Pathway to Excellence in Long-Term ® Care : Creating and Sustaining
24 Slides5.07 MB
Pathway to Excellence in Long-Term Care : Creating and Sustaining a Culture of Excellence
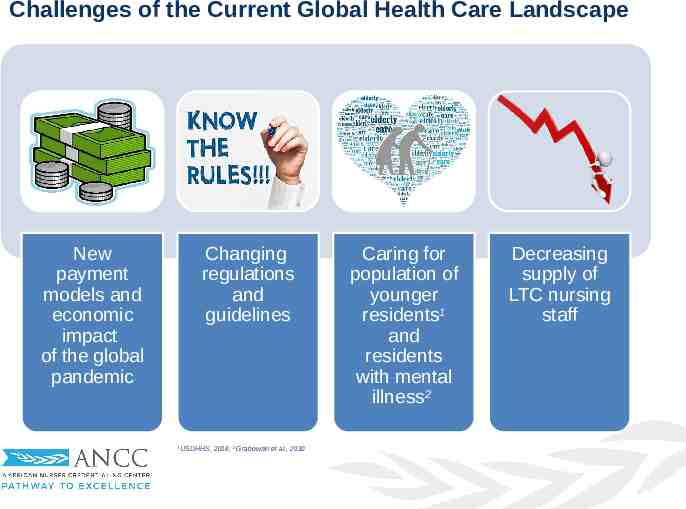
Challenges of the Current Global Health Care Landscape New payment models and economic impact of the global pandemic Changing regulations and guidelines 1 USDHHS, 2016; 2 Grabowski et al., 2010 Caring for population of younger residents1 and residents with mental illness2 Decreasing supply of LTC nursing staff
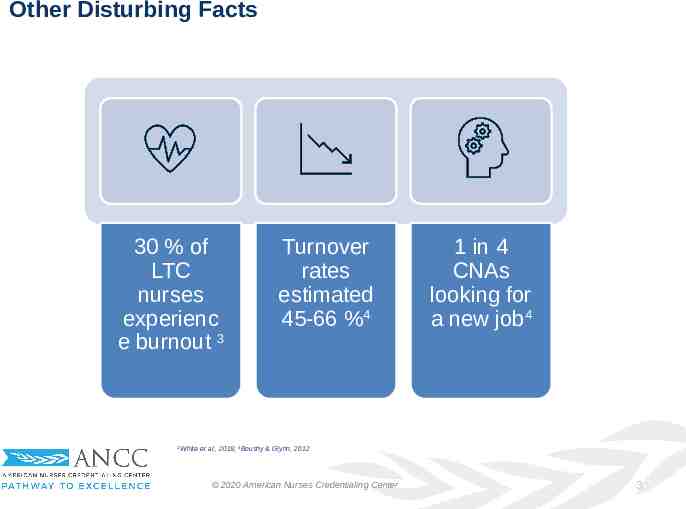
Other Disturbing Facts 30 % of LTC nurses experienc e burnout 3 3 Turnover rates estimated 45-66 %4 1 in 4 CNAs looking for a new job4 White et al., 2019; 4Boushy & Glynn, 2012 2020 American Nurses Credentialing Center 3
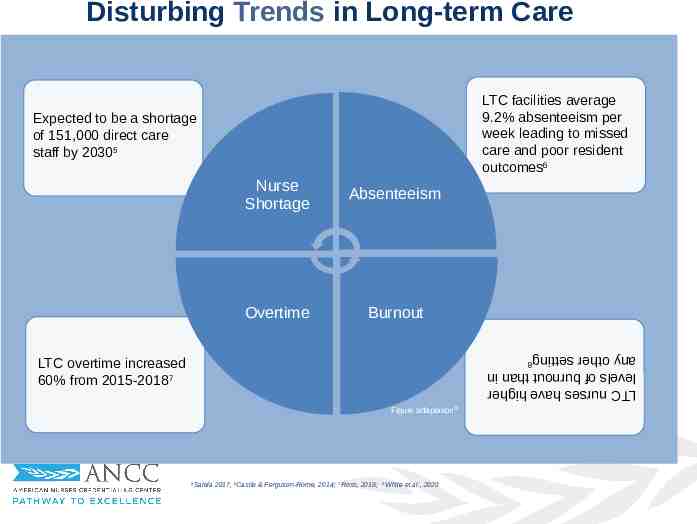
Disturbing Trends in Long-term Care LTC facilities average 9.2% absenteeism per week leading to missed care and poor resident outcomes6 Expected to be a shortage of 151,000 direct care staff by 20305 Nurse Shortage Absenteeism Overtime Burnout LTC nurses have higher levels of burnout than in any other setting8 LTC overtime increased 60% from 2015-20187 Figure adaptation20 Salela 2017, 6Castle & Ferguson-Rome, 2014; 7 Ross, 2018; 5 8 White et al., 2020
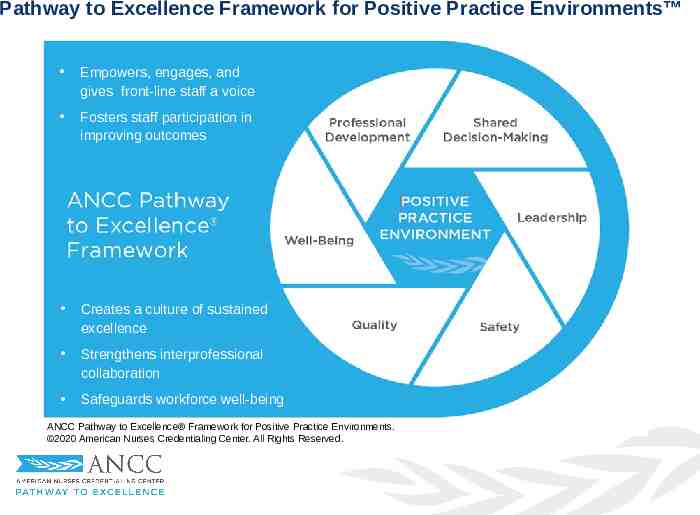
Pathway to Excellence Framework for Positive Practice Environments Empowers, engages, and gives front-line staff a voice Fosters staff participation in improving outcomes Creates a culture of sustained excellence Strengthens interprofessional collaboration Safeguards workforce well-being ANCC Pathway to Excellence Framework for Positive Practice Environments. 2020 American Nurses Credentialing Center. All Rights Reserved.

