Long-Term Care: Infection Prevention Updates and Best Practices Carol
44 Slides1.04 MB
Long-Term Care: Infection Prevention Updates and Best Practices Carol Jamerson, RN, BSN, CIC Nurse Epidemiologist Virginia Department of Health Dottie Torrey, RN Regional Nurse Consultant American Healthcare
Objectives By the end of the presentation the attendees will better understand: The collaborative efforts in infection prevention with the Virginia Department of Health and long-term care facilities Updates in infection prevention specific to Norovirus, influenza vaccine, and the Tdap vaccine Available tools for best practices in long-term care for infection prevention addressing multidrug-resistant organisms, safe practices for blood glucose monitoring, and controlling disease outbreaks
Acknowledgments Virginia Department of Health - Healthcare-Associated Infections Team Andrea Alvarez, MPH - Coordinator Dana Burshell, MPH, CPH, CIC - Epidemiologist Virginia Health Care Association (VHCA) Judy Brown, RN, LNHA, Health Education Specialist Beverley Soble, Vice-President of Regulatory Affairs Eastern Virginia Medical School Robert M. Palmer, MD, MPH – John Franklin Chair of Geriatrics, Professor of Medicine and Director of the Glennan Center for Geriatrics and Geronotology Edward C. Oldfield, III – Professor of Medicine, Microbiology and Molecular Cell Biology, Director of Infectious Disease Division Collaborative partners from 12 nursing homes in Eastern Virginia
Successful Strategies for Infection Prevention in Assisted Living Facilities and Nursing Homes
Topics Covered Routes of disease transmission and chain of infection Standard and transmission-based precautions Hand hygiene and personal protective equipment Surveillance and outbreak investigation Environmental cleaning and disinfection Bloodborne pathogens, safe injection practices, and blood glucose monitoring Vaccination Staying home when sick (staff and visitors) Transfer of residents Working with your health department and licensing agency
Hot Topics Urinary tract infections Isolation of residents with multidrug-resistant organisms (MDROs) Tuberculosis Communication of information during transfer Environmental services
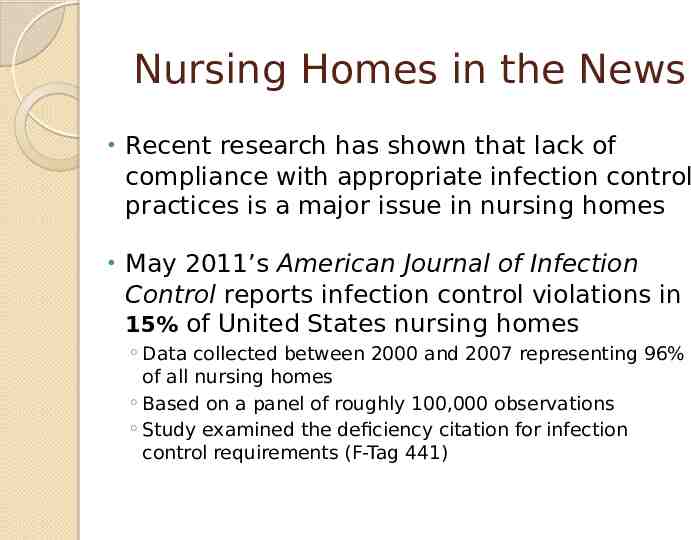
Nursing Homes in the News Recent research has shown that lack of compliance with appropriate infection control practices is a major issue in nursing homes May 2011’s American Journal of Infection Control reports infection control violations in 15% of United States nursing homes Data collected between 2000 and 2007 representing 96% of all nursing homes Based on a panel of roughly 100,000 observations Study examined the deficiency citation for infection control requirements (F-Tag 441)
Centers for Medicare and Medicaid Services (CMS) Federal Regulation F-Tag 441 states: “The facility must establish and maintain an infection control program designed to provide a safe, sanitary, and comfortable environment and to help prevent the development and transmission of disease and infection.”
