Tuberculosis: management, control and prevention Developed by: In
50 Slides3.14 MB
Tuberculosis: management, control and prevention Developed by: In partnership with:
The Truth About TB is a national programme that raises public and professional awareness of tuberculosis. This training resource has been developed by TB Alert, the national tuberculosis charity, in partnership with NHS England and Public Health England. www.thetruthabouttb.org
Aims and objectives Aim: to recognise how TB presents and to enhance early diagnosis and treatment through prompt referral to TB Specialist Services. Objectives: To provide an overview of the identification, prevention and treatment of Tuberculosis (TB) in your area of clinical practice. risk factors early diagnosis the impact of delay in diagnosis treatment of TB LTBI testing and treatment role of TB Specialist Services. www.thetruthabouttb.org
What is tuberculosis? TB is a bacillus, meaning rod shaped bacteria; it is from the genus mycobacteria. TB most usually affects the lungs but it can affect other parts of the body. Only TB of the lungs or throat is infectious. TB is an airborne disease which can be cured. TB is transmitted to others when a person with infectious TB coughs, talks, sings, laughs or sneezes. TB is a notifiable disease under Public Health (Control of Disease) Act 1984. TB incidence is decreasing globally, and has decreased in the UK since 2011. www.thetruthabouttb.org
Epidemiology of TB www.thetruthabouttb.org
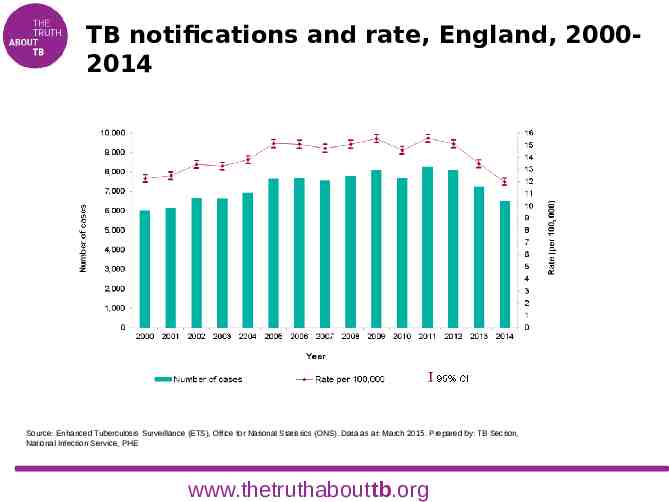
TB notifications and rate, England, 20002014 Source: Enhanced Tuberculosis Surveillance (ETS), Office for National Statistics (ONS). Data as at: March 2015. Prepared by: TB Section, National Infection Service, PHE www.thetruthabouttb.org
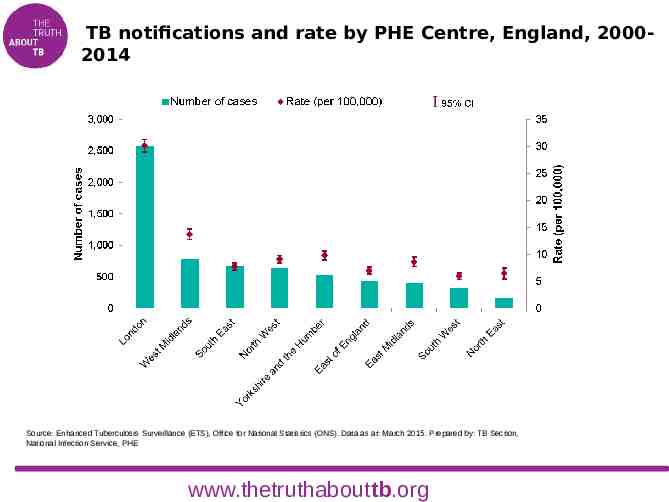
TB notifications and rate by PHE Centre, England, 20002014 Source: Enhanced Tuberculosis Surveillance (ETS), Office for National Statistics (ONS). Data as at: March 2015. Prepared by: TB Section, National Infection Service, PHE www.thetruthabouttb.org
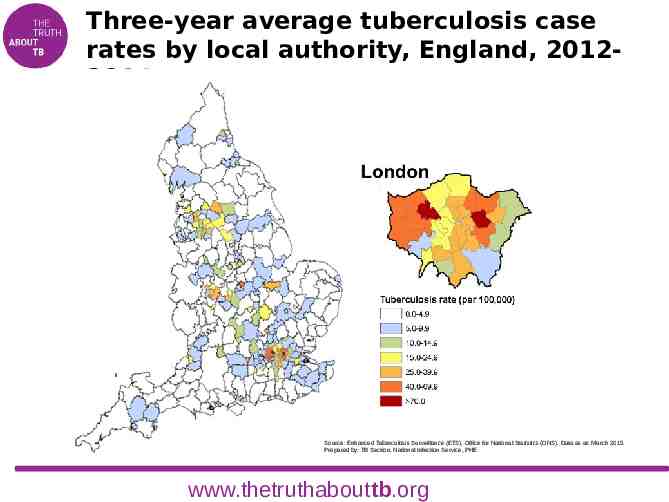
Three-year average tuberculosis case rates by local authority, England, 20122014 Source: Enhanced Tuberculosis Surveillance (ETS), Office for National Statistics (ONS). Data as at: March 2015. Prepared by: TB Section, National Infection Service, PHE www.thetruthabouttb.org
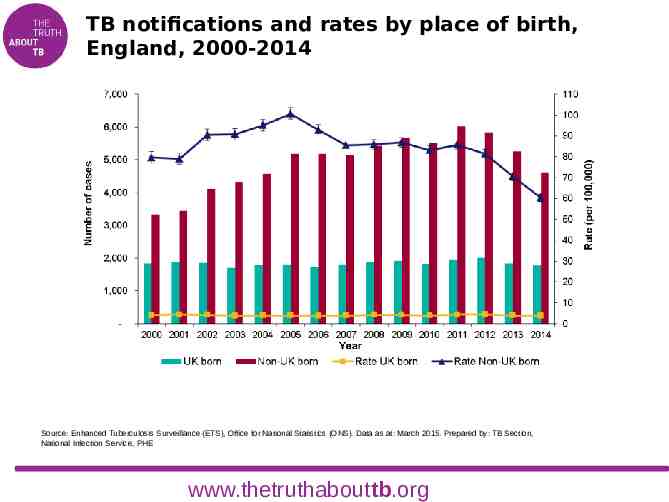