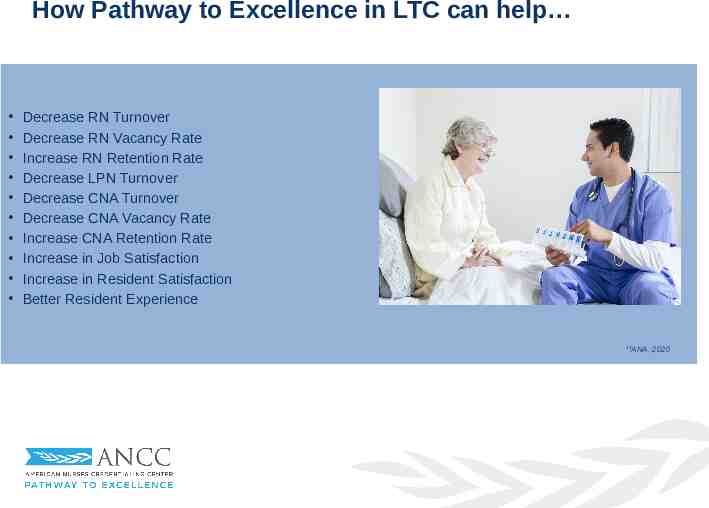
How Pathway to Excellence in LTC can help Decrease RN Turnover Decrease RN Vacancy Rate Increase RN Retention Rate Decrease LPN Turnover Decrease CNA Turnover Decrease CNA Vacancy Rate Increase CNA Retention Rate Increase in Job Satisfaction Increase in Resident Satisfaction Better Resident Experience 14 ANA, 2020
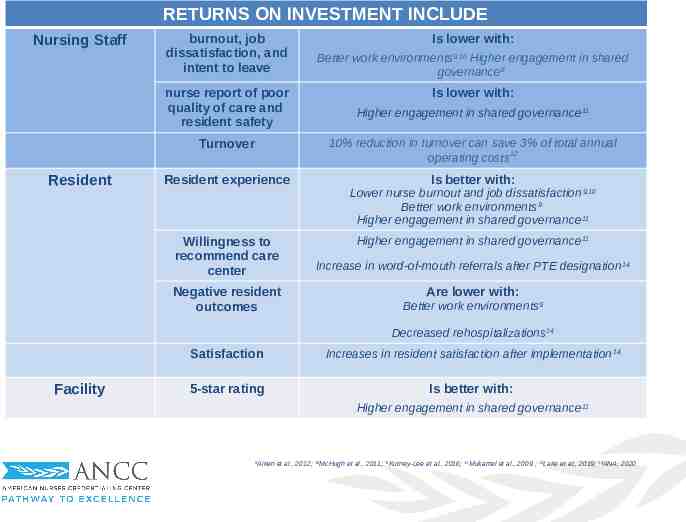
RETURNS ON INVESTMENT INCLUDE Nursing Staff burnout, job dissatisfaction, and intent to leave nurse report of poor quality of care and resident safety Turnover Resident Is lower with: Better work environments9,10 Higher engagement in shared governance8 Is lower with: Higher engagement in shared governance 11 10% reduction in turnover can save 3% of total annual 12 operating costs Resident experience Is better with: Lower nurse burnout and job dissatisfaction 9,10 Better work environments9 Higher engagement in shared governance 11 Willingness to recommend care center Negative resident outcomes Higher engagement in shared governance 11 Increase in word-of-mouth referrals after PTE designation 14 Are lower with: Better work environments9 Decreased rehospitalizations 14 Facility Satisfaction Increases in resident satisfaction after implementation 14 5-star rating Is better with: Higher engagement in shared governance 11 Aiken et al., 2012; 10McHugh et al., 2011; 11Kutney-Lee et al., 2016; 12Mukamel et al., 2009 ; 13Lake et al., 2019; 14ANA, 2020 9
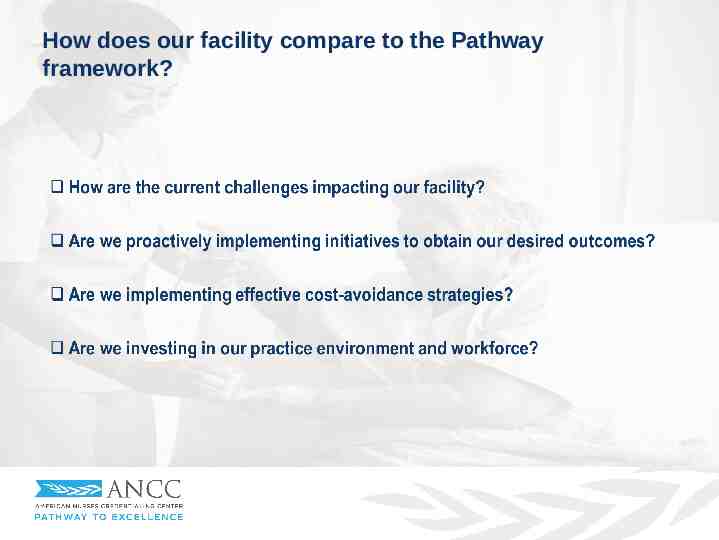
