The FUNDamentals of DME Equipment: A Guide for Selection,
44 Slides1.26 MB
The FUNDamentals of DME Equipment: A Guide for Selection, Acquisition, and Delivery of Complex Rehab Technology Beth Beach MS, OTR/L, ATP Tony Leo MOT/L, ATP
AEL/NRTTS
What is Durable Medical Equipment (DME)? Durable Medical Equipment must meet the following criteria (Medicare.gov 2014): 1. Is durable or long-lasting 2. Is used for a medical reason 3. Is not usually useful to someone who isn’t sick, injured or disabled 4. Is used in the home
What is complex rehab technology (CRT)? “Complex Rehab Technology products and services include medically necessary, individually-configured manual and power wheelchair systems, adaptive seating systems, alternative positioning systems, and other mobility devices that require evaluation, fitting, configuration, adjustment or programming.” (NuMotion/NCART)

Who needs complex rehab technology? “Primary diagnoses that can require Complex Rehab Technology include, but are not limited to, spinal cord injury, traumatic brain injury, cerebral palsy, muscular dystrophy, spina bifida, osteogenesis imperfecta, arthrogryposis, amyotrophic lateral sclerosis (ALS), multiple sclerosis, demyelinating diseases, myelopathy, progressive muscular atrophy, anterior horn cell diseases, post polio paralysis, cerebellar degeneration, dystonia, Huntington’s chorea, spinocerebellar disease, amputation, paralysis or paresis, or any other disability or disease that may require the use of such individually configured products and services.” (NuMotion/NCART)
General Funding Guidelines for CRT The client requires the equipment long-term The equipment will improve the client’s function MRADLs) within the home and, if under 21, the school environment Other less expensive/extensive equipment has been considered but will not meet the client’s current and anticipated needs (i.e. progressive disease)
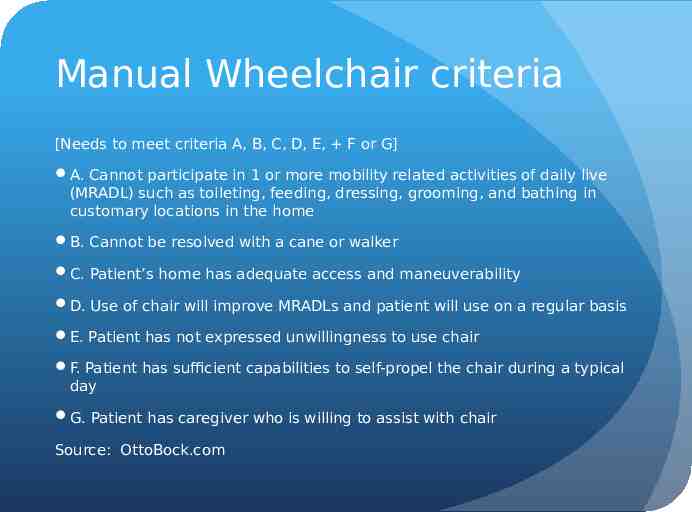
Manual Wheelchair criteria [Needs to meet criteria A, B, C, D, E, F or G] A. Cannot participate in 1 or more mobility related activities of daily live (MRADL) such as toileting, feeding, dressing, grooming, and bathing in customary locations in the home B. Cannot be resolved with a cane or walker C. Patient’s home has adequate access and maneuverability D. Use of chair will improve MRADLs and patient will use on a regular basis E. Patient has not expressed unwillingness to use chair F. Patient has sufficient capabilities to self-propel the chair during a typical day G. Patient has caregiver who is willing to assist with chair Source: OttoBock.com