TB notifications and rates by place of birth, England, 2000-2014 Source: Enhanced Tuberculosis Surveillance (ETS), Office for National Statistics (ONS). Data as at: March 2015. Prepared by: TB Section, National Infection Service, PHE www.thetruthabouttb.org
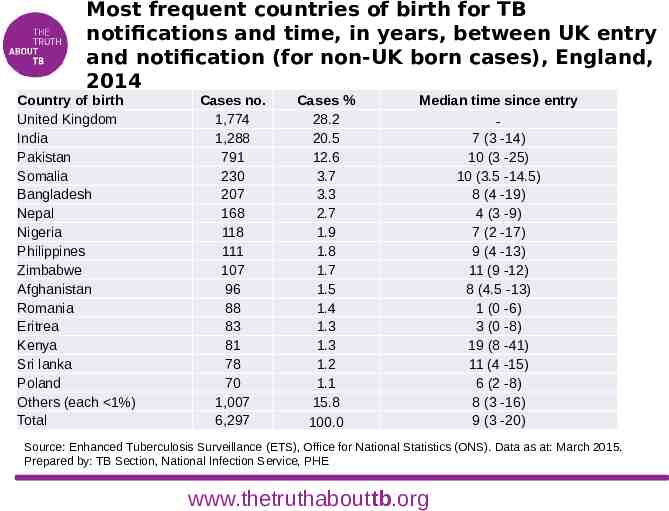
Most frequent countries of birth for TB notifications and time, in years, between UK entry and notification (for non-UK born cases), England, 2014 Country of birth United Kingdom India Pakistan Somalia Bangladesh Nepal Nigeria Philippines Zimbabwe Afghanistan Romania Eritrea Kenya Sri lanka Poland Others (each 1%) Total Cases no. 1,774 1,288 791 230 207 168 118 111 107 96 88 83 81 78 70 1,007 6,297 Cases % 28.2 20.5 12.6 3.7 3.3 2.7 1.9 1.8 1.7 1.5 1.4 1.3 1.3 1.2 1.1 15.8 100.0 Median time since entry 7 (3 -14) 10 (3 -25) 10 (3.5 -14.5) 8 (4 -19) 4 (3 -9) 7 (2 -17) 9 (4 -13) 11 (9 -12) 8 (4.5 -13) 1 (0 -6) 3 (0 -8) 19 (8 -41) 11 (4 -15) 6 (2 -8) 8 (3 -16) 9 (3 -20) Source: Enhanced Tuberculosis Surveillance (ETS), Office for National Statistics (ONS). Data as at: March 2015. Prepared by: TB Section, National Infection Service, PHE www.thetruthabouttb.org

Local epidemiology 2013 Total notifications Incidence (n/100,000) UK born (%) Non-UK born (%) Pulmonary disease Extra-pulmonary disease www.thetruthabouttb.org 2014

Local epidemiology ADD a local map showing the local burden of TB – possibly by LSOA (available from PHE’s Field Epidemiology Service) www.thetruthabouttb.org
Aetiology, pathogenesis and transmission of TB www.thetruthabouttb.org

Droplet nuclei containing TB bacilli are inhaled, enter the lungs, and travel to the alveoli. TB bacilli multiply in the alveoli. www.thetruthabouttb.org

A small number of TB bacilli enter the bloodstream and spread throughout the body. The bacilli may reach any part of the body. Within 2-10 weeks, the immune system produces immune cells called macrophages that surround the TB bacilli. The cells form a hard shell called a granuloma that keeps the bacilli contained and under control (latent TB infection). www.thetruthabouttb.org
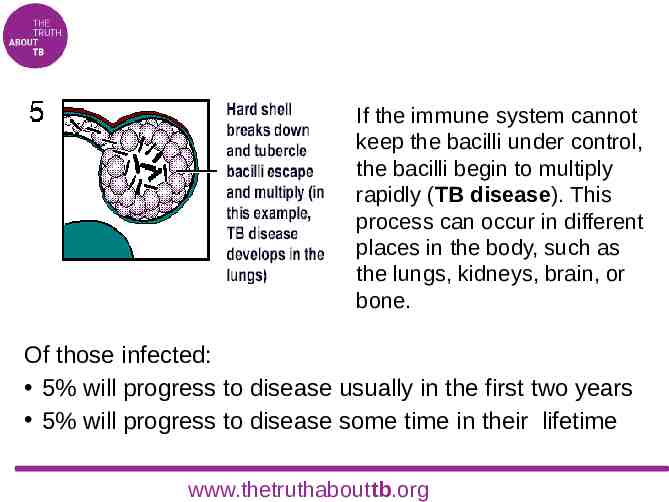
If the immune system cannot keep the bacilli under control, the bacilli begin to multiply rapidly (TB disease). This process can occur in different places in the body, such as the lungs, kidneys, brain, or bone. Of those infected: 5% will progress to disease usually in the first two years 5% will progress to disease some time in their lifetime www.thetruthabouttb.org
Risk factors for TB www.thetruthabouttb.org
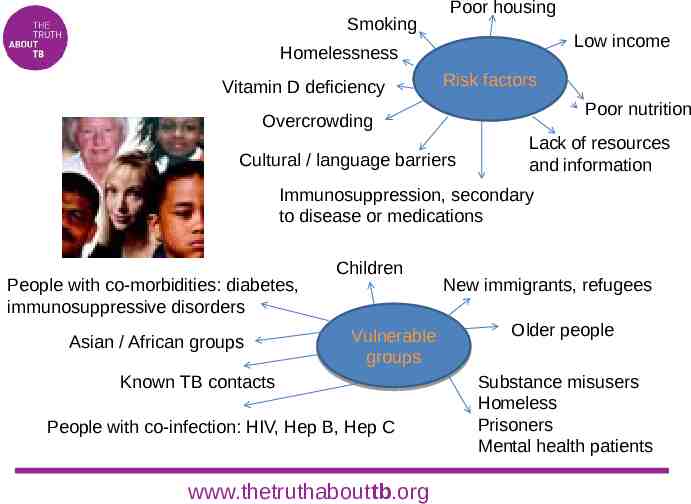
