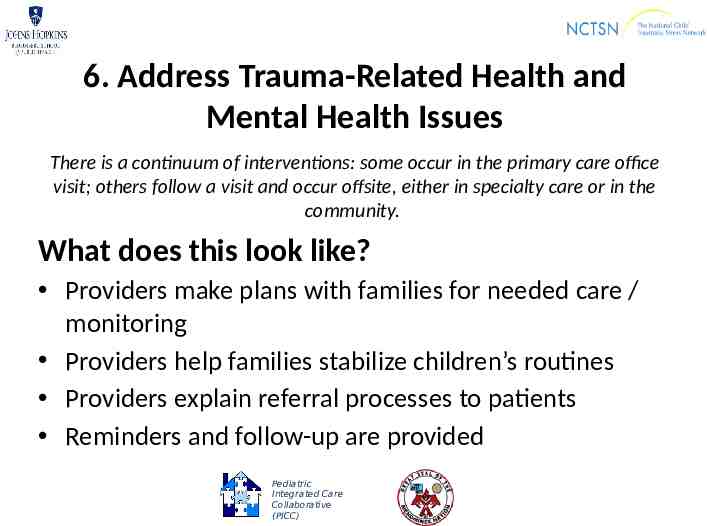
6. Address Trauma-Related Health and Mental Health Issues There is a continuum of interventions: some occur in the primary care office visit; others follow a visit and occur offsite, either in specialty care or in the community. What does this look like? Providers make plans with families for needed care / monitoring Providers help families stabilize children’s routines Providers explain referral processes to patients Reminders and follow-up are provided Pediatric Integrated Care Collaborative (PICC)
Reflecting on Where You Are Jen Agosti Pediatric Integrated Care Collaborative (PICC)

Theme Areas on the Self-Reflection Creating a TraumaInformed Office Family Involvement Collaboration and Coordination Promoting Resilience: Primary Prevention of Trauma Assessing TraumaRelated Somatic and Mental Health Issues Addressing TraumaRelated Somatic and Mental Health Issues Pediatric Integrated Care Collaborative (PICC)
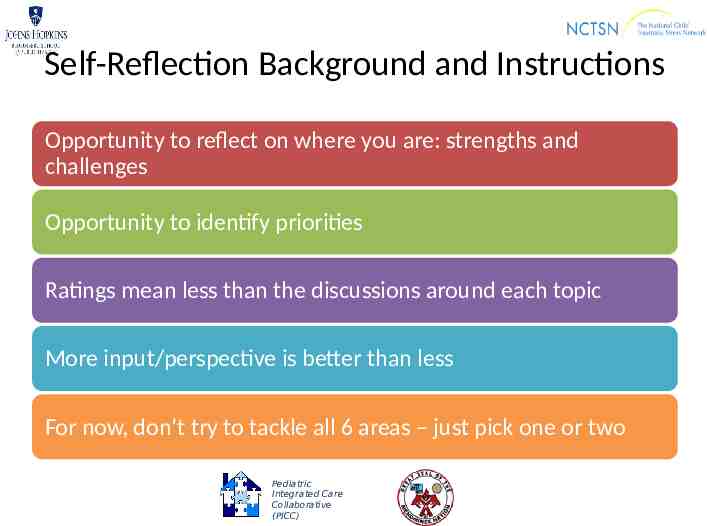
Self-Reflection Background and Instructions Opportunity to reflect on where you are: strengths and challenges Opportunity to identify priorities Ratings mean less than the discussions around each topic More input/perspective is better than less For now, don’t try to tackle all 6 areas – just pick one or two Pediatric Integrated Care Collaborative (PICC)
Breakout Sessions Small Group Facilitators Pediatric Integrated Care Collaborative (PICC)
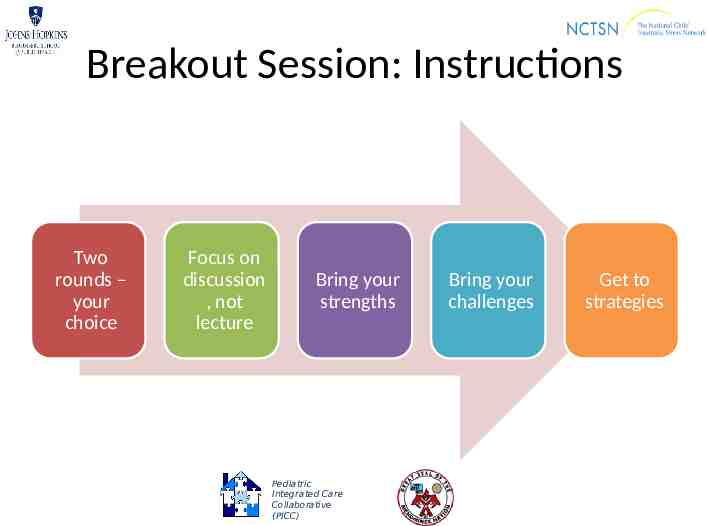
Breakout Session: Instructions Two rounds – your choice Focus on discussion , not lecture Bring your strengths Pediatric Integrated Care Collaborative (PICC) Bring your challenges Get to strategies
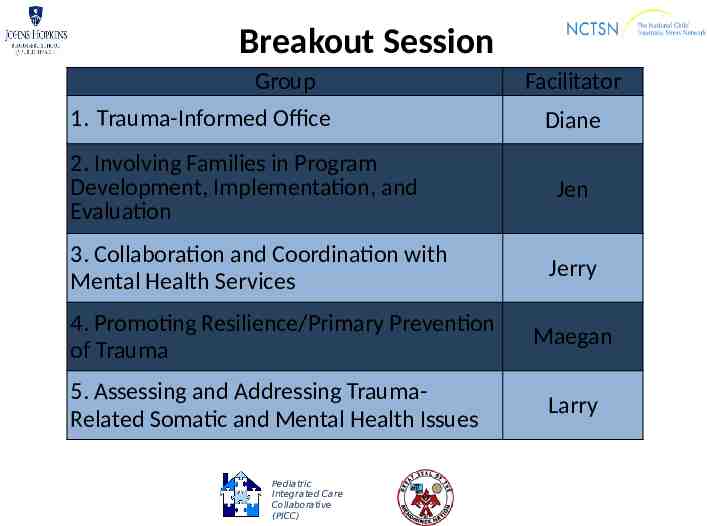