Infections: A Leading Cause of Morbidity and Mortality Between 1.6 and 3.8 million infections occur each year in nursing homes with nearly 388,000 deaths attributed to these infections (1) Costs associated with infections in nursing homes are significant Estimates range from 673 million to 2 billion (1) Strong correlation between low staffing levels and the receipt of an infection control deficiency citation (1) AJIC May 2011, Vol. 39, p.263
CDC 12 Steps to Protect LTC Residents The CDC advocates that 4 basic groups of actions should be taken to prevent antimicrobial resistance in long-term care: Prevent infection Diagnose and treat infection effectively Use antimicrobials wisely Prevent transmission Most steps applicable to other healthcare settings as well CDC 12 Steps
A Little History About Antibiotic Use 2000 B.C. “Here, eat this root.” 1000 A.D. “That root is heathen. Here, say this prayer.” 1850 A.D. “That prayer is superstition. Here, drink this potion.” 1940 A.D. “That potion is snake oil. Here, take this penicillin; it’s a miracle drug.” 1985 A.D. “Penicillin is worthless. Here, take this new antibiotic; it’s bigger and better.” 2011 A.D. “Those antibiotics don’t work anymore. Here, eat this root.”
Multidrug Resistant Organisms (MDROs) The Alphabet Soup! Ingredients: MRSA; VRE; Multidrug Resistant Gram-Negative Rods (MDR- GNR) includes various organisms such as E. Coli, Klebsiella pneumoniae, Acinetobacter baumannii, Stenotrophomonas maltophilia and more . As a review: Colonization: Presence of a microorganism in or on the body without signs of symptoms of active infection. Active infection: Presence of microorganisms that are actively invading tissue and causing damage.
Important Points for MDRO Control Know your facility’s risk based on ongoing surveillance in order to note trends in transmission or infections Remember an outbreak maybe indicated by a higher incidence than usual in your facility population Work together with your microbiology laboratory and share trends with your medical director Develop effective policies and protocols and educate staff in implementation
MDRO Control (cont’d) Take action based on your findings Involve your key stakeholders Notify your local health department for advice and support Validate your environmental cleaning procedures and make adjustments as needed
Modes of Transmission The most common mechanism of transmission is via contact. Person to person Contaminated objects Hand hygiene is the keystone to infection prevention and control of transmission. Ensure that you have an effective hand hygiene program in place and monitor for compliance!

Patient Placement If possible, place resident in a private room If this option is not available, the resident should be cohorted with another resident with the same organism If neither option is possible, the resident should be placed in a room with another resident who is considered at low risk for acquistion of a MDRO. Examples include: no wounds, no invasive devices, not immunocomprised
Precautions Always standard precautions! Contact precautions may also be indicated. Consider the individual resident’s clinical situation and incidence of MDROs in your facility to determine when to implement and discontinue contact precautions. Practice what your facility’s policies reflect and remember to update policies based on your risk assessment!