Smoking Poor housing Low income Homelessness Vitamin D deficiency Risk factors Poor nutrition Overcrowding Cultural / language barriers Lack of resources and information Immunosuppression, secondary to disease or medications People with co-morbidities: diabetes, immunosuppressive disorders Asian / African groups Children Vulnerable groups Known TB contacts People with co-infection: HIV, Hep B, Hep C www.thetruthabouttb.org New immigrants, refugees Older people Substance misusers Homeless Prisoners Mental health patients
Stigma and TB The risk factors associated with TB are factors that can themselves create stigma. A caring, respectful attitude is essential Stigma can: prevent people seeking help lead to denial once diagnosed deter people from attending appointments or taking treatment make contact tracing difficult. www.thetruthabouttb.org
Diagnosis and treatment of active TB www.thetruthabouttb.org
Typical presentation of TB General symptoms: fever, night sweats, fatigue, anorexia, weight loss Pulmonary symptoms: cough, haemoptysis Extra pulmonary symptoms: localised pain and/or swelling, lymphadenopathy, wounds that won’t heal N.B. extra pulmonary TB can mimic other diseases/conditions www.thetruthabouttb.org Have a high level of suspicion
Think TB! If you see a patient who is unwell, tired, maybe losing weight, maybe feverish, perhaps with swollen lymph glands or a cough for three weeks or longer . . if they come from a high risk group . could it be TB? www.thetruthabouttb.org
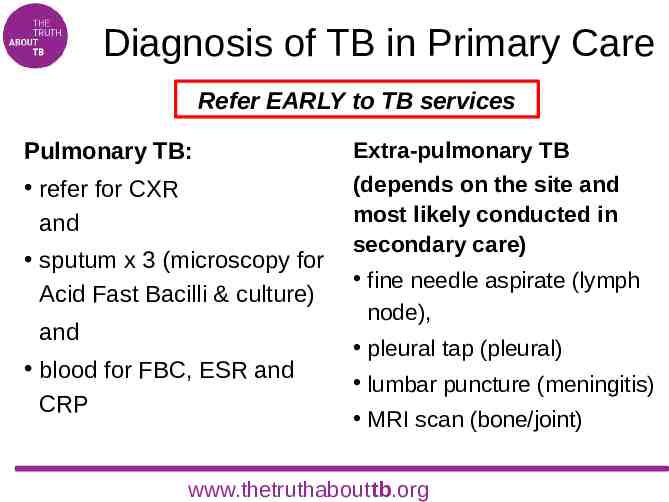
Diagnosis of TB in Primary Care Refer EARLY to TB services Pulmonary TB: Extra-pulmonary TB refer for CXR and (depends on the site and most likely conducted in secondary care) sputum x 3 (microscopy for Acid Fast Bacilli & culture) and blood for FBC, ESR and CRP fine needle aspirate (lymph node), pleural tap (pleural) lumbar puncture (meningitis) MRI scan (bone/joint) www.thetruthabouttb.org
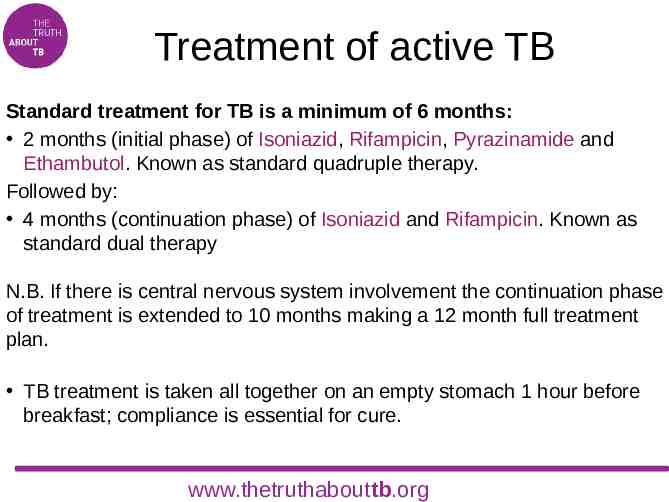
Treatment of active TB Standard treatment for TB is a minimum of 6 months: 2 months (initial phase) of Isoniazid, Rifampicin, Pyrazinamide and Ethambutol. Known as standard quadruple therapy. Followed by: 4 months (continuation phase) of Isoniazid and Rifampicin. Known as standard dual therapy N.B. If there is central nervous system involvement the continuation phase of treatment is extended to 10 months making a 12 month full treatment plan. TB treatment is taken all together on an empty stomach 1 hour before breakfast; compliance is essential for cure. www.thetruthabouttb.org

