Workflow mapping: a tool for achieving meaningful use Center for
32 Slides513.22 KB
Workflow mapping: a tool for achieving meaningful use Center for Excellence in Primary Care UCSF Department of Family and Community Medicine Tom Bodenheimer, MD
Goals Explain workflow mapping Discuss why workflow mapping is useful prior to and after EHR implementation Demonstrate how to create workflow maps Review some meaningful use workflow examples
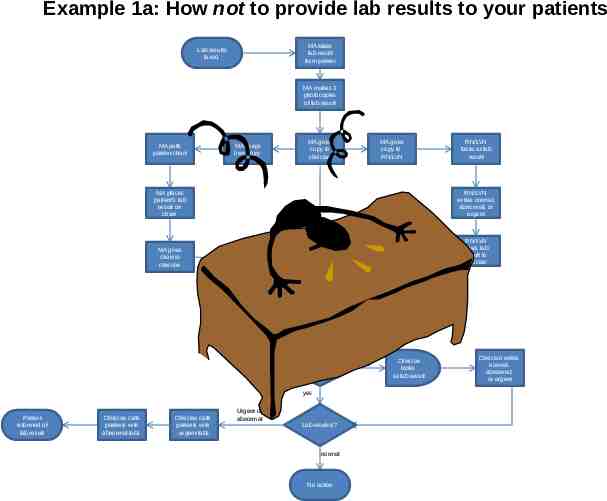
Example 1a: How not to provide lab results to your patients MA takes lab result from printer Lab results faxed MA makes 3 photocopies of lab result MA pulls patient chart MA keeps own copy MA gives copy to clinician MA gives copy to RN/LVN MA places patient’s lab result on chart RN/LVN looks at lab result RN/LVN writes normal, abnormal, or urgent MA gives chart to clinician RN/LVN gives lab result to clinician Clinician receives all 3 copies of lab result Clinician sorts lab results by patient Did RN/LVN write on lab result? yes Patient informed of lab result Clinician calls patients with abnormal labs Clinician calls patients with urgent labs Urgent or abnormal Lab result is? normal No action no Clinician looks at lab result Clinician writes normal, abnormal, or urgent
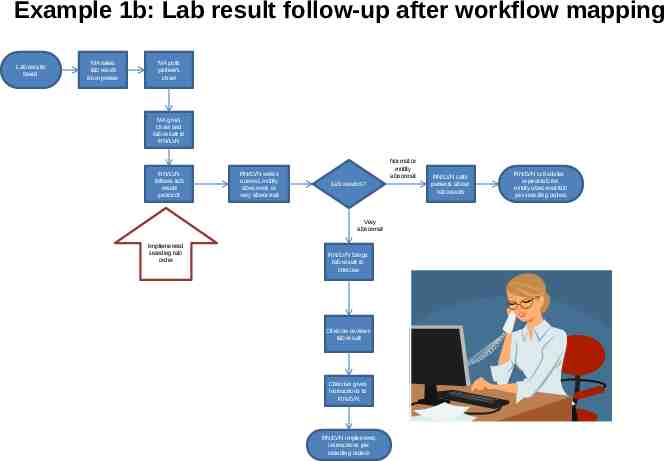
Example 1b: Lab result follow-up after workflow mapping Lab results faxed MA takes lab result from printer MA pulls patient’s chart MA gives chart and lab result to RN/LVN RN/LVN follows lab result protocol RN/LVN writes normal, mildly abnormal, or very abnormal Normal or mildly abnormal Lab result is? Very abnormal Implemented standing lab order RN/LVN brings lab result to clinician Clinician reviews lab result Clinician gives instructions to RN/LVN RN/LVN implements instructions per standing orders RN/LVN calls patients about lab results RN/LVN schedules repeat lab for mildly abnormal lab per standing orders
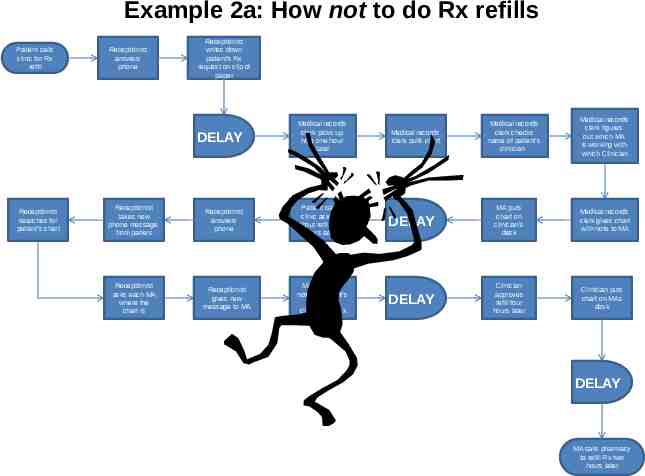
Example 2a: How not to do Rx refills Patient calls clinic for Rx refill Receptionist answers phone Receptionist writes down patient’s Rx request on slip of paper DELAY Receptionist searches for patient’s chart Receptionist takes new phone message from patient Receptionist asks each MA where the chart is Medical records clerk picks up note one hour later Receptionist answers phone Patient calls clinic asking about refill two hours later Receptionist gives new message to MA MA clips new note on patient’s chart on clinician’s desk Medical records clerk pulls chart Medical records clerk checks name of patient’s clinician Medical records clerk figures out which MA is working with which Clinician DELAY MA puts chart on clinician’s desk Medical records clerk gives chart with note to MA DELAY Clinician approves refill four hours later Clinician puts chart on MAs desk DELAY MA calls pharmacy to refill Rx two hours later
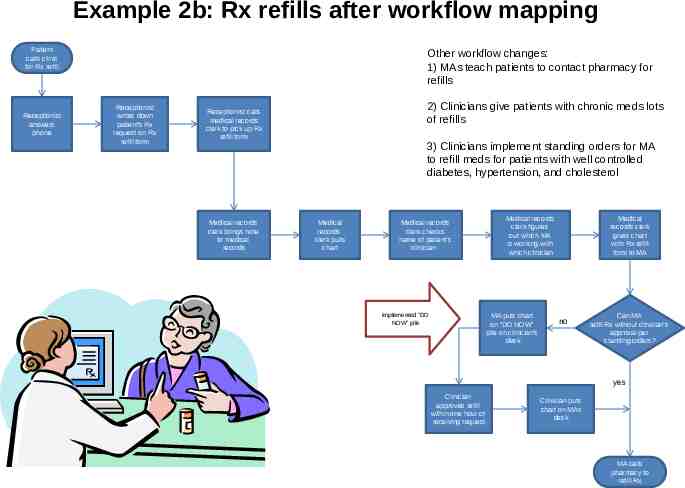