Breakout Session Group 1. Trauma-Informed Office 2. Involving Families in Program Development, Implementation, and Evaluation 3. Collaboration and Coordination with Mental Health Services 4. Promoting Resilience/Primary Prevention of Trauma 5. Assessing and Addressing TraumaRelated Somatic and Mental Health Issues Pediatric Integrated Care Collaborative (PICC) Facilitator Diane Jen Jerry Maegan Larry
Highlights from Breakout Sessions In 3 min (or less) share one or two highlights / pearls from the session Pediatric Integrated Care Collaborative (PICC)
Accelerating Improvement Jen Agosti Pediatric Integrated Care Collaborative (PICC)
Moving to PDSAs (Tool to Support SUSTAINABLE Improvement) Test hunches quickly (by getting & studying results) Multiple hunches can be tested simultaneously Identify problems while they have minimal impact Get buy-in as you go based on proof of success Always have the end in mind: What Am I Trying to Accomplish AND How Will I Ensure It Will Be Sustained? Adapted from 2001 Institute for Healthcare Improvement Pediatric Integrated Care Collaborative (PICC)
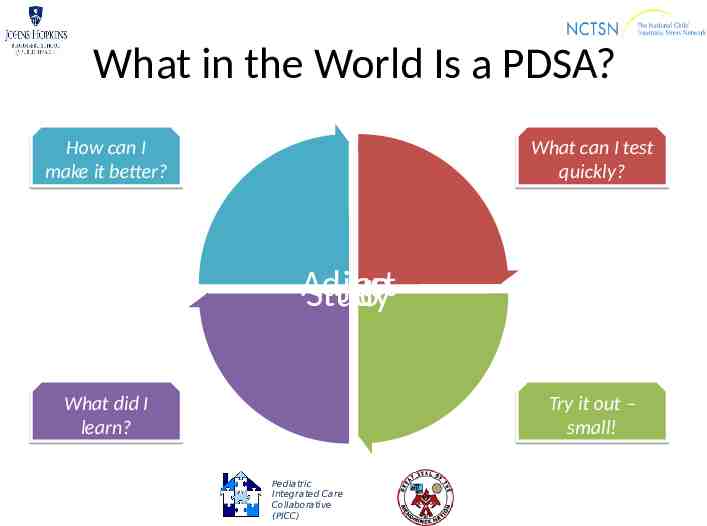
What in the World Is a PDSA? How can I make it better? What can I test quickly? Adjust Plan Study Do What did I learn? Try it out – small! Pediatric Integrated Care Collaborative (PICC)
An Example: Moving from Broad Strategy to PDSA (small test) What changes can we make that will result in improvement? Provide guidance that promotes development of resilience and wellness ENDLESS Number of Ideas to Test – Share written information with parents during child well-being visits – Use parent advocates / liaisons to talk with parents about positive parenting – Offer parent coaching / parenting sessions during clinic hours – Incorporate questions on positive parenting into well-being visits – Use Talking Points to help staff talk about positive parenting and resilience – And so on . Pediatric Integrated Care Collaborative (PICC)