How does our facility compare to the Pathway framework?
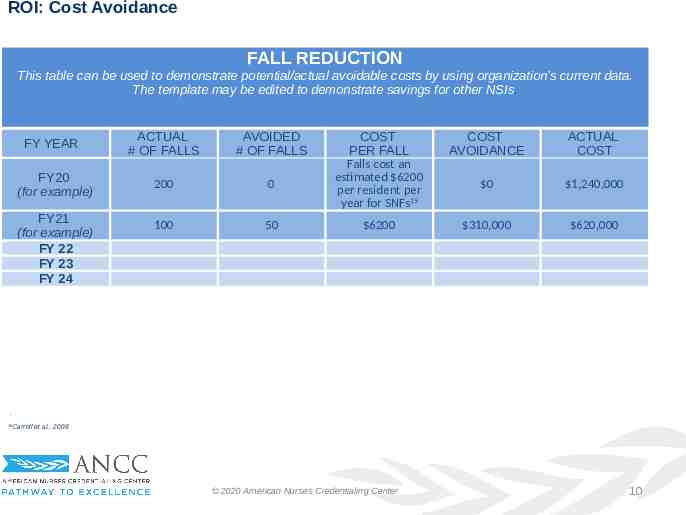
ROI: Cost Avoidance FALL REDUCTION This table can be used to demonstrate potential/actual avoidable costs by using organization’s current data. The template may be edited to demonstrate savings for other NSIs. FY YEAR FY20 (for example) FY21 (for example) FY 22 FY 23 FY 24 ACTUAL # OF FALLS AVOIDED # OF FALLS 200 0 100 50 COST PER FALL Falls cost an estimated 6200 per resident per year for SNFs15 COST AVOIDANCE ACTUAL COST 0 1,240,000 6200 310,000 620,000 . Carroll et al., 2008 15 2020 American Nurses Credentialing Center 10
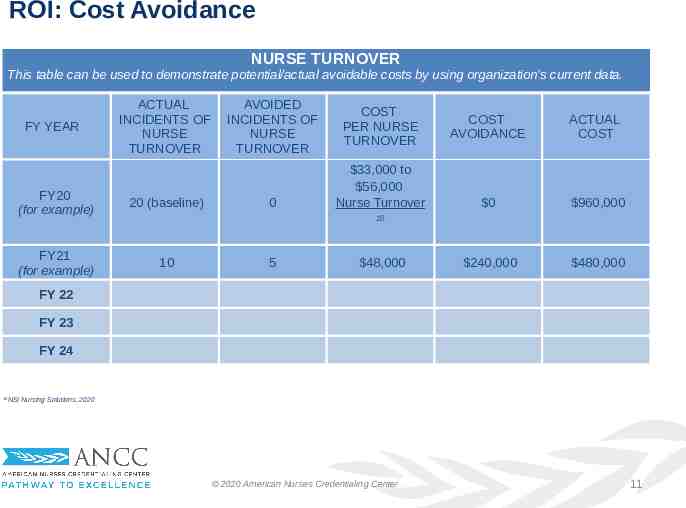
ROI: Cost Avoidance NURSE TURNOVER This table can be used to demonstrate potential/actual avoidable costs by using organization’s current data. FY YEAR ACTUAL INCIDENTS OF NURSE TURNOVER FY20 (for example) 20 (baseline) FY21 (for example) 10 AVOIDED INCIDENTS OF NURSE TURNOVER 0 COST PER NURSE TURNOVER 33,000 to 56,000 Nurse Turnover COST AVOIDANCE ACTUAL COST 0 960,000 240,000 480,000 16 5 48,000 FY 22 FY 23 FY 24 16 NSI Nursing Solutions, 2020 2020 American Nurses Credentialing Center 11
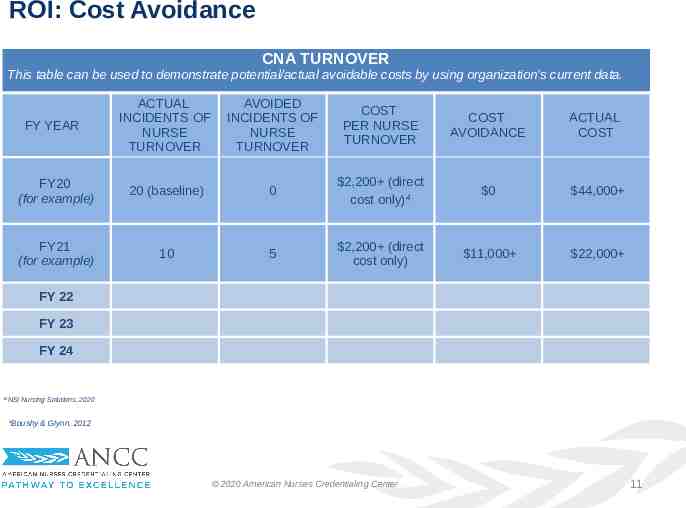
ROI: Cost Avoidance CNA TURNOVER This table can be used to demonstrate potential/actual avoidable costs by using organization’s current data. ACTUAL INCIDENTS OF NURSE TURNOVER AVOIDED INCIDENTS OF NURSE TURNOVER COST PER NURSE TURNOVER COST AVOIDANCE ACTUAL COST FY20 (for example) 20 (baseline) 0 2,200 (direct cost only)4 0 44,000 FY21 (for example) 10 5 2,200 (direct cost only) 11,000 22,000 FY YEAR FY 22 FY 23 FY 24 16 NSI Nursing Solutions, 2020 4 Boushy & Glynn, 2012 2020 American Nurses Credentialing Center 11