Example 2b: Rx refills after workflow mapping Patient calls clinic for Rx refill Receptionist answers phone Other workflow changes: 1) MAs teach patients to contact pharmacy for refills Receptionist writes down patient’s Rx request on Rx refill form 2) Clinicians give patients with chronic meds lots of refills Receptionist calls medical records clerk to pick up Rx refill form Medical records clerk brings note to medical records 3) Clinicians implement standing orders for MA to refill meds for patients with well controlled diabetes, hypertension, and cholesterol Medical records clerk pulls chart Medical records clerk checks name of patient’s clinician Medical records clerk figures out which MA is working with which clinician MA puts chart on “DO NOW” pile on clinician’s desk implemented “DO NOW” pile Medical records clerk gives chart with Rx refill form to MA no Can MA refill Rx without clinician’s approval per standing orders? yes Clinician approves refill within one hour of receiving request Clinician puts chart on MAs desk MA calls pharmacy to refill Rx
What is a workflow map? A visual representation of a process – A process is a series of actions, steps, or tasks performed in a certain order to achieve a certain result Defines the beginning of a process, the end of a process, and all the steps in-between Defines who does what in the process A measurement of what IS
Workflows before implementing EHR are different from those after Practice Manager EHR adoption Practice Manager
Workflow mapping pre-EHR reveals inefficiencies and waste Workflow mapping helps practices – Identify inefficiencies, waste, and dangers – Eliminate wasteful steps – Streamline complicated workflows – Standardize how work is done Example 1 (lab results): workflow mapping uncovered unnecessary steps that could easily be eliminated, making life easier for physicians and staff Example 2 (rx refills): workflow mapping showed that big changes were needed to eliminate waste and reduce patient delays
Workflow mapping pre-EHR: Tailor EHR to meet practice needs Mapping out processes before EHR implementation helps practices decide how to use the EHR Workflow mapping demonstrates what protocols and standing orders are needed to redistribute work Workflow maps help practices work with their EHR vendor so that the vendor understands how each person will use the EHR Examples 1 and 2: protocols and standing orders written pre-EHR adoption delineate who does what, which facilitates implementation of the EHR
Workflow mapping post-EHR: EHR is a huge change Going from paper to EHR changes every single thing in a practice Roles will change – What will medical records clerks do? – Medical assistants will enter vital signs electronically and provide more services in the rooming process – Clinicians will type progress notes and use templates – E-prescribing often shifts all refill work to Clinicians’ inboxes Example 2 (rx refill): Post-EHR workflow can be set up so that Clinicians do not handle every refill. This depends on pre-EHR workflow redesign
Workflows post-EHR: shows practices how best to use EHR EHR implementation tends to push work back onto the Clinician. Workflow mapping can prevent this Workflow mapping helps staff look at entire process and think how their work fits into a larger system Workflow maps help practices decide which personnel they need post-EHR Example 1 (lab results): If a practice does not have a RN or LVN, Clinicians need to review all labs. If the practice wants to delegate lab review to another team member, the practice would need a RN or LVN because MAs cannot review labs. Also, the practice will not need a medical records person.
