The Primary Care Behavioral Health (PCBH) Model: What You Need to
33 Slides746.20 KB
The Primary Care Behavioral Health (PCBH) Model: What You Need to Know Dr. Stacy Ogbeide Licensed Psychologist and Behavioral Health Consultant Zeke Sanders, MA and Pooja Datta, MEd Psychology Residents Beverly Bernal, MA, Psychology Extern UT Health San Antonio
Overview Behavioral Health Models of Integrated Care The Primary Care Behavioral Health (PCBH) model Q and A
Introductions Name? What has been your experience with primary care? (personal, professional) What do the terms “integrated care” mean to you?
Important Terms PCP Primary Care Provider Retains ultimate responsibility for patient care BHC Behavioral Health Consultant Member of the primary care team
How Important is BH in PC? What are the options for outpatient behavioral health services in Bexar county? How long does it take to access? How effective is referral?
Primary Care: IOM definition The provision of integrated, accessible health care services by clinicians who are accountable for addressing a large majority of personal health care needs, developing a sustained partnership with patients, and practicing in the context of family and community (IOM, 1996).

What is “Integrated Care”?
Integrated Care: Methods of Care IMPACT/Collaborative Care Model Chronic Care Model Co-Location Primary Care Behavioral Health (PCBH) Consultation Model
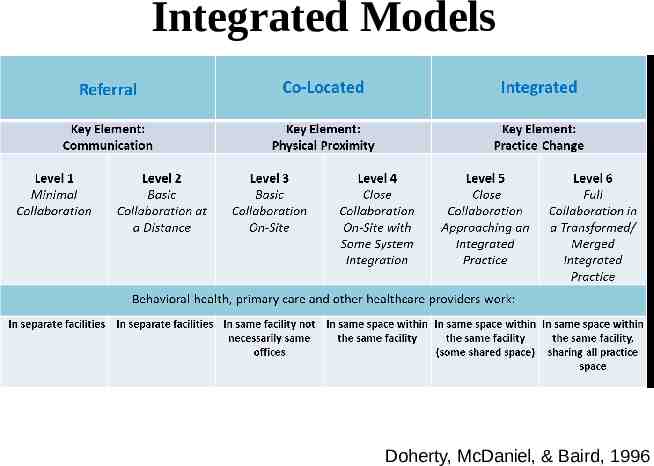
Integrated Models Doherty, McDaniel, & Baird, 1996
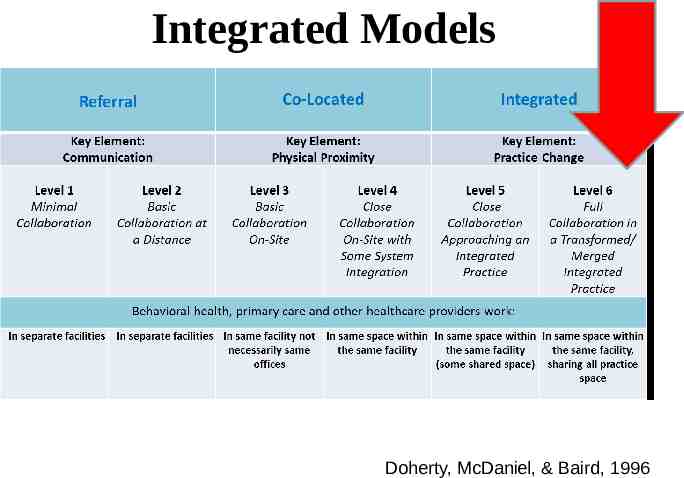
Integrated Models Doherty, McDaniel, & Baird, 1996

What is “Primary Care Behavioral Health (PCBH)”?