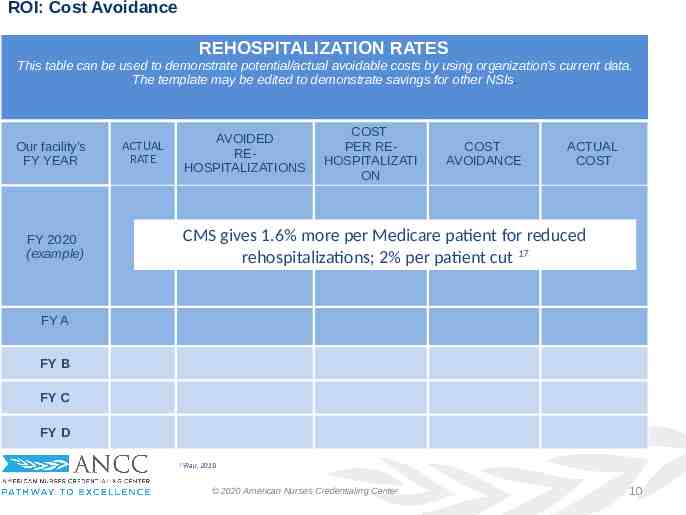
ROI: Cost Avoidance REHOSPITALIZATION RATES This table can be used to demonstrate potential/actual avoidable costs by using organization’s current data. The template may be edited to demonstrate savings for other NSIs. Our facility’s FY YEAR FY 2020 (example) AVOIDED REHOSPITALIZATIONS ACTUAL RATE COST PER REHOSPITALIZATI ON COST AVOIDANCE ACTUAL COST CMS gives 1.6% more per Medicare patient for reduced rehospitalizations; 2% per patient cut 17 FY A FY B FY C 9 Schimert et al., 2016 FY D 17 Rau, 2019 2020 American Nurses Credentialing Center 10
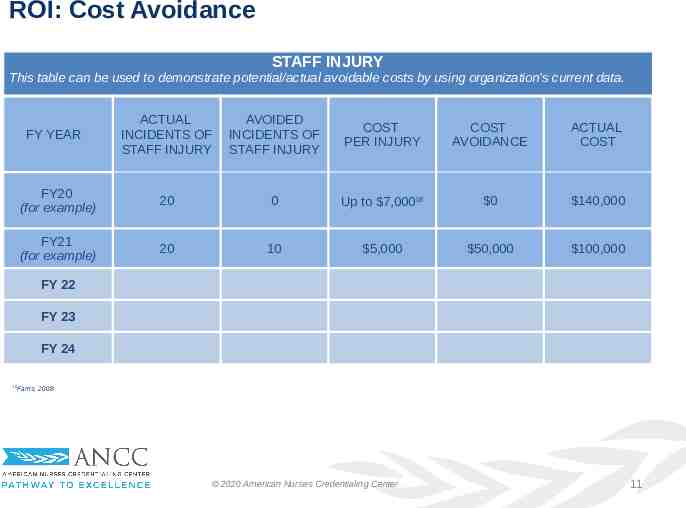
ROI: Cost Avoidance STAFF INJURY This table can be used to demonstrate potential/actual avoidable costs by using organization’s current data. ACTUAL INCIDENTS OF STAFF INJURY AVOIDED INCIDENTS OF STAFF INJURY COST PER INJURY COST AVOIDANCE ACTUAL COST FY20 (for example) 20 0 Up to 7,00018 0 140,000 FY21 (for example) 20 10 5,000 50,000 100,000 FY YEAR FY 22 FY 23 FY 24 18 Farris, 2008 2020 American Nurses Credentialing Center 11
Our frontline is our bottom line! Engagement of LTC Facility Name’s employees is key to our success Success is when resident safety and other facility outcomes are owned and become the responsibility of every single employee. Registered nurses follow physicians as the least engaged of the healthcare workforce19 19 Press Ganey 2019 2020 American Nurses Credentialing Center 2