Who’s involved with workflow mapping? One designated person – Oversees the team and keeps tasks on track – Understands all aspects of the process in detail – Drafts the initial workflow map The team – Decides what processes to map – Everyone involved in a workflow should be part of the mapping process – Discusses accuracy of the workflow map after it’s been drafted – Perfects the process and maps it out
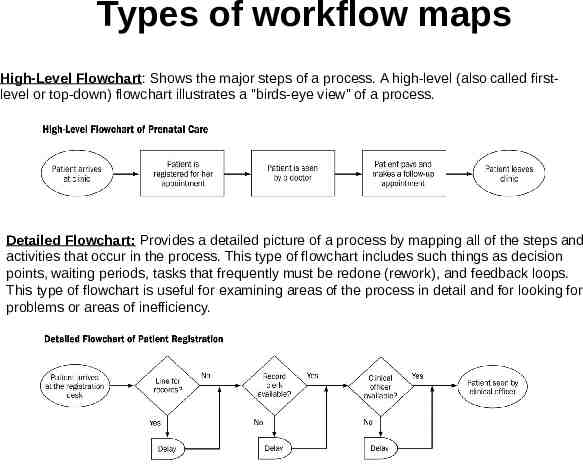
Types of workflow maps High-Level Flowchart: Shows the major steps of a process. A high-level (also called firstlevel or top-down) flowchart illustrates a "birds-eye view" of a process. Detailed Flowchart: Provides a detailed picture of a process by mapping all of the steps and activities that occur in the process. This type of flowchart includes such things as decision points, waiting periods, tasks that frequently must be redone (rework), and feedback loops. This type of flowchart is useful for examining areas of the process in detail and for looking for problems or areas of inefficiency.
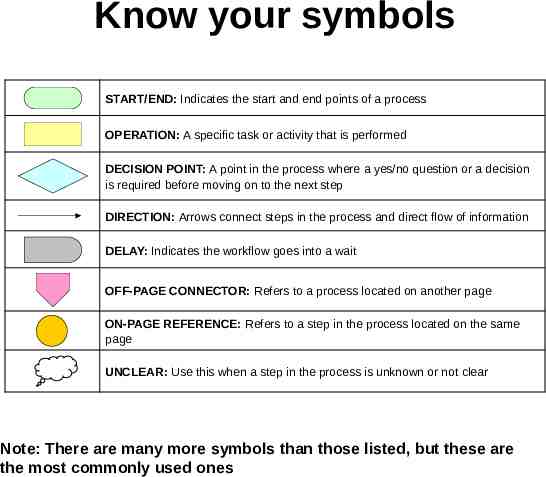
Know your symbols START/END: Indicates the start and end points of a process OPERATION: A specific task or activity that is performed DECISION POINT: A point in the process where a yes/no question or a decision is required before moving on to the next step DIRECTION: Arrows connect steps in the process and direct flow of information DELAY: Indicates the workflow goes into a wait OFF-PAGE CONNECTOR: Refers to a process located on another page ON-PAGE REFERENCE: Refers to a step in the process located on the same page UNCLEAR: Use this when a step in the process is unknown or not clear Note: There are many more symbols than those listed, but these are the most commonly used ones
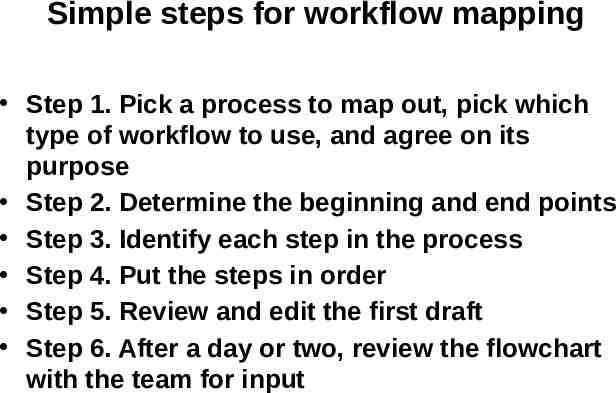
Simple steps for workflow mapping Step 1. Pick a process to map out, pick which type of workflow to use, and agree on its purpose Step 2. Determine the beginning and end points Step 3. Identify each step in the process Step 4. Put the steps in order Step 5. Review and edit the first draft Step 6. After a day or two, review the flowchart with the team for input
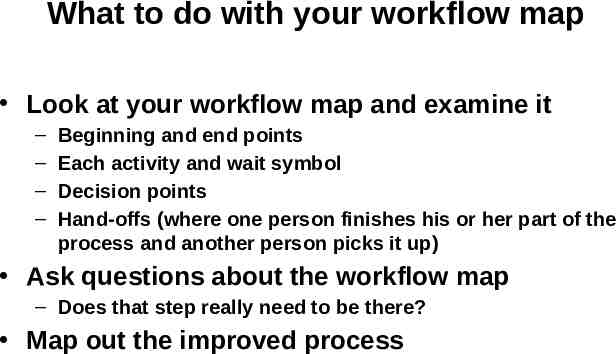