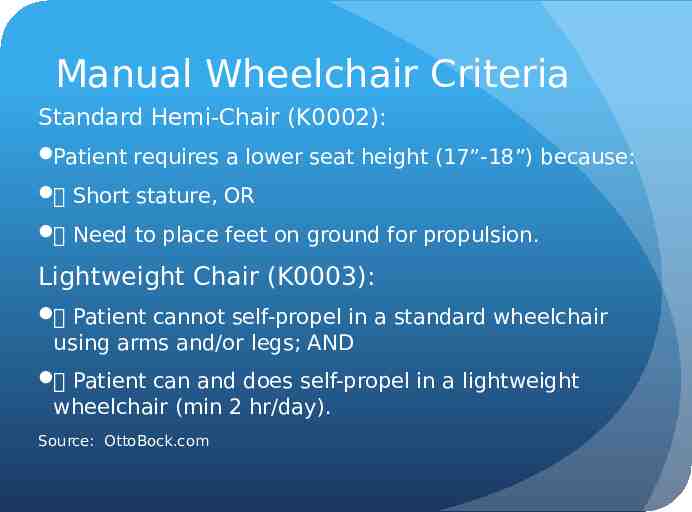
Manual Wheelchair Criteria Standard Hemi-Chair (K0002): Patient requires a lower seat height (17”-18”) because: Short stature, OR Need to place feet on ground for propulsion. Lightweight Chair (K0003): Patient cannot self-propel in a standard wheelchair using arms and/or legs; AND Patient can and does self-propel in a lightweight wheelchair (min 2 hr/day). Source: OttoBock.com
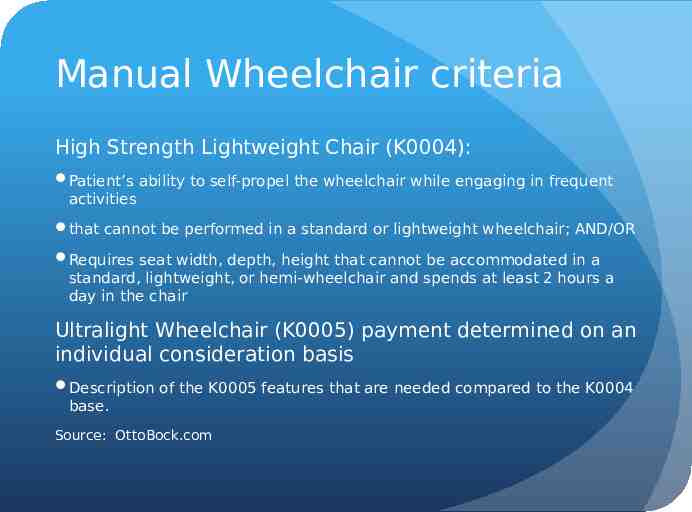
Manual Wheelchair criteria High Strength Lightweight Chair (K0004): Patient’s ability to self-propel the wheelchair while engaging in frequent activities that cannot be performed in a standard or lightweight wheelchair; AND/OR Requires seat width, depth, height that cannot be accommodated in a standard, lightweight, or hemi-wheelchair and spends at least 2 hours a day in the chair Ultralight Wheelchair (K0005) payment determined on an individual consideration basis Description of the K0005 features that are needed compared to the K0004 base. Source: OttoBock.com
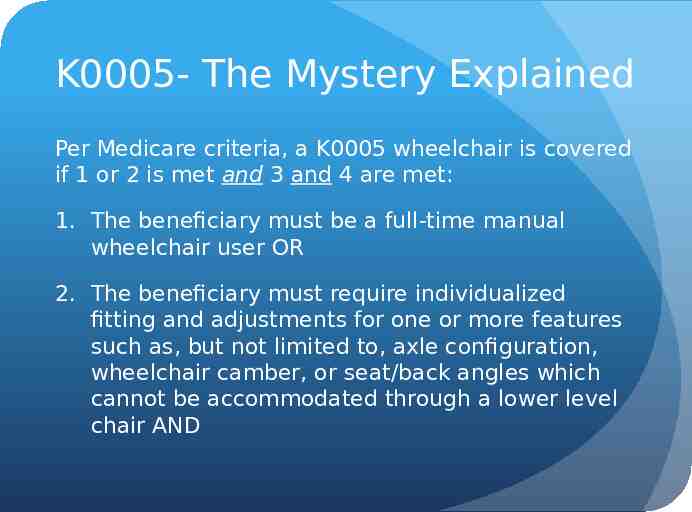
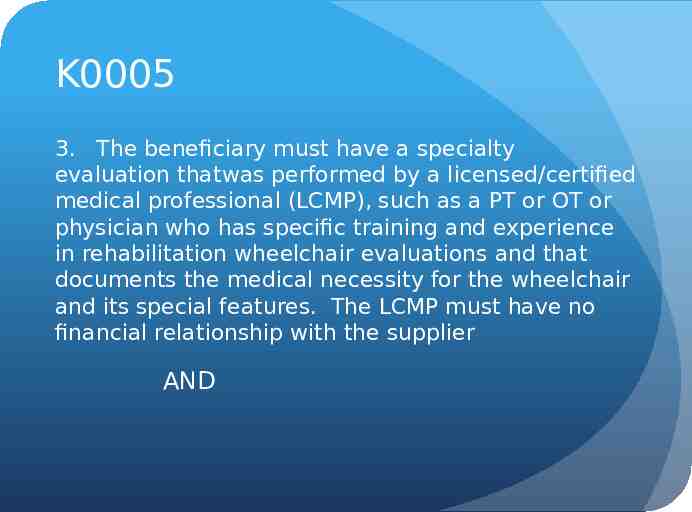
K0005- The Mystery Explained Per Medicare criteria, a K0005 wheelchair is covered if 1 or 2 is met and 3 and 4 are met: 1. The beneficiary must be a full-time manual wheelchair user OR 2. The beneficiary must require individualized fitting and adjustments for one or more features such as, but not limited to, axle configuration, wheelchair camber, or seat/back angles which cannot be accommodated through a lower level chair AND