Main treatment side effects Isoniazid: fever, peripheral neuropathy and optic neuritis Pyrazinamide: use with caution in patients with gout Rifampicin: reddish colour to the urine Ethambutol: peripheral neuropathy, optic neuropathy and gout Generally – hepatotoxcity, nausea and skin rashes www.thetruthabouttb.org
Directly observed treatment Directly observed treatment is known as DOT. Each DOT case is assessed by the TB specialist team regarding the patient’s ability to adhere to the six-month treatment regimen. DOT is initiated for those at risk of being unable to adhere to treatment. A professional case worker, person trained to be a DOT observer, or a trusted family member or friend will watch the patient take their TB treatment. Primary care providers, such as GP practices or pharmacists, may be asked to provide DOT. www.thetruthabouttb.org
Diagnosis and treatment of latent TB infection (LTBI) www.thetruthabouttb.org
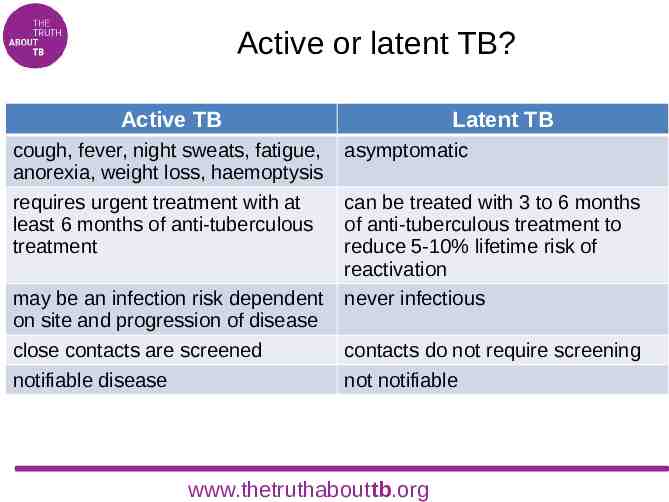
Active or latent TB? Active TB cough, fever, night sweats, fatigue, anorexia, weight loss, haemoptysis requires urgent treatment with at least 6 months of anti-tuberculous treatment may be an infection risk dependent on site and progression of disease close contacts are screened notifiable disease Latent TB asymptomatic can be treated with 3 to 6 months of anti-tuberculous treatment to reduce 5-10% lifetime risk of reactivation never infectious contacts do not require screening not notifiable www.thetruthabouttb.org
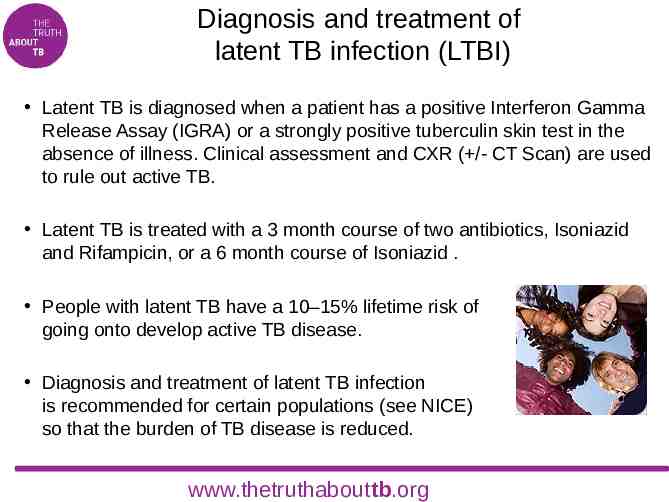
Diagnosis and treatment of latent TB infection (LTBI) Latent TB is diagnosed when a patient has a positive Interferon Gamma Release Assay (IGRA) or a strongly positive tuberculin skin test in the absence of illness. Clinical assessment and CXR ( /- CT Scan) are used to rule out active TB. Latent TB is treated with a 3 month course of two antibiotics, Isoniazid and Rifampicin, or a 6 month course of Isoniazid . People with latent TB have a 10–15% lifetime risk of going onto develop active TB disease. Diagnosis and treatment of latent TB infection is recommended for certain populations (see NICE) so that the burden of TB disease is reduced. www.thetruthabouttb.org
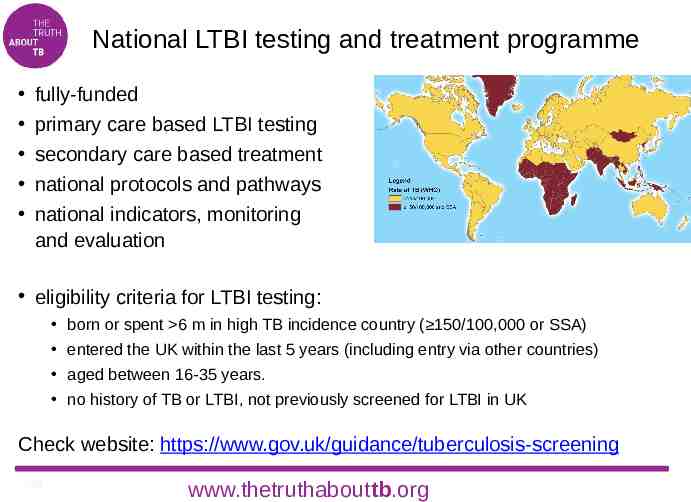
National LTBI testing and treatment programme fully-funded primary care based LTBI testing secondary care based treatment national protocols and pathways national indicators, monitoring and evaluation eligibility criteria for LTBI testing: born or spent 6 m in high TB incidence country ( 150/100,000 or SSA) entered the UK within the last 5 years (including entry via other countries) aged between 16-35 years. no history of TB or LTBI, not previously screened for LTBI in UK Check website: https://www.gov.uk/guidance/tuberculosis-screening 30 www.thetruthabouttb.org