Vaccinations and the Elderly In the elderly population, pneumonia and influenza are the fifth leading cause of death in the United States Residents who live in a long-term care facility may be at greater risk for serious infections due to age, decreased immunity, and/or underlying health conditions. Living in close quarters and having frequent contact with other residents may increase transmission risk.
Successful Vaccination Strategies Stress benefits of vaccination Allay fears and misconceptions Vaccines are safe! Cannot “catch” the disease from the vaccine Minimal side effects Benefits outweigh the risks Find creative ways to increase staff influenza vaccination rates Mobile flu carts Accommodate all shifts and weekdays/weekends Offer incentives for participation
Virginia Department of Health “Community Immunity” 2011-2012 Flu Theme
What is Community Immunity? “When a critical portion of a community is immunized against the flu, most members of the community are protected because there is little opportunity for the virus to spread.” For community immunity to work, each of us who can receive flu vaccine must get vaccinated every year Ultimately this will help protect all of
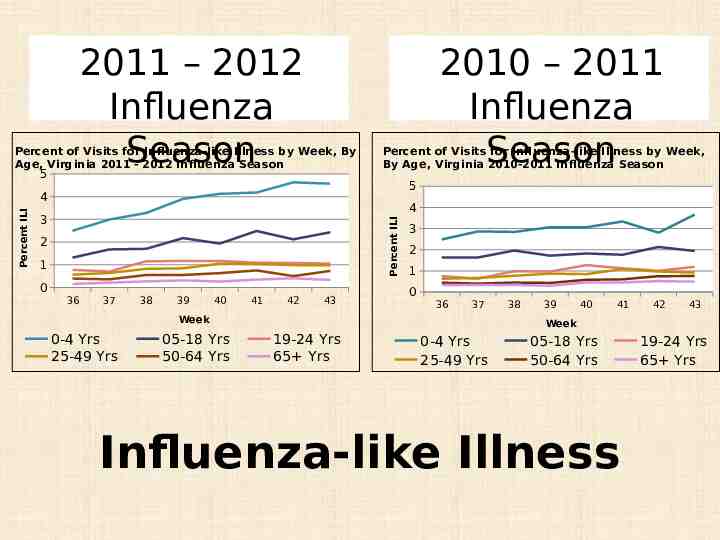
2011 – 2012 Influenza Season Percent of Visits for Influenza-like Illness by Week, By Age, Virginia 2011 - 2012 Influenza Season 5 2010 – 2011 Influenza Season Percent of Visits for Influenza-like Illness by Week, By Age, Virginia 2010-2011 Influenza Season 5 4 3 Percent ILI Percent ILI 4 2 1 0 36 37 38 39 40 41 42 43 3 2 1 0 36 37 Week 0-4 Yrs 25-49 Yrs 05-18 Yrs 50-64 Yrs 38 39 40 41 42 43 Week 19-24 Yrs 65 Yrs 0-4 Yrs 25-49 Yrs 05-18 Yrs 50-64 Yrs Influenza-like Illness 19-24 Yrs 65 Yrs
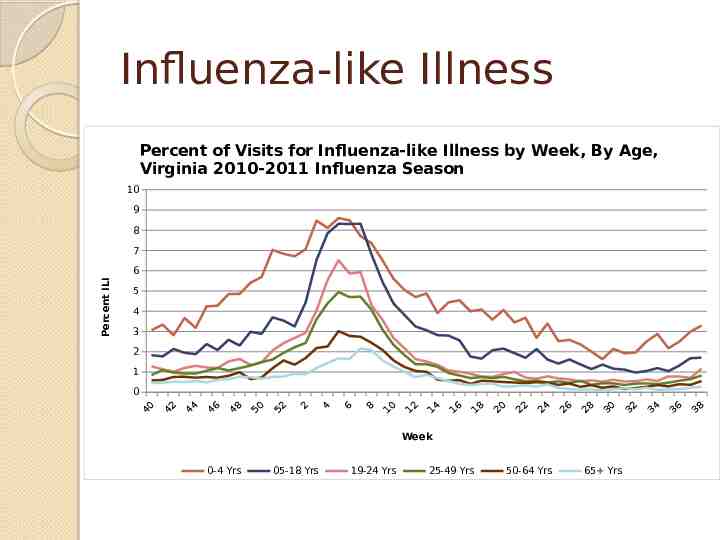
Influenza-like Illness Percent of Visits for Influenza-like Illness by Week, By Age, Virginia 2010-2011 Influenza Season 10 9 8 7 Percent ILI 6 5 4 3 2 1 0 40 42 44 46 48 50 52 2 4 6 8 10 12 14 16 18 20 22 24 26 28 30 Week 0-4 Yrs 05-18 Yrs 19-24 Yrs 25-49 Yrs 50-64 Yrs 65 Yrs 32 34 36 38
Changing Faces of Flu
Blood Glucose Monitoring Best Practices Fingerstick devices should never be used for more than one person Select single-use devices that permanently retract upon puncture Dedicate blood glucose meters to a single resident, one person, if possible If shared, the device should be cleaned and disinfected after every use, per manufacturer’s instructions Insulin pens and other medication cartridges and syringes are for single-use only and should never be used for more than oneBGMperson InService
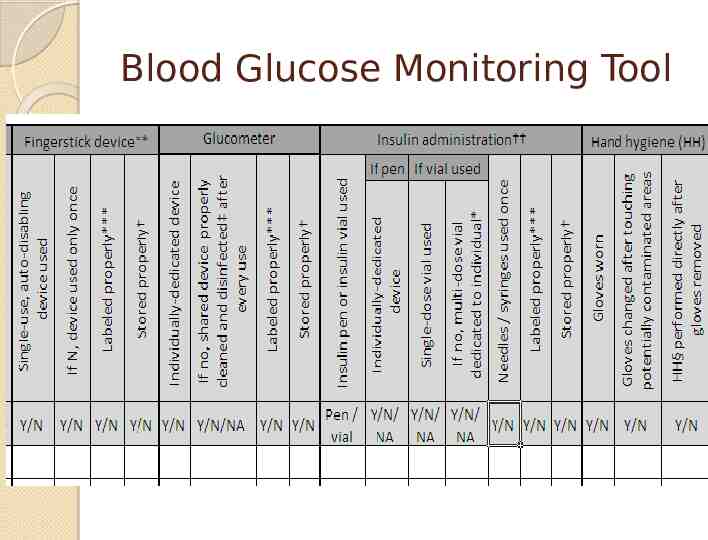
Blood Glucose Monitoring Tool
Norovirus -‘Tis the Season March 2011- Updated guidelines published in the Morbidity and Mortality Weekly Report (MMWR) o In the United States, approximately 21 million illnesses annually attributed to Norovirus o Transmission may be foodborne, waterborne, or by person to person o Indirect exposure may occur via fomites, contaminated environmental surfaces, or possibly via inhalation of aerosolized droplets from vomitus Please contact your local health department for assistance as soon as an outbreak is suspected!