K0005 3. The beneficiary must have a specialty evaluation thatwas performed by a licensed/certified medical professional (LCMP), such as a PT or OT or physician who has specific training and experience in rehabilitation wheelchair evaluations and that documents the medical necessity for the wheelchair and its special features. The LCMP must have no financial relationship with the supplier AND
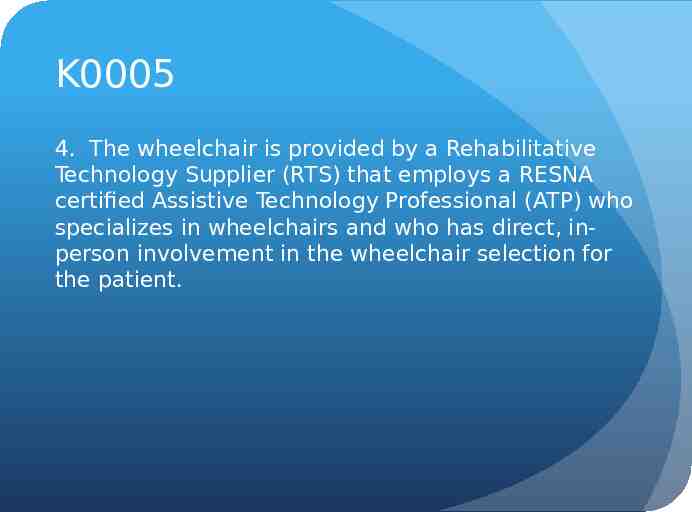
K0005 4. The wheelchair is provided by a Rehabilitative Technology Supplier (RTS) that employs a RESNA certified Assistive Technology Professional (ATP) who specializes in wheelchairs and who has direct, inperson involvement in the wheelchair selection for the patient.
Tilt in Space Wheelchairs
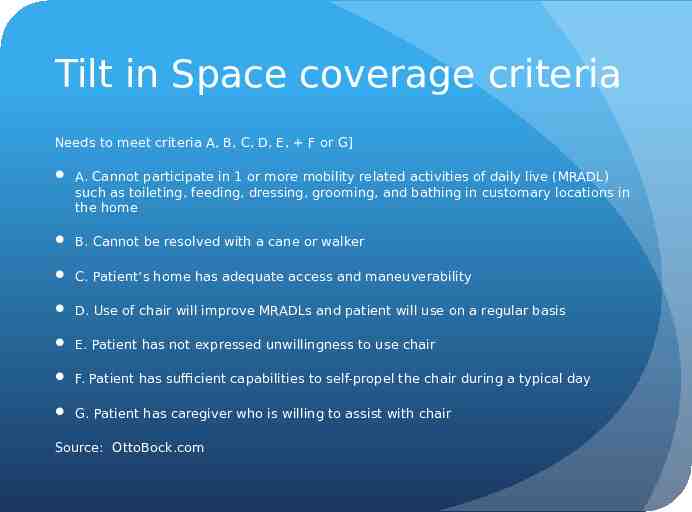
Tilt in Space coverage criteria Needs to meet criteria A, B, C, D, E, F or G] A. Cannot participate in 1 or more mobility related activities of daily live (MRADL) such as toileting, feeding, dressing, grooming, and bathing in customary locations in the home B. Cannot be resolved with a cane or walker C. Patient’s home has adequate access and maneuverability D. Use of chair will improve MRADLs and patient will use on a regular basis E. Patient has not expressed unwillingness to use chair F. Patient has sufficient capabilities to self-propel the chair during a typical day G. Patient has caregiver who is willing to assist with chair Source: OttoBock.com