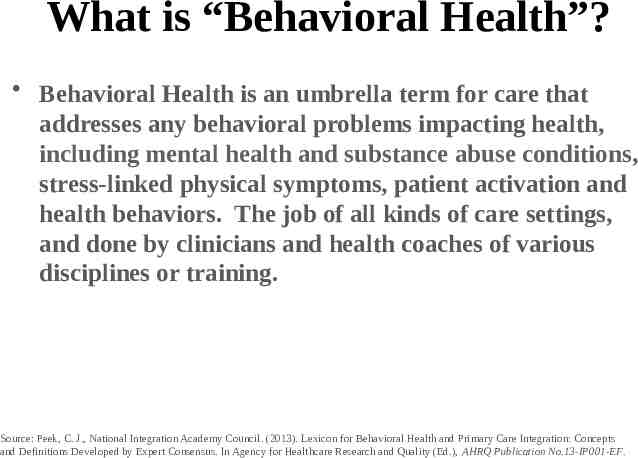
What is “Behavioral Health”? Behavioral Health is an umbrella term for care that addresses any behavioral problems impacting health, including mental health and substance abuse conditions, stress-linked physical symptoms, patient activation and health behaviors. The job of all kinds of care settings, and done by clinicians and health coaches of various disciplines or training. Source: Peek, C. J., National Integration Academy Council. (2013). Lexicon for Behavioral Health and Primary Care Integration: Concepts and Definitions Developed by Expert Consensus. In Agency for Healthcare Research and Quality (Ed.), AHRQ Publication No.13-IP001-EF.
Primary Care Behavioral Health A Definition The PCBH model combines medical and behavioral health services to more fully address the spectrum of problems that patients bring to their primary medical care providers. It allows patients to feel that, for almost any problem, they have come to the right place. Dr. Alexander Blount
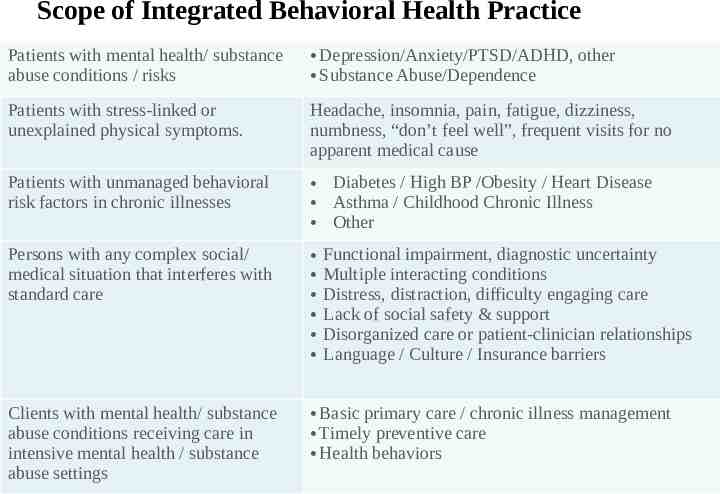
Scope of Integrated Behavioral Health Practice Patients with mental health/ substance abuse conditions / risks Depression/Anxiety/PTSD/ADHD, other Substance Abuse/Dependence Patients with stress-linked or unexplained physical symptoms. Headache, insomnia, pain, fatigue, dizziness, numbness, “don’t feel well”, frequent visits for no apparent medical cause Patients with unmanaged behavioral risk factors in chronic illnesses Diabetes / High BP /Obesity / Heart Disease Asthma / Childhood Chronic Illness Other Persons with any complex social/ medical situation that interferes with standard care Clients with mental health/ substance abuse conditions receiving care in intensive mental health / substance abuse settings Basic primary care / chronic illness management Timely preventive care Health behaviors Functional impairment, diagnostic uncertainty Multiple interacting conditions Distress, distraction, difficulty engaging care Lack of social safety & support Disorganized care or patient-clinician relationships Language / Culture / Insurance barriers
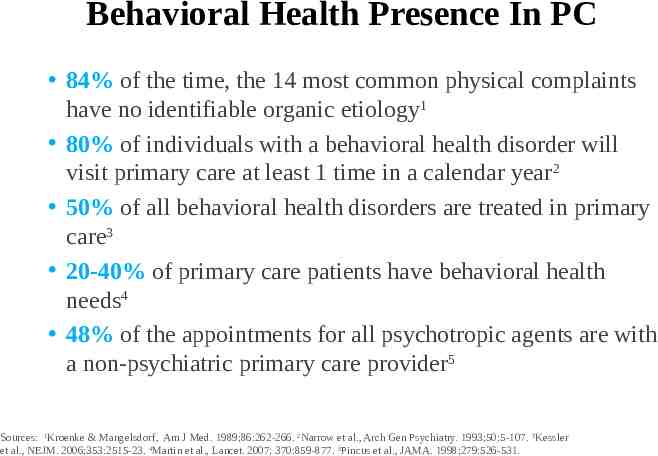
Behavioral Health Presence In PC 84% of the time, the 14 most common physical complaints have no identifiable organic etiology1 80% of individuals with a behavioral health disorder will visit primary care at least 1 time in a calendar year2 50% of all behavioral health disorders are treated in primary care3 20-40% of primary care patients have behavioral health needs4 48% of the appointments for all psychotropic agents are with a non-psychiatric primary care provider5 Sources: 1Kroenke & Mangelsdorf, Am J Med. 1989;86:262-266. 2Narrow et al., Arch Gen Psychiatry. 1993;50:5-107. 3Kessler et al., NEJM. 2006;353:2515-23. 4Martin et al., Lancet. 2007; 370:859-877. 5Pincus et al., JAMA. 1998;279:526-531.