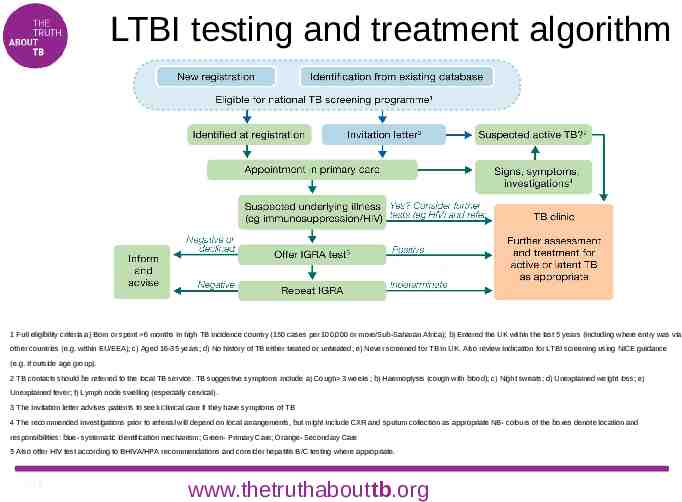
LTBI testing and treatment algorithm Latent Tuberculosis Infection (LTBI) testing and treatment algorithm 1 Full eligibility criteria a) Born or spent 6 months in high TB incidence country (150 cases per 100,000 or more/Sub-Saharan Africa); b) Entered the UK within the last 5 years (including where entry was via other countries (e.g. within EU/EEA); c) Aged 16-35 years; d) No history of TB either treated or untreated; e) Never screened for TB in UK. Also review indication for LTBI screening using NICE guidance (e.g. if outside age group). 2 TB contacts should be referred to the local TB service. TB suggestive symptoms include a) Cough 3 weeks; b) Haemoptysis (cough with blood); c) Night sweats; d) Unexplained weight loss; e) Unexplained fever; f) Lymph node swelling (especially cervical). 3 The invitation letter advises patients to seek clinical care if they have symptoms of TB 4 The recommended investigations prior to referral will depend on local arrangements, but might include CXR and sputum collection as appropriate NB- colours of the boxes denote location and responsibilities: blue- systematic identification mechanism; Green- Primary Care; Orange- Secondary Care 5 Also offer HIV test according to BHIVA/HPA recommendations and consider hepatitis B/C testing where appropriate. 31 www.thetruthabouttb.org
Control and prevention of TB www.thetruthabouttb.org
The TB Strategy for England Launched in 2015 Aims to achieve a year-on-year decrease in TB incidence, a reduction in health inequalities and, ultimately, the elimination of TB as a public health problem Strategy lists 10 key ‘areas for action’: improving access and early diagnosis high quality diagnostics high quality treatment and care services contact tracing vaccination tackling drug resistance tackling TB in under-served populations new entrant screening for LTBI effective surveillance and monitoring workforce strategy. www.gov.uk/government/publications/collaborative-tuberculosis-strategy-for-england 33 www.thetruthabouttb.org
Contact tracing Contact tracing is usually carried out by TB nurses. Results aid understanding of how infectious the TB index case is – this can inform further public health actions. TB transmission most often occurs among household contacts. Contact tracing is important because: 1% of contacts screened have active TB 10% of contacts screened have latent TB infection 60% of child contacts under 2 years will go onto develop active TB. www.thetruthabouttb.org