Is the Pathway framework Right Fit for our facility? Is creating a positive practice environment aligned with your facility’s mission and vision? Will it help achieve your strategic objectives and desired outcomes? Does it address your challenges? Is creating an environment that nursing staff and other clinicians can call their professional home desired by the organization? Is investing in the workforce a priority for the facility? 2020 American Nurses Credentialing Center Is the international recognition desired by the facility? Does the facility recognize the importance of safeguarding staff well-being? 7

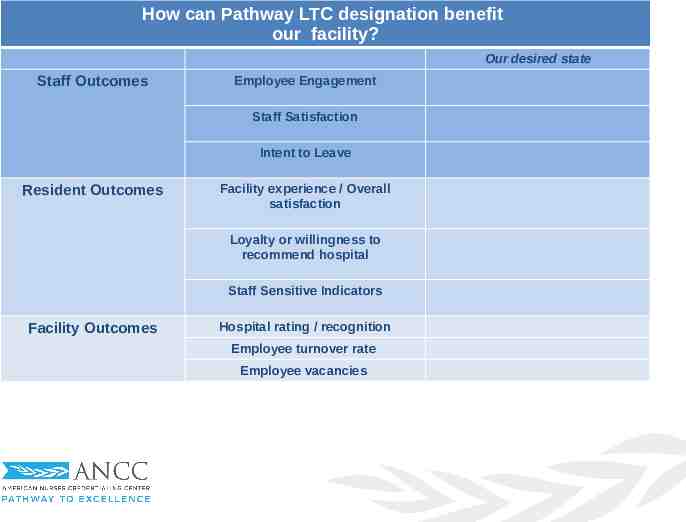
How can Pathway LTC designation benefit our facility? Our desired state Staff Outcomes Employee Engagement Staff Satisfaction Intent to Leave Resident Outcomes Facility experience / Overall satisfaction Loyalty or willingness to recommend hospital Staff Sensitive Indicators Facility Outcomes Hospital rating / recognition Employee turnover rate Employee vacancies
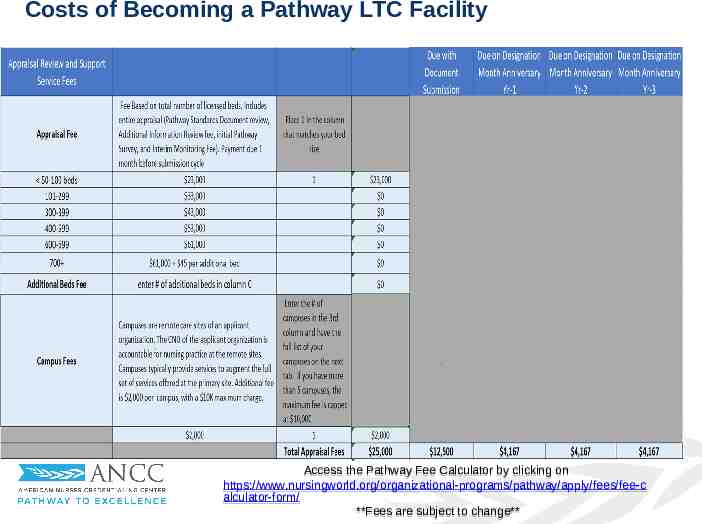
Costs of Becoming a Pathway LTC Facility Access the Pathway Fee Calculator by clicking on https://www.nursingworld.org/organizational-programs/pathway/apply/fees/fee-c alculator-form/ **Fees are subject to change**
Discussion and Questions
References 1. US Department of Health and Human Services. (2016). Long-term Care Providers and Services Users in the United States. National Center for Health Statistics: Vital and Health Statistics. Retrieved from Vital and Health Statistics, Series 3, Number 43 (cdc.gov) 2. Grabowski, D. C., Aschbrenner, K. A., Rome, V. F., & Bartels, S. J. (2010). Review: Quality of Mental Health Care for Nursing Home Residents: A Literature Review. Medical Care Research