Tilt in Space coverage criteria Client must have a specialty evaluation that was performed by a licensed/certified medical professional (LCMP), as previously noted. The wheelchair is provided by a Rehabilitative Technology Supplier (RTS) that employs a RESNAcertified Assistive Technology Professional (ATP) who specializes in wheelchairs and who has direct, in-person involvement in the wheelchair selection for the patient. Note: as of 4/1/14, tilt in space frames are rentals under Medicare

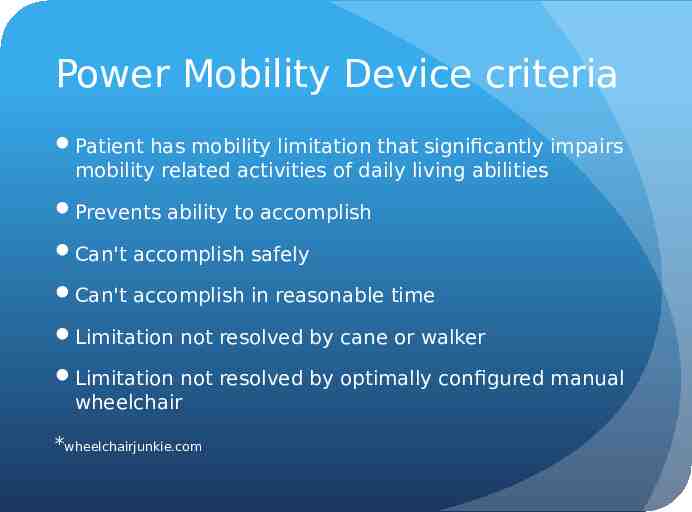
Power Mobility Device criteria Patient has mobility limitation that significantly impairs mobility related activities of daily living abilities Prevents ability to accomplish Can't accomplish safely Can't accomplish in reasonable time Limitation not resolved by cane or walker Limitation not resolved by optimally configured manual wheelchair *wheelchairjunkie.com
POV vs. Power Wheelchair In order to request a power wheelchair, a power operated vehicle, or scooter must be ruled out as an option for the client POV has a tiller for operation POV has captain’s type seating POV is usually longer than a power chair Transfers can be an issue with a POV

Power Chair Groups Group 1 power chair Standard integrated or remote proportional control input device- cannot be upgraded for specialty controls Non-expandable controller- cannot be upgraded Accommodates non-powered options (i.e. manual recline and manual elevating legrests) These chairs are not considered complex rehab technology and fall under competitive bidding for Medicare
Group 1 Power Wheelchair
Power Chair Groups Group 2 power chair Standard integrated or remote proportional control input device Accommodates seating and positioning components such as specialty backs, cushions Can accommodate power functions such as power tilt and/or recline These cannot be upgraded with specialty controls and power functions are more limited- not CRT under Medicare

Group 2 Power Wheelchair

Power Chair Groups Group 3 power chairs Standard integrated or remote proportional control input device Accommodates seating and positioning components such as specialty backs and cushions Can be upgraded with specialty controls Has options for multiple power functions This is the first category considered CRT under Medicare

Group 3 Power wheelchairs Mid-wheel Front wheel Rear wheel

Power Chair Groups Group 4 power chairs Not covered under Medicare as they have essentially the same options as group 3, just are more heavy duty and faster. Group 5 power chairs These are pediatric power wheelchairs

Power Chair Groups Group 4 Group 5

Seating Skin Protection and/or Positioning Seat Cushions Positioning Backs Positioning Accessories Custom Fabricated Seating Must have a manual wheelchair or power wheelchair with sling/solid seat and back and meet MCR coverage criteria for the skin protection and/or positioning seat or back.

Role of the therapist Evaluate patient and document need for complex rehab technology in a letter of medical necessity Communicate with other team members- rehab technology specialist (RTS), physician, treating therapists, case managers, client and family