What to do with your workflow map Look at your workflow map and examine it – – – – Beginning and end points Each activity and wait symbol Decision points Hand-offs (where one person finishes his or her part of the process and another person picks it up) Ask questions about the workflow map – Does that step really need to be there? Map out the improved process
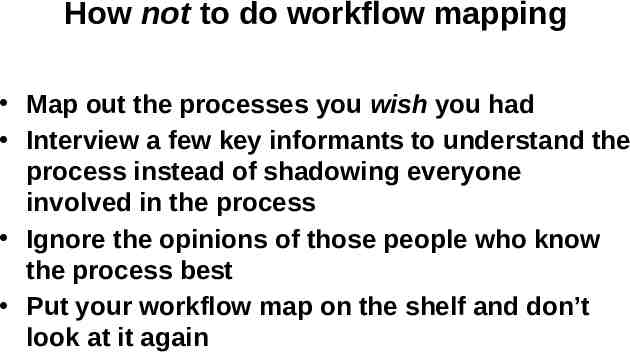
How not to do workflow mapping Map out the processes you wish you had Interview a few key informants to understand the process instead of shadowing everyone involved in the process Ignore the opinions of those people who know the process best Put your workflow map on the shelf and don’t look at it again
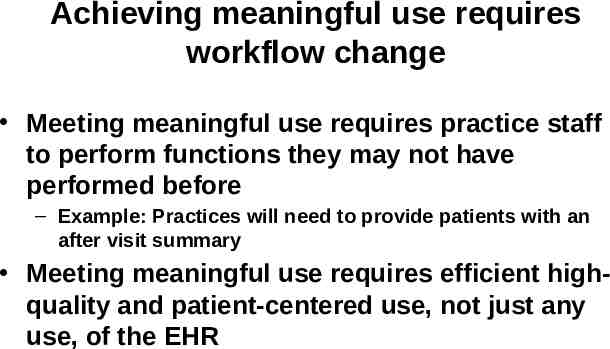
Achieving meaningful use requires workflow change Meeting meaningful use requires practice staff to perform functions they may not have performed before – Example: Practices will need to provide patients with an after visit summary Meeting meaningful use requires efficient highquality and patient-centered use, not just any use, of the EHR
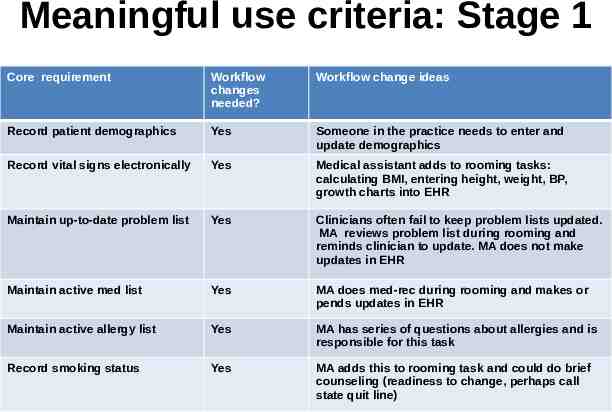
Meaningful use criteria: Stage 1 Core requirement Workflow changes needed? Workflow change ideas Record patient demographics Yes Someone in the practice needs to enter and update demographics Record vital signs electronically Yes Medical assistant adds to rooming tasks: calculating BMI, entering height, weight, BP, growth charts into EHR Maintain up-to-date problem list Yes Clinicians often fail to keep problem lists updated. MA reviews problem list during rooming and reminds clinician to update. MA does not make updates in EHR Maintain active med list Yes MA does med-rec during rooming and makes or pends updates in EHR Maintain active allergy list Yes MA has series of questions about allergies and is responsible for this task Record smoking status Yes MA adds this to rooming task and could do brief counseling (readiness to change, perhaps call state quit line)
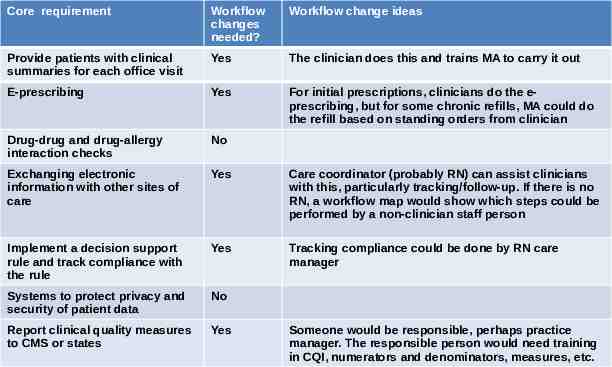