and Review, 67(6), 627-656. doi:10.1177/1077558710362538 3. White, E. M., Aiken, L. H., & McHugh, M. D. (2019). Registered nurse burnout, job dissatisfaction, and missed care in nursing homes. Journal of the American Geriatrics Society, 67(10), 2065-2071. 4. Boushey, H., & Glynn, S. J. (2012). There are significant business costs to replacing employees. Center for American Progress, 16, 1-9. 5. Salela, A. (2017). LTC worker shortage a 'train wreck waiting to happen,' expert says. Retrieved from https://www.mcknights.com/news/ltc-workershortage-a-train-wreck-waiting-to-happen-expert-says/ 2019 American Nurses Credentialing Center 18
References, cont. 6. Ross, J. (2018). Alarming trend in LTC: Overtime up 60% in 3 Years. Retrieved from https://www.mcknights.com/marketplace/ 7. Castle, N. G., & Ferguson-Rome, J. C. (2014). Influence of Nurse Aide Absenteeism on Nursing Home Quality. The Gerontologist, 55(4), 605-615. doi:10.1093/geront/gnt167 8. White, E., Woodford, E., Britton, J., Newberry, L., & Pabico, C. (2020). Nursing practice environment and care quality in nursing homes. Nursing Management, 51(6), 9-12. doi:10.1097/01.NUMA.0000662656.07901.a8 9. Aiken LH, Sermeus W, Van den Heede K, Sloane DM, Busse R, et al. (2012). Patient safety, satisfaction, and quality of hospital care: cross sectional surveys of nurses and residents in 12 countries in Europe and the United States. BMJ. 344:e1717. 10. McHugh MD, Kutney-Lee A, Cimiotti JP, Sloane DM, Aiken LH. (2011). Nurses’ widespread job dissatisfaction, burnout, and frustration with health benefits signal problems for resident care. Health Affairs. 30(2):202-210.