Vaccination with BCG The aim of the UK BCG immunisation programme is to immunise those at increased risk of developing severe disease and/or those at increased risk of exposure to TB infection. www.thetruthabouttb.org
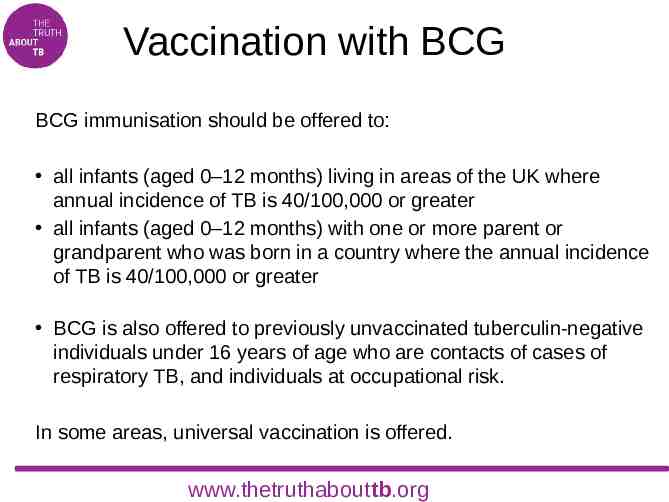
Vaccination with BCG BCG immunisation should be offered to: all infants (aged 0–12 months) living in areas of the UK where annual incidence of TB is 40/100,000 or greater all infants (aged 0–12 months) with one or more parent or grandparent who was born in a country where the annual incidence of TB is 40/100,000 or greater BCG is also offered to previously unvaccinated tuberculin-negative individuals under 16 years of age who are contacts of cases of respiratory TB, and individuals at occupational risk. In some areas, universal vaccination is offered. www.thetruthabouttb.org
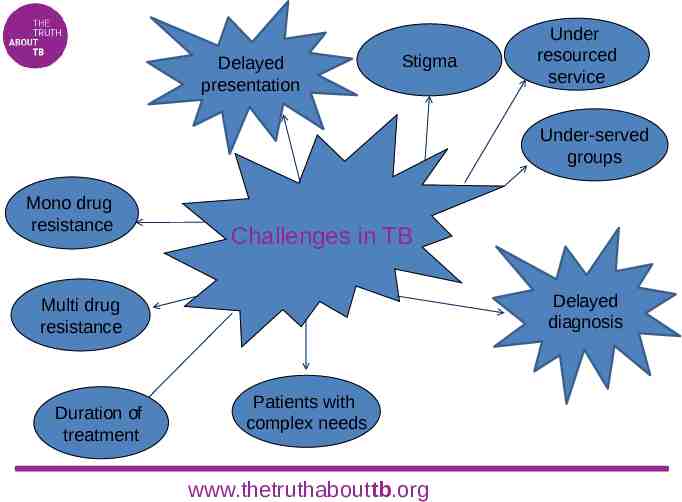
Delayed presentation Stigma Under resourced service Under-served groups Mono drug resistance Challenges in TB Delayed diagnosis Multi drug resistance Duration of treatment Patients with complex needs www.thetruthabouttb.org
TB Specialist Services and their role in TB control www.thetruthabouttb.org

TB Specialist Services The TB Specialist Team includes specialist TB physicians, microbiologists, TB specialist nurses, TB case workers, public health teams and, in London, the Find & Treat Team. The role of the team: investigation, diagnosis and treatment of suspected TB, active and latent co-ordination of care and support for patients on treatment for TB provision of support and advice to other services and the public notification and public health responsibilities contact tracing and screening for TB education and training. REFER EARLY www.thetruthabouttb.org
Local TB Services ADD details of local TB Services HERE www.thetruthabouttb.org
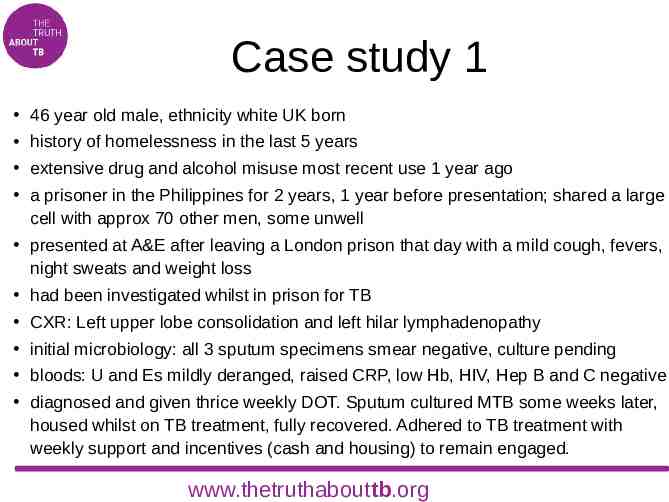
Case study 1 46 year old male, ethnicity white UK born history of homelessness in the last 5 years extensive drug and alcohol misuse most recent use 1 year ago a prisoner in the Philippines for 2 years, 1 year before presentation; shared a large cell with approx 70 other men, some unwell presented at A&E after leaving a London prison that day with a mild cough, fevers, night sweats and weight loss had been investigated whilst in prison for TB CXR: Left upper lobe consolidation