Core requirement Workflow changes needed? Workflow change ideas Provide patients with clinical summaries for each office visit Yes The clinician does this and trains MA to carry it out E-prescribing Yes For initial prescriptions, clinicians do the eprescribing, but for some chronic refills, MA could do the refill based on standing orders from clinician Drug-drug and drug-allergy interaction checks No Exchanging electronic information with other sites of care Yes Care coordinator (probably RN) can assist clinicians with this, particularly tracking/follow-up. If there is no RN, a workflow map would show which steps could be performed by a non-clinician staff person Implement a decision support rule and track compliance with the rule Yes Tracking compliance could be done by RN care manager Systems to protect privacy and security of patient data No Report clinical quality measures to CMS or states Yes Someone would be responsible, perhaps practice manager. The responsible person would need training in CQI, numerators and denominators, measures, etc.
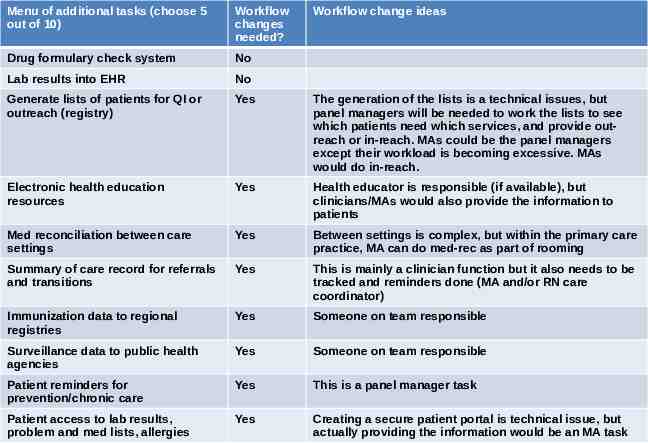
Menu of additional tasks (choose 5 out of 10) Workflow changes needed? Workflow change ideas Drug formulary check system No Lab results into EHR No Generate lists of patients for QI or outreach (registry) Yes The generation of the lists is a technical issues, but panel managers will be needed to work the lists to see which patients need which services, and provide outreach or in-reach. MAs could be the panel managers except their workload is becoming excessive. MAs would do in-reach. Electronic health education resources Yes Health educator is responsible (if available), but clinicians/MAs would also provide the information to patients Med reconciliation between care settings Yes Between settings is complex, but within the primary care practice, MA can do med-rec as part of rooming Summary of care record for referrals and transitions Yes This is mainly a clinician function but it also needs to be tracked and reminders done (MA and/or RN care coordinator) Immunization data to regional registries Yes Someone on team responsible Surveillance data to public health agencies Yes Someone on team responsible Patient reminders for prevention/chronic care Yes This is a panel manager task Patient access to lab results, problem and med lists, allergies Yes Creating a secure patient portal is technical issue, but actually providing the information would be an MA task