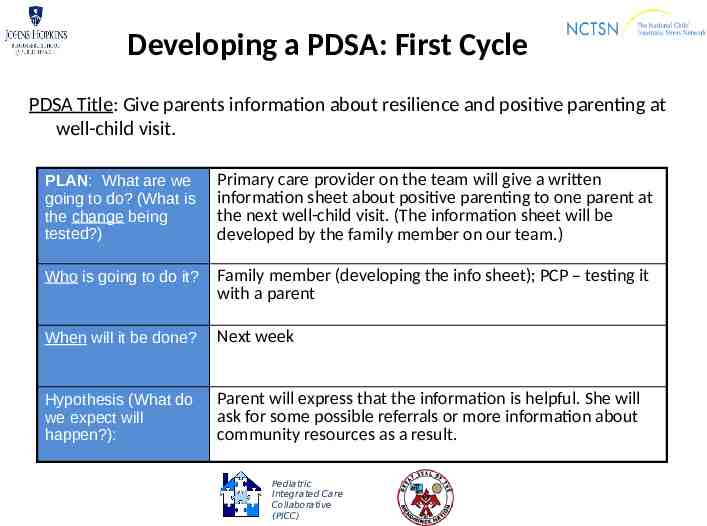
Developing a PDSA: First Cycle PDSA Title: Give parents information about resilience and positive parenting at well-child visit. PLAN: What are we going to do? (What is the change being tested?) Primary care provider on the team will give a written information sheet about positive parenting to one parent at the next well-child visit. (The information sheet will be developed by the family member on our team.) Who is going to do it? Family member (developing the info sheet); PCP – testing it with a parent When will it be done? Next week Hypothesis (What do we expect will happen?): Parent will express that the information is helpful. She will ask for some possible referrals or more information about community resources as a result. Pediatric Integrated Care Collaborative (PICC)
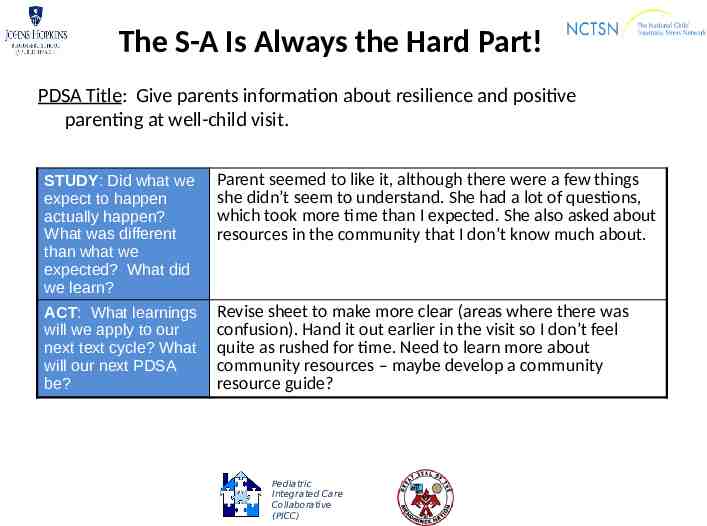
The S-A Is Always the Hard Part! PDSA Title: Give parents information about resilience and positive parenting at well-child visit. STUDY: Did what we expect to happen actually happen? What was different than what we expected? What did we learn? Parent seemed to like it, although there were a few things she didn’t seem to understand. She had a lot of questions, which took more time than I expected. She also asked about resources in the community that I don’t know much about. ACT: What learnings will we apply to our next text cycle? What will our next PDSA be? Revise sheet to make more clear (areas where there was confusion). Hand it out earlier in the visit so I don’t feel quite as rushed for time. Need to learn more about community resources – maybe develop a community resource guide? Pediatric Integrated Care Collaborative (PICC)
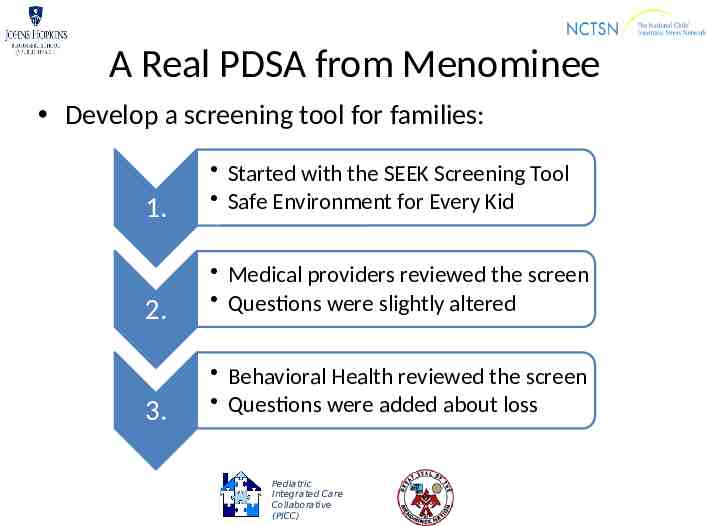