and left hilar lymphadenopathy initial microbiology: all 3 sputum specimens smear negative, culture pending bloods: U and Es mildly deranged, raised CRP, low Hb, HIV, Hep B and C negative diagnosed and given thrice weekly DOT. Sputum cultured MTB some weeks later, housed whilst on TB treatment, fully recovered. Adhered to TB treatment with weekly support and incentives (cash and housing) to remain engaged. www.thetruthabouttb.org
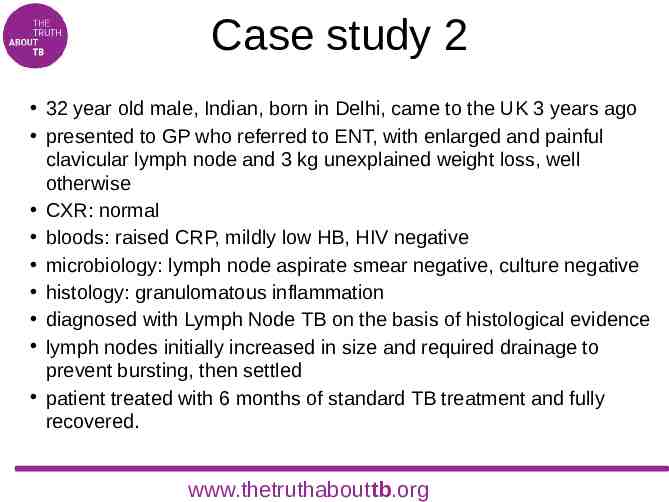
Case study 2 32 year old male, Indian, born in Delhi, came to the UK 3 years ago presented to GP who referred to ENT, with enlarged and painful clavicular lymph node and 3 kg unexplained weight loss, well otherwise CXR: normal bloods: raised CRP, mildly low HB, HIV negative microbiology: lymph node aspirate smear negative, culture negative histology: granulomatous inflammation diagnosed with Lymph Node TB on the basis of histological evidence lymph nodes initially increased in size and required drainage to prevent bursting, then settled patient treated with 6 months of standard TB treatment and fully recovered. www.thetruthabouttb.org
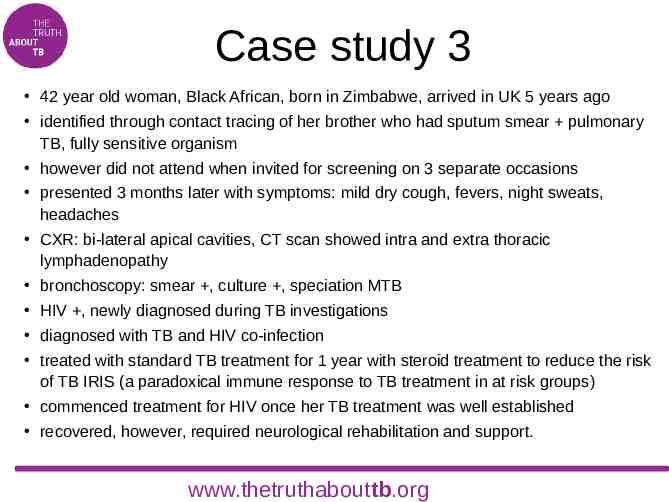
Case study 3 42 year old woman, Black African, born in Zimbabwe, arrived in UK 5 years ago identified through contact tracing of her brother who had sputum smear pulmonary TB, fully sensitive organism however did not attend when invited for screening on 3 separate occasions presented 3 months later with symptoms: mild dry cough, fevers, night sweats, headaches CXR: bi-lateral apical cavities, CT scan showed intra and extra thoracic lymphadenopathy bronchoscopy: smear , culture , speciation MTB HIV , newly diagnosed during TB investigations diagnosed with TB and HIV co-infection treated with standard TB treatment for 1 year with steroid treatment to reduce the risk of TB IRIS (a paradoxical immune response to TB treatment in at risk groups) commenced treatment for HIV once her TB treatment was well established recovered, however, required neurological rehabilitation and support. www.thetruthabouttb.org
Blank: for your case study (1) www.thetruthabouttb.org
Blank: for your case study (2) www.thetruthabouttb.org
Further information and resources TB Alert is the UK's national tuberculosis charity – the only charity working solely on fighting TB in the UK and overseas. The Truth About TB is TB Alert’s awareness programme. For information leaflets or awareness materials to display in your area of work: www.thetruthabouttb.org/resources/awareness-raising-resources For information about TB and patient stories: www.thetruthabouttb.org www.thetruthabouttb.org