Suggested workflows for meaningful use The following workflow are examples How your practice works may be different Pilot the EHR workflows with one MA or one receptionist and one clinician and a couple of patients to see if they work
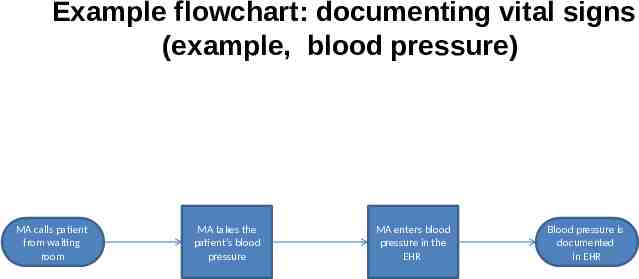
Example flowchart: documenting vital signs (example, blood pressure) MA calls patient from waiting room MA takes the patient’s blood pressure MA enters blood pressure in the EHR Blood pressure is documented in EHR
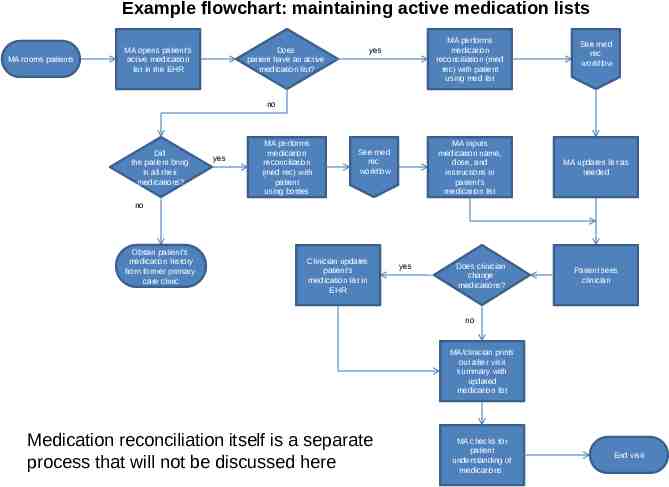
Example flowchart: maintaining active medication lists MA rooms patients MA opens patient’s active medication list in the EHR MA performs medication reconciliation (med rec) with patient using med list yes Does patient have an active medication list? See med rec workflow no Did the patient bring in all their medications? yes MA performs medication reconciliation (med rec) with patient using bottles MA inputs medication name, dose, and instructions in patient’s medication list yes See med rec workflow MA updates list as needed no Obtain patient’s medication history from former primary care clinic Clinician updates patient’s medication list in EHR yes Does clinician change medications? Patient sees clinician no MA/clinician prints out after visit summary with updated medication list Medication reconciliation itself is a separate process that will not be discussed here MA checks for patient understanding of medications End visit
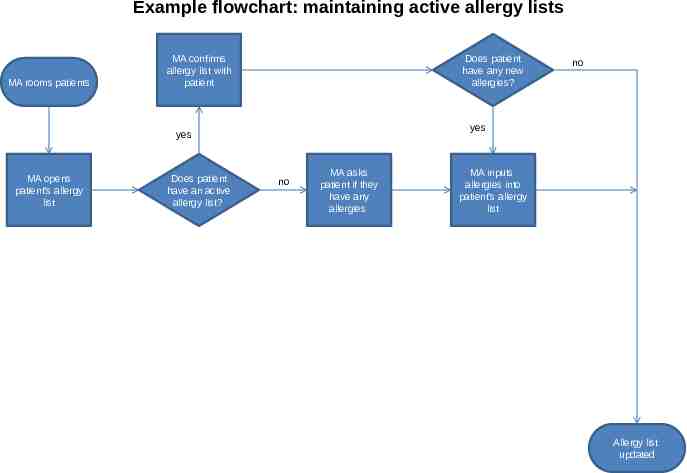
Example flowchart: maintaining active allergy lists MA rooms patients MA confirms allergy list with patient Does patient have any new allergies? yes yes MA opens patient’s allergy list Does patient have an active allergy list? no no MA asks patient if they have any allergies MA inputs allergies into patient’s allergy list Allergy list updated
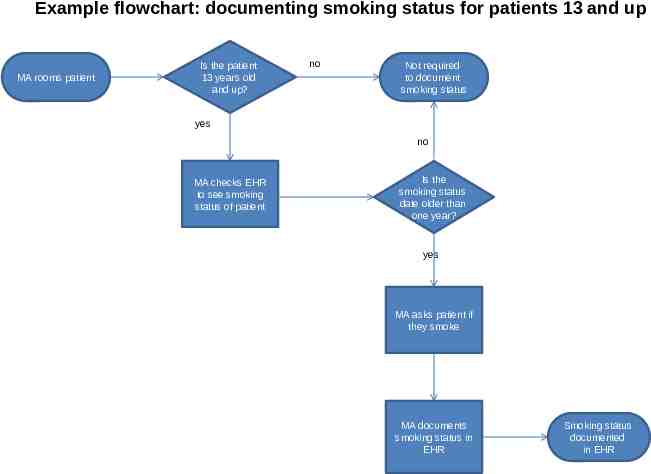
Example flowchart: documenting smoking status for patients 13 and up MA rooms patient Is the patient 13 years old and up? no Not required to document smoking status yes no MA checks EHR to see smoking status of patient Is the smoking status date older than one year? yes MA asks patient if they smoke MA documents smoking status in EHR Smoking status documented in EHR