A Real PDSA from Menominee Develop a screening tool for families: 1. Started with the SEEK Screening Tool Safe Environment for Every Kid 2. Medical providers reviewed the screen Questions were slightly altered 3. Behavioral Health reviewed the screen Questions were added about loss Pediatric Integrated Care Collaborative (PICC)
One Small Test of Change So What? First PDSA is just the first step Small so that it can be tested quickly, but Small test does not equal small change Goal is to apply learnings and continue to make tests bigger and broader Sweep in more people as you go – moving toward implementation as you continue to learn and refine tools/develop processes Pediatric Integrated Care Collaborative (PICC)
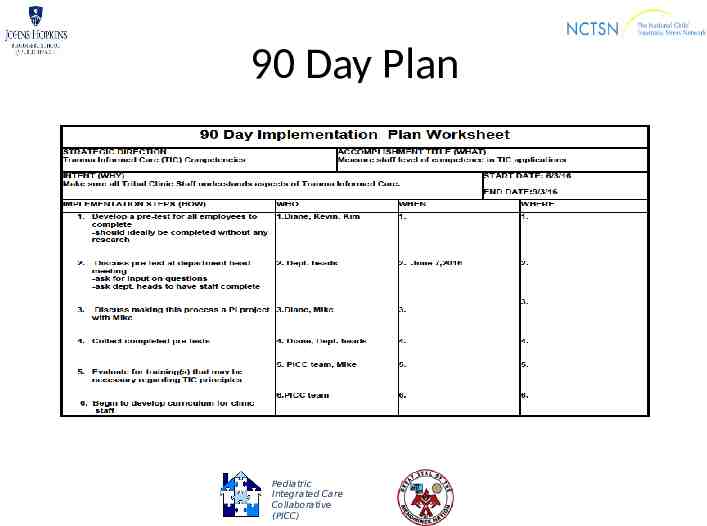
90 Day Plan Pediatric Integrated Care Collaborative (PICC)
Small Test of Change CHECKLIST Is intended to be an actual long-term change -- making something different Can be accomplished quickly No over-planning (Plan only as much as you can do) Consensus not required Adapt known results and tools Base on learning from prior cycle Is replicable and sustainable Pediatric Integrated Care Collaborative (PICC)
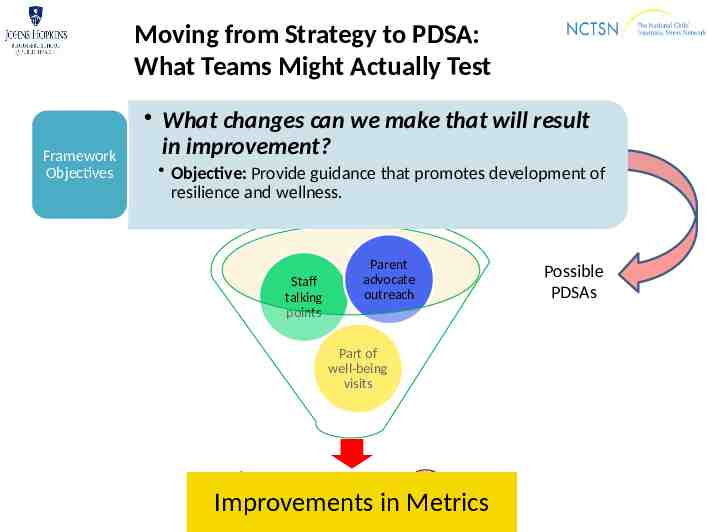
Moving from Strategy to PDSA: What Teams Might Actually Test Framework Objectives What changes can we make that will result in improvement? Objective: Provide guidance that promotes development of resilience and wellness. Parent advocate outreach Staff talking points Part of well-being visits Pediatric Integrated Care Collaborative (PICC) Improvements in Metrics Possible PDSAs
One More Note on Small Tests of Change Not just about changing things Not just about doing something small Not just about doing things quickly All about replicable and sustainable implementation Pediatric Integrated Care Collaborative (PICC)