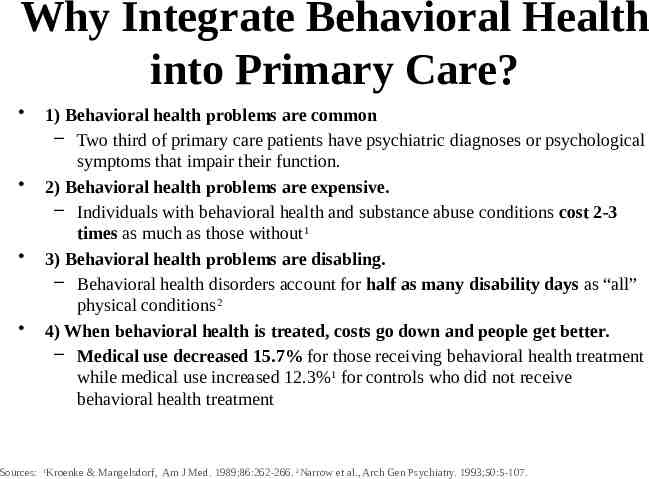
Why Integrate Behavioral Health into Primary Care? 1) Behavioral health problems are common – Two third of primary care patients have psychiatric diagnoses or psychological symptoms that impair their function. 2) Behavioral health problems are expensive. – Individuals with behavioral health and substance abuse conditions cost 2-3 times as much as those without1 3) Behavioral health problems are disabling. – Behavioral health disorders account for half as many disability days as “all” physical conditions2 4) When behavioral health is treated, costs go down and people get better. – Medical use decreased 15.7% for those receiving behavioral health treatment while medical use increased 12.3%1 for controls who did not receive behavioral health treatment Sources: 1Kroenke & Mangelsdorf, Am J Med. 1989;86:262-266. 2Narrow et al., Arch Gen Psychiatry. 1993;50:5-107.
What does this look like?

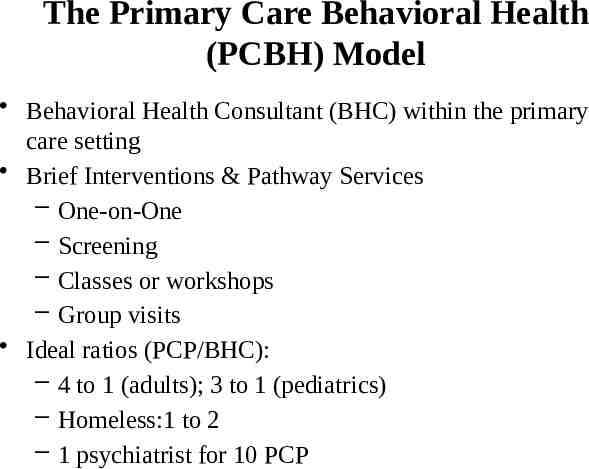
The Primary Care Behavioral Health (PCBH) Model Behavioral Health Consultant (BHC) within the primary care setting Brief Interventions & Pathway Services – One-on-One – Screening – Classes or workshops – Group visits Ideal ratios (PCP/BHC): – 4 to 1 (adults); 3 to 1 (pediatrics) – Homeless:1 to 2 – 1 psychiatrist for 10 PCP
Who is the Behavioral Health Consultant? 1) Knows brief assessment and brief behavioral interventions 2) Familiar with the “primary care way” of seeing patients 3) Works as a partner is seeing the panel of patients; is not to simply accept referrals 4) There to relieve the pressure off of the PCPs schedule and makes the care plan more effective and comprehensive