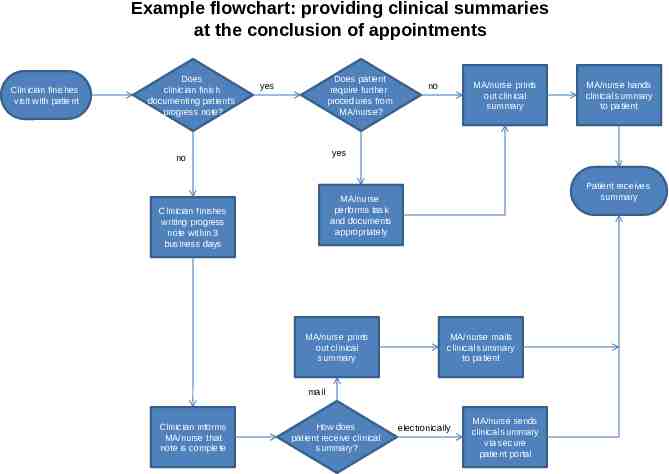
Example flowchart: providing clinical summaries at the conclusion of appointments Clinician finishes visit with patient Does clinician finish documenting patient’s progress note? Does patient require further procedures from MA/nurse? yes MA/nurse prints out clinical summary no yes no Patient receives summary MA/nurse performs task and documents appropriately Clinician finishes writing progress note within 3 business days MA/nurse prints out clinical summary MA/nurse mails clinical summary to patient mail Clinician informs MA/nurse that note is complete MA/nurse hands clinical summary to patient How does patient receive clinical summary? electronically MA/nurse sends clinical summary via secure patient portal
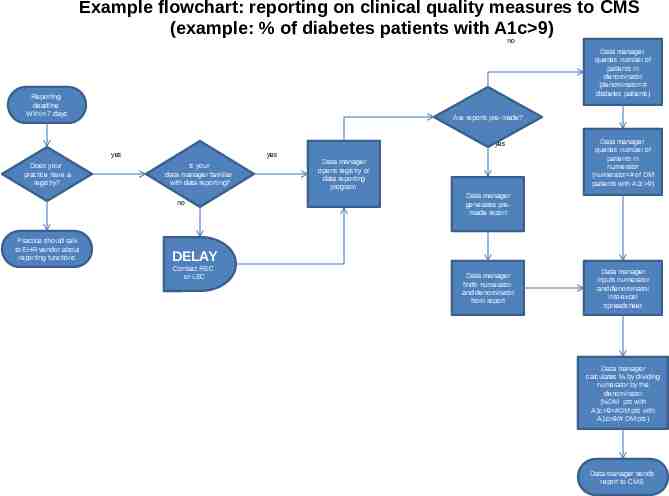
Example flowchart: reporting on clinical quality measures to CMS (example: % of diabetes patients with A1c 9) no Data manager queries number of patients in denominator (denominator # diabetes patients) Reporting deadline Within 7 days Are reports pre-made? yes yes Does your practice have a registry? yes Is your data manager familiar with data reporting? no Practice should talk to EHR vendor about reporting functions Data manager opens registry or data reporting program Data manager queries number of patients in numerator (numerator # of DM patients with A1c 9) Data manager generates premade report DELAY Contact REC or LEC Data manager finds numerator and denominator from report Data manager inputs numerator and denominator into excel spreadsheet Data manager calculates % by dividing numerator by the denominator (%DM pts with A1c 9 #DM pts with A1c 9/# DM pts) Data manager sends report to CMS
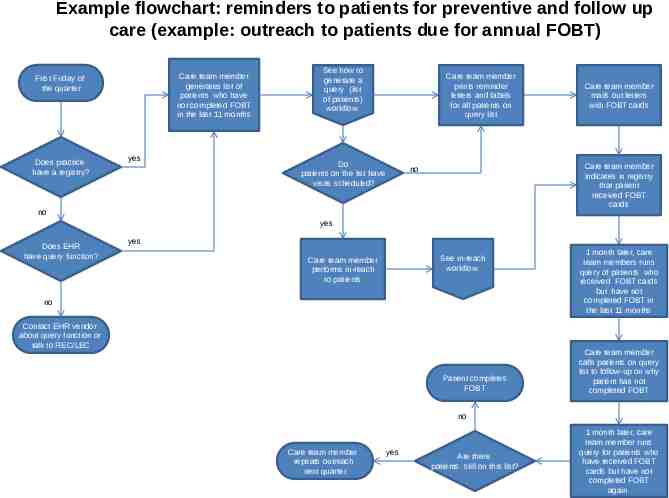