Role of the therapist 50% of orders in the Medicare Demonstration Project are denied. A majority of the denied prior authorizations relied on Physician chart notes and did not include a therapy evaluation. When the customer sees a therapist for a wheelchair evaluation, the approval rate jumps to around 90%. When there is a comprehensive therapy evaluation, the process moves faster and the customer is more likely to get their chair approved without needing repeat visits.
Letter of Medical Necessity Introduces the client- age, sex, diagnosis, past medical history Discusses what equipment the client has presently and what the problems are with the equipment Standard therapy evaluation including strength, range of motion, bed/floor mobility, sitting balance, head control, tone, etc. States the equipment recommended and WHY each component is necessary
Letter of Medical Necessity Clinician or the Clinic’s own form (meeting all coverage criteria) VOTA 2014\Medicare LMN Requirements.pdf Orion FMEVOTA 2014\Group 3 Power Multiple Seat functions - Copy.pdf Illinois Seating/Mobility Evaluation (12 Page Eval)VOTA 2014\Seating Eval Form from Illinois Public Aid 019.pdf State Medicaid and other Payer Specific Wheelchair or Equipment Forms; as required but must be approved for Medicare FundingVOTA 2014\handout- sample CHKD LMN.doc
Role of the ATP/RTS The ATP can never complete any portion of the PT/OT Evaluation prior to, or after the evaluation. The only exception is the demographics portion of the form, which may be completed before the evaluation. The ATP must complete a separate Client Assessment for all Medicare orders requiring ATP involvement per Medicare policy. The Client Assessment must be completed, signed and dated by the ATP, including credentials to prove involvement in the mobility evaluation
Medicare Forms F2F Chart notes 7 element prescription
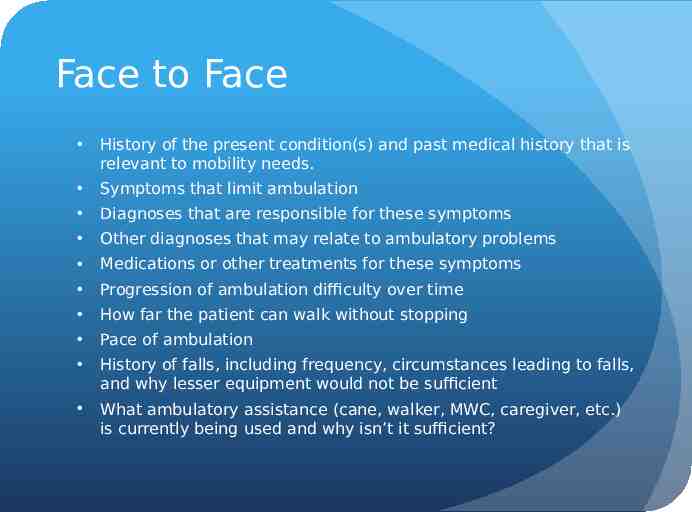
Face to Face History of the present condition(s) and past medical history that is relevant to mobility needs. Symptoms that limit ambulation Diagnoses that are responsible for these symptoms Other diagnoses that may relate to ambulatory problems Medications or other treatments for these symptoms Progression of ambulation difficulty over time How far the patient can walk without stopping Pace of ambulation History of falls, including frequency, circumstances leading to falls, and why lesser equipment would not be sufficient What ambulatory assistance (cane, walker, MWC, caregiver, etc.) is currently being used and why isn’t it sufficient?
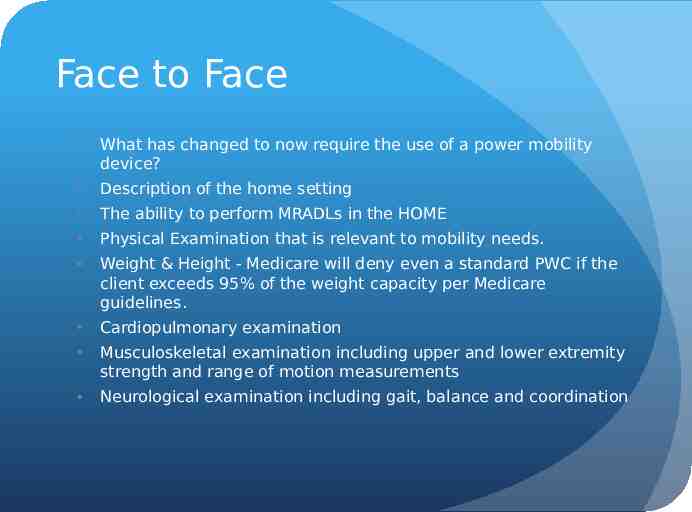