Surveillance: Outbreak/Cluster Outbreak/cluster Occurs when there are more cases of a disease in a designated population than usually occur for a given period of time Every disease has an expected level of activity, or a “baseline” number of cases that occur over a given time period Surveillance helps identify outbreaks! Establish baseline and seasonal trends Identify commonalities among those who are sick Types of symptoms, area of the facility where they reside, etc. How to Identify an Outbreak
VDH Reporting Procedures Reportable conditions required by the Code of Virginia http://www.vdh.virginia.gov/ epidemiology/ regulations.htm Office of Licensure and Certification (OLC) reporting requirement Remember to contact your local health department for any outbreak concerns and advice!
Recommended Hand Hygiene for Norovirus Proper handwashing with soap and water - most effective way Hand sanitizers with 70% ethyl alcohol as adjunct in between proper handwashings but should not be considered a substitute for soap and water During suspected or confirmed outbreaks of Norovirus use soap and water!
Isolation Precautions and Sick Staff Members Sick patients/residents are recommended to be isolated until 2448 hours after symptoms resolve Sick patient care staff, food workers, and child–care staff should be excluded from work a minimum of 48 hours after symptoms resolve. Upon return to work, remind staff of importance for frequent hand hygiene.
Environmental Cleaning Proper cleaning and sanitizing of equipment, high traffic clinical areas, and frequently touched surfaces After initial cleaning of surfaces to remove visible soil, use a freshly made 10% chlorine bleach solution (i.e., 5,000 ppm sodium hypochlorite 1 cup bleach to 9 cups water) or other Environmental Protection Agency (EPA)-approved disinfectant o Note: all cleaning products and disinfectants should be EPA-registered and have labels claims for healthcare use o Change mop heads when a new bucket of cleaning solution is prepared, or after cleaning large spills of emesis or fecal material
Reminders Norovirus is highly contagious and very hardy, so strict adherence to control measures is necessary Successful Strategies for Infection Prevention in Assisted Living Facilities and Nursing Homes toolkit section with expanded information Complete guidelines are available on the Virginia Department of Health website: o http://www.vdh.virginia.gov/Epidemiology/ Surveillance/norovirus.htm
Pertussis (Whooping Cough) Vaccine preventable disease that causes severe coughing, vomiting, and complications possibly leading to pneumonia, and even death in infants Usually spread by coughing or sneezing while in close contact with others Protection from childhood vaccination fades over time thus the need for adults to be revaccinated On the rise throughout the United States, including Virginia 2010: CDC reported 27,550 cases in the U.S.