PCBH Model GATHER Generalist Accessible Team-based High productivity Educator Routine (pathways, regular care component) Care structure – Brief visits (15-25 minutes) – Consultation model
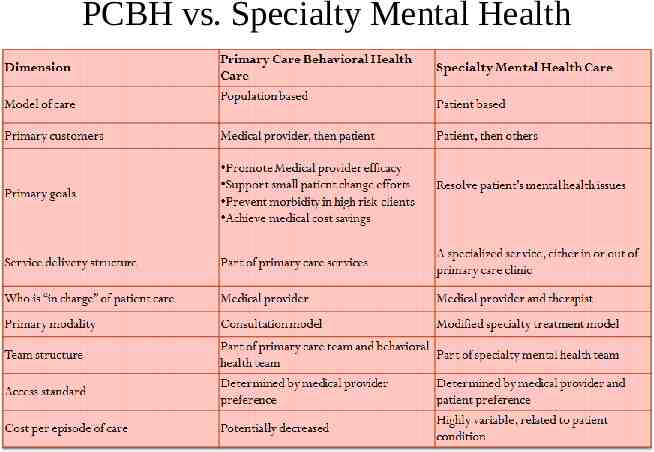
PCBH vs. Specialty Mental Health
Why be brief? Primary care fast-paced Lots of patients “On-Demand” services Population health focus (think vertical versus horizontal) Problem-focused Clear plan focused on patient’s strengths and abilities
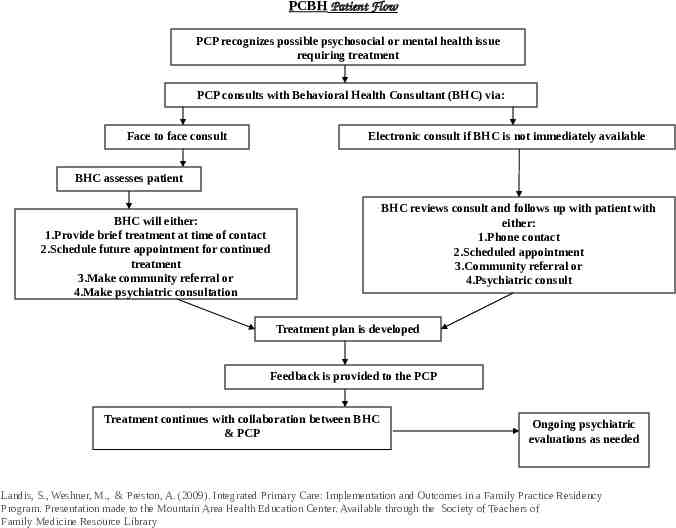
PCBH Patient Flow PCP recognizes possible psychosocial or mental health issue requiring treatment PCP consults with Behavioral Health Consultant (BHC) via: Face to face consult Electronic consult if BHC is not immediately available BHC assesses patient BHC reviews consult and follows up with patient with either: 1.Phone contact 2.Scheduled appointment 3.Community referral or 4.Psychiatric consult BHC will either: 1.Provide brief treatment at time of contact 2.Schedule future appointment for continued treatment 3.Make community referral or 4.Make psychiatric consultation Treatment plan is developed Feedback is provided to the PCP Treatment continues with collaboration between BHC & PCP Ongoing psychiatric evaluations as needed Landis, S., Weshner, M., & Preston, A. (2009). Integrated Primary Care: Implementation and Outcomes in a Family Practice Residency Program. Presentation made to the Mountain Area Health Education Center. Available through the Society of Teachers of Family Medicine Resource Library
Wrap-Up Wrap-up Name one thing from today that you will implement starting now.
Questions/Discussion What questions do you have? What clinical problems do you think would be challenging to treat in primary care?