Example flowchart: reminders to patients for preventive and follow up care (example: outreach to patients due for annual FOBT) Care team member generates list of patients who have not completed FOBT in the last 11 months First Friday of the quarter Does practice have a registry? yes See how to generate a query (list of patients) workflow Care team member prints reminder letters and labels for all patients on query list Do patients on the list have visits scheduled? Care team member mails out letters with FOBT cards Care team member indicates in registry that patient received FOBT cards no no yes Does EHR have query function? yes See in-reach workflow Care team member performs in-reach to patients no Contact EHR vendor about query function or talk to REC/LEC Patient completes FOBT 1 month later, care team members runs query of patients who received FOBT cards but have not completed FOBT in the last 11 months Care team member calls patients on query list to follow-up on why patient has not completed FOBT no Care team member repeats outreach next quarter yes Are there patients still on this list? 1 month later, care team member runs query for patients who have received FOBT cards but have not completed FOBT again
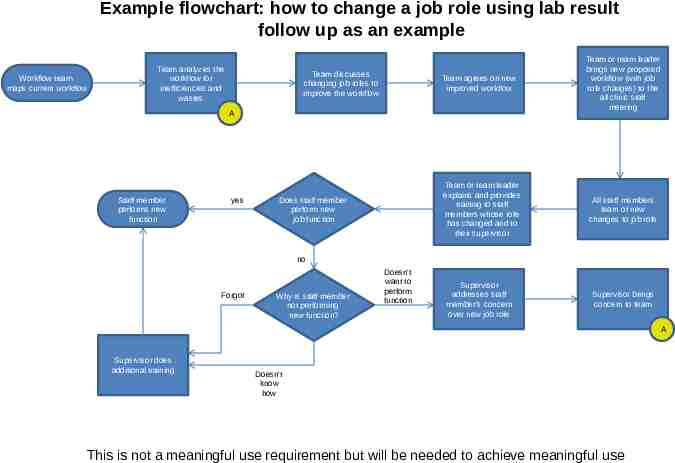
Example flowchart: how to change a job role using lab result follow up as an example Workflow team maps current workflow Team analyzes the workflow for inefficiencies and wastes Team discusses changing job roles to improve the workflow Team agrees on new improved workflow A Staff member performs new function yes Team or team leader explains and provides training to staff members whose role has changed and to their supervisor Does staff member perform new job function Team or team leader brings new proposed workflow (with job role changes) to the all clinic staff meeting All staff members learn of new changes to job role no Forgot Why is staff member not performing new function? Doesn’t want to perform function Supervisor addresses staff member’s concern over new job role Supervisor brings concern to team A Supervisor does additional training Doesn’t know how This is not a meaningful use requirement but will be needed to achieve meaningful use
Conclusion Workflow mapping is a great tool to help implement EHR and achieve meaningful use EHR adoption does not equal meaningful use Workflow maps are a tool to improve care for patients, improve efficiency in practice, and redistribute work and job roles