References, cont. 11. Kutney-Lee A, Germack H, Hatfield L, Kelly S., Maguire P, et al. (2016). Nurse engagement in shared governance and resident and nurse outcomes. J Nurs Admin. 46(11):605-612. 12. Mukamel, D. B., Spector, W. D., Limcangco, R., Wang, Y., Feng, Z., & Mor, V. (2009). The Costs of Turnover in Nursing Homes. Medical Care, 47(10), 1039-1045. doi:10.1097/mlr.0b013e3181a3cc62 13. Lake ET, Sanders J, Duan R, Riman KA, Schoenauer KM, Chen Y. (2019). A Meta-Analysis of the Associations Between the Nurse Work Environment in Hospitals and 4 Sets of Outcomes. Med Care. 57(5):353-361. doi: 10.1097/MLR.0000000000001109. 14. American Nurses Association. (2020). Testimonials and Case Studies. Retrieved from https://www.nursingworld.org//pathway/overview/ 15. Carroll, N. V., Delafuente, J. C., Cox, F. M., & Narayanan, S. (2008). FallRelated Hospitalization and Facility Costs Among Residents of Institutions Providing Long-Term Care. The Gerontologist, 48(2), 213-222. doi:10.1093/geront/48.2.213

References, cont. 16. NSI Nursing Solutions, Inc. (2020). National Healthcare Retention & RN Staffing Report; 2020. Accessed 07/17/20 at https://www.nsinursingsolutions.com/Documents/Library/NSI 17. Rau, J. (2019). Medicare Cuts Payments To Nursing Homes Whose Patients Keep Ending Up In Hospital. Retrieved from https://khn.org/news/medicare-cuts-payments-to-nursing-homes-whosepatients-keep-ending-up-in-hospital/ 18. Faris J. (2008). Lowering nursing injuries using post offer pre-employment testing. Work, 31(1), 39–45. 19. Press Ganey. (2019). Health Care Workforce Special Report: The State of Engagement (White Paper). Accessed 07/17/20 at https://www.pressganey.com/blog/press-ganey-releases-special-report-onstate-of-health-care-workforce-engagement
Learn More PATHWAY DESIGNATION https://www.nursingworld.org/organizational-programs/pathway/ Learn more 90-SECOND VIDEO OVERVIEW TO INTRODUCE NURSES TO PATHWAY TO EXCELLENCE https://youtu.be/aX8vH9F-3Sg?list PLCGdz-zkJ3hpwG9461zb4UAXPX2IZnv9f LONG TERM CARE RESOURCES https://www.nursingworld.org/organizational-programs/pathway/overview/pathway-to-excellence-inlong-term-care/ CASE STUDIES https://www.nursingworld.org/organizational-programs/pathway/overview/testimonials-and-case-stu dies/ PATHWAY TO EXCELLENCE PUBLICATIONS https://www.nursingworld.org/continuing-education/ce-subcategories/pathway/ A LITERATURE TABLE OF SELECTED RESEARCH STUDIES THAT HIGHLIGHT A FAVORABLE ASSOCIATION BETWEEN A VARIABLE WE INTERPRET TO BE CONSISTENT WITH A PATHWAY TO EXCELLENCE CHARACTERISTIC AND PATIENT, NURSE, OR ORGANIZATIONAL OUTCOMES https://www.nursingworld.org/organizational-programs/pathway/library-of-pathway-associated-conc epts/ 2020 American Nurses Credentialing Center 14