Resources
PCBH Resources PCBH Corner: Link: https://www.youtube.com/playlist?list PLvLh YdubBs5P-dw9IrSH7-TwTqM8fkqo
More Resources Resources available online – http://www.pcpci.org/resources/browse – Search ‘Behavioral Health Integration’ – http://www.mtnviewconsulting.com/ – Patient Education: http://champsonline.org/ToolsProducts/Clinical Resources/PatientEdTools/PatientEdHandouts. html
References and Resources Websites: AHRQ Academy for Integrating Behavioral Health and Primary Care: http://integrationacademy.ahrq.gov/ AIMS CENTER: http://aims.uw.edu/ Center for Integrated Primary Care: http://www.umassmed.edu/cipc/ Collaborative Family Healthcare Association: www.cfha.net Evolving Models of Behavioral Health Integration in primary Care. Milbank Memorial Fund 2010. http://www.milbank.org Lexicon for Behavioral Health and Primary Care Integration. AHRQ 2013: http://integrationacademy.ahrq.gov/sites/ default/files/Lexicon.pdf National Alliance on Mental Illness. Integrating Mental Health & Pediatric Primary Care Resource Center: http://www.nami.org SAMHSA/HRSA Center for Integrated Health Solutions: http://www.integration.samhsa.gov Some of the information from this presentation was adapted from PCPCC’s Behavioral Health Task Force Slide Deck. Last updated September 2014. Link: https://www.pcpcc.org/
References Bridges, A. J., Gregus, S. J., Hernandez Rodriguez, J., Andrews, A. R., III, Villalobos, B. T., Pastrana, F. A., & Cavell, T. A. (2015, March 16). Diagnoses, intervention strategies, and rates of functional improvement in integrated behavioral health care patients. Journal of Consulting and Clinical Psychology. Advance online publication. Cape, J., Whittington, C., Buszewicz, M., Wallace, P., Underwood, L. (2010). Brief psychological therapies for anxiety and depression in primary care: Meta-analysis and metaaggression. BMC Medicine, 8, http://www.biomedcentral.com/1741-7015/8/38 Chen, W. C., Chu, H., Lu, R., Chou, Y. H., Chen, C. H., Chang, Y., O’Brien, A. P., & Chou, K. (2009). Efficacy of progressive muscle relaxation training in reducing anxiety in patients with acute Schizophrenia. Journal of Clinical Nursing, 18, 2187-2196. doi: 10.1111/j.13652702.2008.02773.x deGruy, F. (2015). Integrated care: Tools, maps, and leadership. Journal of the American Board of Family Medicine, 28, S107-S110. doi: 10.3122/jabfm.2015.S1.150106 Hegel, M., Barrett, J. E., & Oxman, T. E. (2000). Training therapists in problem solving treatment of depressive disorders in primary care: Lessons learned from the “Treatment Effectiveness Project.” Family, Systems, & Health, 18, 423-435.
References “PEARLS” (2016). Pearls program overview. Retrieved from http://www.pearlsprogram.org/Our-Program.aspx Ray-Sannerud, B. N., Morrow, C. E., Kanzler, K. E., Dolan, D. C., Corso, K. A., Corso, M. L., . Bryan, C. J., (2012). Longitudinal outcomes after brief behavioral health intervention in an integrated primary care clinic. Family, Systems, & Health, 30(1), 61-70. doi: 10.1037/a0027029 Robinson, P. J. (2013). Treatment of depression. In O’Donohoe, W. (Ed.) Case Studies in Clinical Psychological Science. NY: Oxford University Press.
References Robinson, P. J., Gould, D., & Strosahl, K. D. (2011). Real Behavior Change in Primary Care. Strategies and Tools for Improving Outcomes and Increasing Job Satisfaction. Oakland: New Harbinger Robinson, P. J. & Reiter, J. T. (2016). Behavioral Consultation and Primary Care: A Guide to Integrating Services, 2nd Edition. NY: Springer. Robinson, P. & Strosahl, K. (2009) Behavioral consultation and primary care: Lessons learned. Journal of Clinical Psychology in Medical Settings,16, 58-71. Strosahl, K. D., Robinson, P. J., & Gustavsson, T. (2012). Brief Interventions for Radical Change: Principles and Practice of Focused Acceptance and Commitment Therapy. Oakland, CA: New Harbinger.