Tdap - What’s New for Healthcare Workers? The Advisory Committee on Immunization Practices (ACIP) Provisional Recommendations for Healthcare Personnel (HCP) on use of Tetanus toxoid, Reduced Diphtheria Toxoid and Acellular Pertussis Vaccine (Tdap) and the use of Postexposure Antimicrobial Prophylaxis - April 2011 CDC Morbidity and Mortality Weekly Report (MMWR) scheduled date of publication of recommendations for immunization of HCP – Fall 2011 Full pertussis-containing vaccine recommendations scheduled for 2012
Tdap in Healthcare Personnel The ACIP recommends that all HCP, regardless of age, should receive a single dose of Tdap as soon as feasible if they have not previously received Tdap and regardless of the time since last Td dose Expanded information is available by visiting: http://www.cdc.gov/vaccines/recs/ provisional/ default.htm
VDH/VHCA Urinary Tract Infection (UTI) Prevention Collaborative Selection of collaborative focus and region 12 participating nursing homes in the Eastern region June - December 2011 o Monthly conference calls o Surveillance from August – October Partnership with Eastern Virginia Medical School – The Glennan Center for Geriatrics and Gerontology
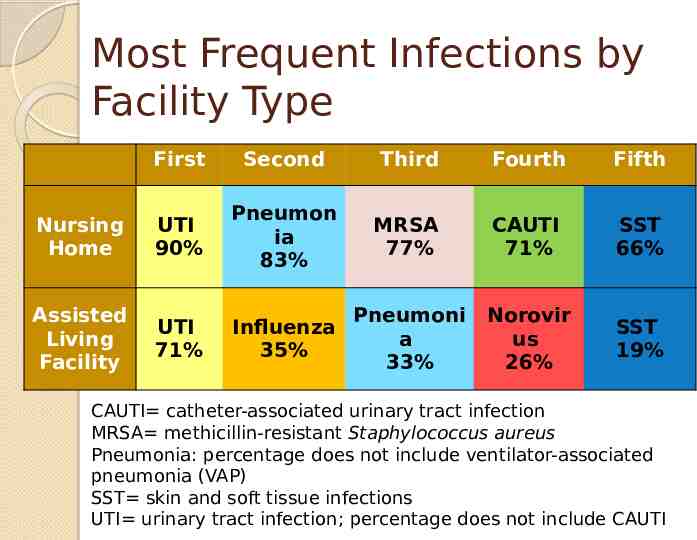
Most Frequent Infections by Facility Type First Second Third Fourth Fifth Nursing Home UTI 90% Pneumon ia 83% MRSA 77% CAUTI 71% SST 66% Assisted Living Facility UTI 71% Influenza 35% Pneumoni a 33% Norovir us 26% SST 19% CAUTI catheter-associated urinary tract infection MRSA methicillin-resistant Staphylococcus aureus Pneumonia: percentage does not include ventilator-associated pneumonia (VAP) SST skin and soft tissue infections UTI urinary tract infection; percentage does not include CAUTI

UTIs in the Long-Term Care Population As we have noted, UTIs are the most common bacterial infections encountered in older adults Diagnosis and treatment is often challenging as clinical manifestations are often atypical Assessment and delivery of information to the clinician is an important tool in determining if a symptomatic UTI is present
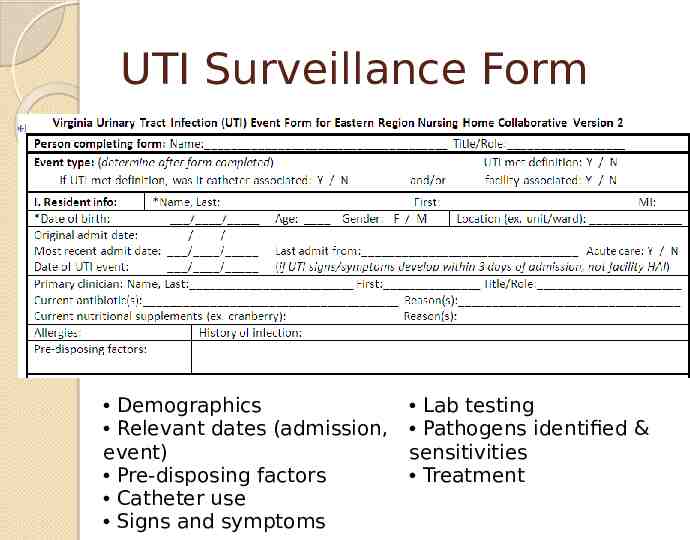
UTI Surveillance Form Demographics Relevant dates (admission, event) Pre-disposing factors Catheter use Signs and symptoms Lab testing Pathogens identified & sensitivities Treatment
Collaborative Activities and Sharing of Information UTI panel presentation - November 2nd Best practices for UTI prevention will be shared throughout Virginia via VDH website (currently being constructed) Anticipate publication of updated and validated revisions to the McGeer et al. (1991) definition set used by many long-term care facilities
Collaborative Wrap-Up Sharing and development of tools for best practices in UTI prevention (toolkit #2) o Surveillance tools o Guidelines for assessment o Education for staff, residents, and families Potential for sustaining/expanding project if grant funding approved
Thank You For All of Your Efforts in Infection Prevention ! VDH Healthcare-Associated Infections Team [email protected] [email protected] [email protected]
Questions?