Face to Face What has changed to now require the use of a power mobility device? Description of the home setting The ability to perform MRADLs in the HOME Physical Examination that is relevant to mobility needs. Weight & Height - Medicare will deny even a standard PWC if the client exceeds 95% of the weight capacity per Medicare guidelines. Cardiopulmonary examination Musculoskeletal examination including upper and lower extremity strength and range of motion measurements Neurological examination including gait, balance and coordination
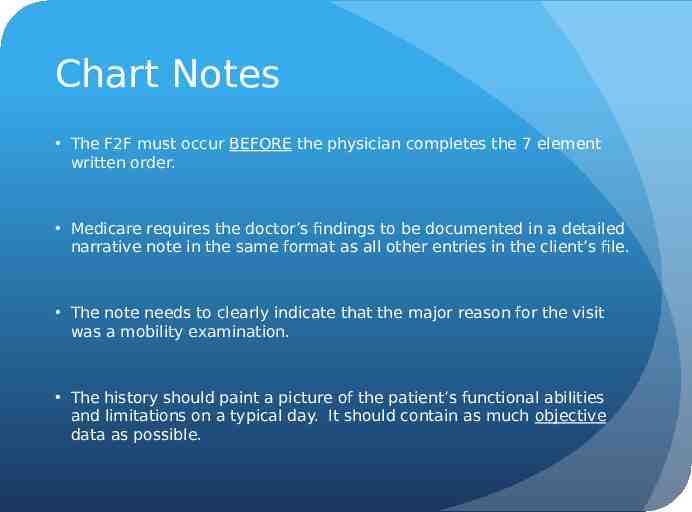
Chart Notes The F2F must occur BEFORE the physician completes the 7 element written order. Medicare requires the doctor’s findings to be documented in a detailed narrative note in the same format as all other entries in the client’s file. The note needs to clearly indicate that the major reason for the visit was a mobility examination. The history should paint a picture of the patient’s functional abilities and limitations on a typical day. It should contain as much objective data as possible.
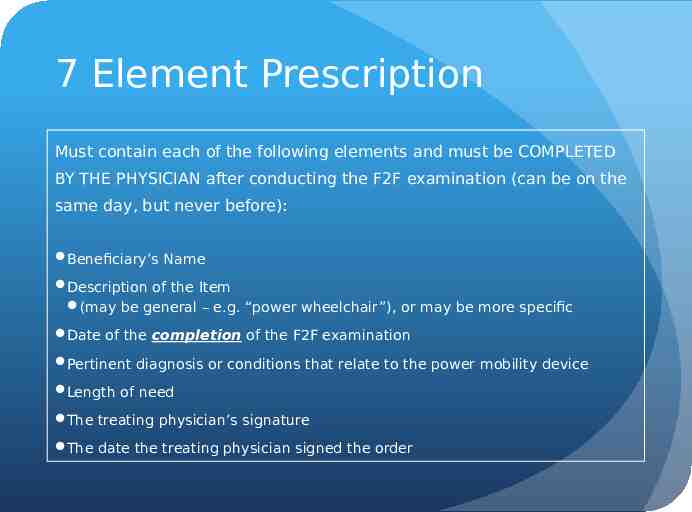
7 Element Prescription Must contain each of the following elements and must be COMPLETED BY THE PHYSICIAN after conducting the F2F examination (can be on the same day, but never before): Beneficiary’s Name Description of the Item (may be general – e.g. “power wheelchair”), or may be more specific Date of the completion of the F2F examination Pertinent diagnosis or conditions that relate to the power mobility device Length of need The treating physician’s signature The date the treating physician signed the order
7 ELEMENT PRESCRIPTION — The Numotion 7 Element Written Order has been revised for easier use. — Contains a more accurate statement under element #2 to assist the physician with understanding the face to face completion date. — The 7 Element Written Order is to be completed entirely by the physician. ***graphic abbreviated for content only — No fields can be completed by the supplier or medical office staff. 40
Appeals Important to be sure that you review the insurance’s coverage criteria for the equipment prior to filing an appeal First appeal is usually written. Can be filed by the patient, family or representative of the family. Must have an authorized representative statement signed by the patient/family to file the appeal If appeal is denied, the next step is usually a telephone hearing Some insurances allow peer to peer reviews
Insurance Trends Denial of standers as “experimental and investigational” Denial of adaptive strollers for distances as “convenience to the caregiver” or “restraint of the individual” Denial of adaptive beds for safety purposes Denial of back up wheelchairs or strollers Denial of bath equipment for very small children and teenagers/young adults “convenience items”
Alternate Funding Sources Virginia Birth Injury Fund Charities- both local and national EPSDT VOTA 2014\Handout- RESOURCES FOR FUNDING A DAPTIVE EQUIPMENT (VA).doc
Questions?