References and further reading Collaborative TB Strategy for England 2015-2020: www.gov.uk/government/uploads/system/uploads/attachment data/file/40323 1/Collaborative TB Strategy for England 2015 2020 .pdf Tuberculosis: NICE, January 2016: www.nice.org.uk/guidance/ng33 Tuberculosis case management and cohort review, guidance for health professionals, RCN, 2012 (with BTS, PHE, National Treatment Agency for Substance Misuse): www2.rcn.org.uk/ data/assets/pdf file/0010/439129/004204.pdf National Knowledge Service: www.gov.uk/government/collections/tuberculosis-and-other-mycobacterial-dis eases-diagnosis-screening-management-and-data#nks-tb-treatment-and-ma nagement-advice www.thetruthabouttb.org
References and further reading (cont’d) PHE website (Tuberculosis) – for TB annual report: www.gov.uk/government/collections/tuberculosis-and-other-mycobacterial-dise ases-diagnosis-screening-management-and-data PHE screening webpages: www.gov.uk/guidance/tuberculosis-screening PHE migrant health web pages: www.gov.uk/topic/health-protection/migrant-health-guide TB Alert’s national awareness programme The Truth About TB: www.thetruthabouttb.org Immunisation against infectious disease, DH, 2006: www.gov.uk/government/collections/immunisation-against-infectious-disease-th e-green-book www.thetruthabouttb.org
Thanks and credits TB Alert and Public Health England would like to thank Professor Chris Griffiths, Professor of Primary Care at Barts and The London, for chairing its primary care expert advisory group. We are also grateful to our advisers Steve Bradley, Dr Gill Craig, Katie Dee, Ann Dennis, Anna Hinton, Dr Mike Lane, Dr Jane Leese, Dr Justin Sacks, Dr Noel Snell, Natalie Winter and Heggy Wyatt. This resource was written by Cheryl Giles, TB specialist nurse at Brighton and Sussex University Hospitals. Dr Anjana Roy of Public Health England coordinated the surveys that informed this work, project management was by Dr Thoreya Swage, and project coordination by Mike Mandelbaum for TB Alert and Surinder Tamne for Public Health England. This teaching resource was developed alongside an e-learning course for primary care clinicians, available on the Royal College of GPs website at www.elearning.rcgp.org.uk/tb . 2016 update by Sarah Anderson, Jennifer Davidson, Gini Williams and Dominik Zenner, www.thetruthabouttb.org

Developed by TB Alert under The Truth About TB programme. In partnership with NHS England and Public Health England.