Self-Reflection & Self-Care: Take a Moment Check in with yourself Laugh (Tell jokes) Breathe (Head outside) Create (Sketch) Stretch (Do some yoga) Nourish (Snacks, water, and coffee) Pediatric Integrated Care Collaborative (PICC)
Action Planning Jen Agosti Pediatric Integrated Care Collaborative (PICC)
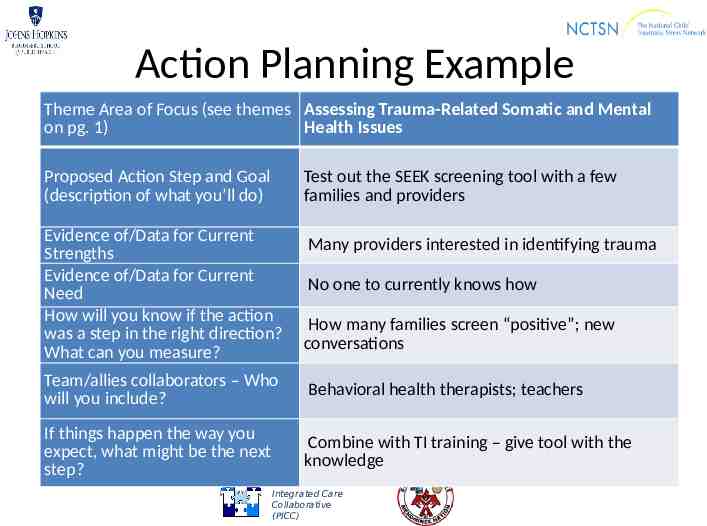
Action Planning Example Theme Area of Focus (see themes Assessing Trauma-Related Somatic and Mental on pg. 1) Health Issues Proposed Action Step and Goal (description of what you’ll do) Test out the SEEK screening tool with a few families and providers Evidence of/Data for Current Strengths Evidence of/Data for Current Need How will you know if the action was a step in the right direction? What can you measure? Many providers interested in identifying trauma No one to currently knows how How many families screen “positive”; new conversations Team/allies collaborators – Who will you include? Behavioral health therapists; teachers If things happen the way you expect, what might be the next step? Combine with TI training – give tool with the knowledge Pediatric Integrated Care Collaborative (PICC)

Small Group Sharing Pediatric Integrated Care Collaborative (PICC)

Small Group Discussions Learn and get ideas from others Objective Activities Share some identified challenges and successes Share possible solutions Identify data that could be used to help you know if you’re making progress Pediatric Integrated Care Collaborative (PICC)
Large Group Sharing/Reflections Jen Agosti and Maegan Rides At The Door Pediatric Integrated Care Collaborative (PICC)
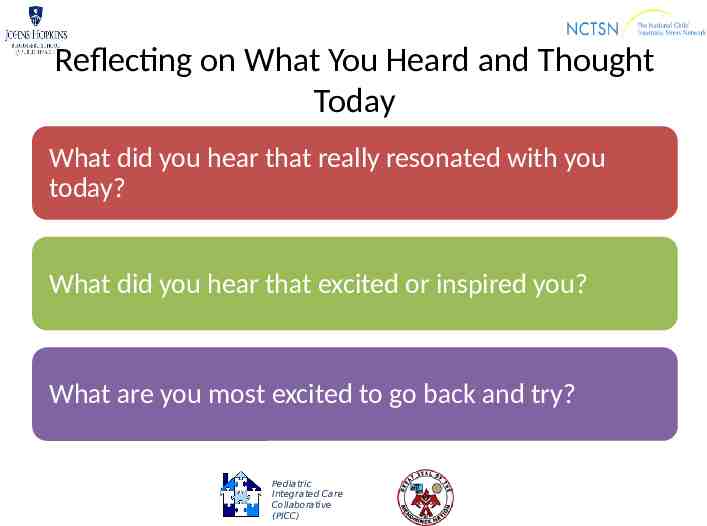
Reflecting on What You Heard and Thought Today What did you hear that really resonated with you today? What did you hear that excited or inspired you? What are you most excited to go back and try? Pediatric Integrated Care Collaborative (PICC)
THANK YOU! Pediatric Integrated Care Collaborative (PICC)