Interprofessional Point-of-Care Documentation for Delirium Screening
28 Slides907.50 KB
Interprofessional Point-of-Care Documentation for Delirium Screening and Intervention: Integration of QSEN Competencies Heitman, L., Essner, A., Job, L. & Mueller, B. June 1, 2017
Goals To create a delirium policy and protocol for identification, documentation and initiation of an interprofessional approach to treat delirium and the risks it imposes for critically ill patients. To support this system change with the underlying quality and safety competencies: Patient-Centered Care Teamwork & Collaboration Evidence-Based Practice Quality Improvement Safety Informatics 2
Elements Early assessment for delirium Early documentation of findings Electronic consultations to interprofessional departments for prompt initiation of appropriate interventions Electronic process for data management to monitor findings and conduct ongoing evaluation of interventions 3
Clinical Issue Annual cost of ICU delirium in the U.S. is 4-6 billion Average costs for patients with delirium more than 2x the costs compared to patients without delirium Total costs estimates attributed to delirium range from 16,000- 64,000 per patient Leslie, Marcantonio, Zhang & Leo-Summers, 2008 Centers for Medicare & Medicaid Services (CMS) proposed delirium as one of 9 new conditions to be added to NonReimbursable Hospital Acquired Conditions. 4
Clinical Issue Delirium affects up to 80% of patients in Critical Care The longer ICU patients are delirious the higher the risk for: Increased morbidity Increased mortality Prolonged hospital stays *Guidelines recommend that critical care teams address delirium as a standard of care for all critically ill patients. (Pun, 2011, Justin, et.al, 2016) 5
Culture Change Historical approach: Long periods of immobility and bedrest to restore physiological stability Sedation, long-term ventilation & bedrest risk for delirium Current approach: ABCDE Bundle Awakening & Breathing Trial Coordination (Critical Care & RT) Careful sedation choices (Critical Care and Pharmacy) Delirium monitoring & documentation (Critical Care) Early exercise & mobility (PT) (Pun, 2011; Schweickert & Krees, 2011) 6
Delirium Team Key Clinical Leaders: Clinical Nurse Specialist: Coordinator of Delirium Project Cardiothoracic Clinical Nurse Specialist Critical Care Educator Project Leader: Clinical Information Systems Delirium policy and protocol development, development of nursing assessment in HIS (CAM-ICU Assessment Tool), staff education, monitoring of delirium assessment by Critical Care staff nurses, utilization of HIS products, Critical Care Sedation Policy revision, and implementation of Richmond Agitation Sedation Scale (RASS). 7
Delirium Team Clinical Liaisons: Respiratory Therapy Manager: Spontaneous Breathing Trials and ventilator weaning Physical Therapists: Early mobility Pharm.D.: Medication review Critical Care staff nurses: Delirium assessment and subsequent documentation Governance Structure: Chief Nursing Officer (Vice-President of Patient Care) Critical Care Director Critical Care Unit Patient Care Managers 8
Process Phase 1: Clinical Nurse Specialist: Reviewed scholarly evidence regarding delirium Consulted with members of the ICU Delirium & Cognitive Impairment Study Group, Vanderbilt Medical Center (delirium.org) Assembled a multidisciplinary team based upon evidence-based practice guidelines Phase 2: The Clinical Nurse Specialists and Critical Care Educator: Met with each committee member to discuss their role Phase 3: Reviewed current Policies and Procedures related to initiation of a new Delirium Policy (i.e. Critical Care Sedation policy, Spontaneous Breathing Trial policy) Delirium education presented to team members 9
Process Phase 4: Reviewed and implemented McKesson Clinical Solutions of HIS Conducted education of Critical Care staff Delirium Project initiated Clinical Nurse Specialists and Critical Care Educator received daily electronic reports of each positive delirium assessment Monthly progress reports were submitted to the Chief Nursing Officer (Vice-President for Patient Care) and Critical Care Director 10
IOM: Aims of Healthcare Improvement Safety CIT (Clinical Information Technology) provided clarity, accuracy and continuity for critically ill patients with delirium: Early assessment, documentation and interprofessional consultation minimized the risk of delirium RASS Sedation Scale Trauma Admission Orders Critical Care Sedation Orders Spontaneous Breathing Trial Coordination Consultation “Alerts” expedited appropriate interventions Client satisfaction: Brochure for patient & family education provided Delirium management communicated across the trajectory of care following ICU discharge 11
Overview: Clinical Solutions of HIS Utilized to implement the Delirium Policy and initiate interventions for delirium management. Each Clinical Solution helped to expedite clinical workflow by implementing evidence based interventions to promote quality patient care and minimize costs. 12
McKesson Clinical Solutions HORIZON EXPERT ORDERS Incorporation of RASS Sedation Scale Following adaptation of the RASS Sedation Scale for the newly introduced Delirium Screening Policy, the RASS score was incorporated into the Horizon Expert Orders for the: (1) Trauma Admission Orders and the (2) new Critical Care Sedation Orders to determine the sedation level for trauma patients and all patients requiring chemical sedation. HORIZON EXPERT DOCUMENTATION Newly created ICU Delirium Chartable Review (CRv) for Adult Nursing Assessment RASS Sedation Scale added to Adult Nursing Assessment under ICU Delirium Chartable Review (CRv) CAM-ICU Delirium Assessment Tool under ICU Delirium Chartable Review (CRv) Spontaneous Breathing Trial results under ICU Delirium Chartable Review (CRv) 13
McKesson Clinical Solutions HIS EXPERT DOCUMENTATION (cont.) Revised Nursing Interventions (NIC/NOC) added to Adult Nursing Assessment under ICU Delirium Chartable Review (CRv) and Plan of Care Chartable Review (CRv). *The preexisting Nursing Interventions required revision to adequately capture the current evidence-based interventions for delirium management HIS CARE ALERTS Automatic consults to Pharmacy, Respiratory Therapy and Physical Therapy for every positive delirium screen. Based upon the CAM-ICU (Delirium Screening Tool) results, automatic alerts are sent to each interdisciplinary consulting department. An email is forwarded to designated printers in each Intensive Care Unit. BUSINESS OBJECTS Daily automatic email reports of all delirium screens are sent to the Clinical Nurse Specialists and Critical Care Educator for evaluation. 14
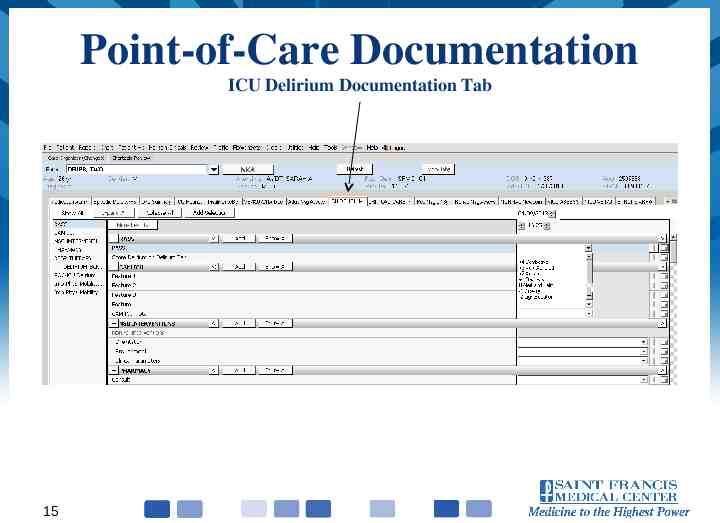
Point-of-Care Documentation ICU Delirium Documentation Tab 15
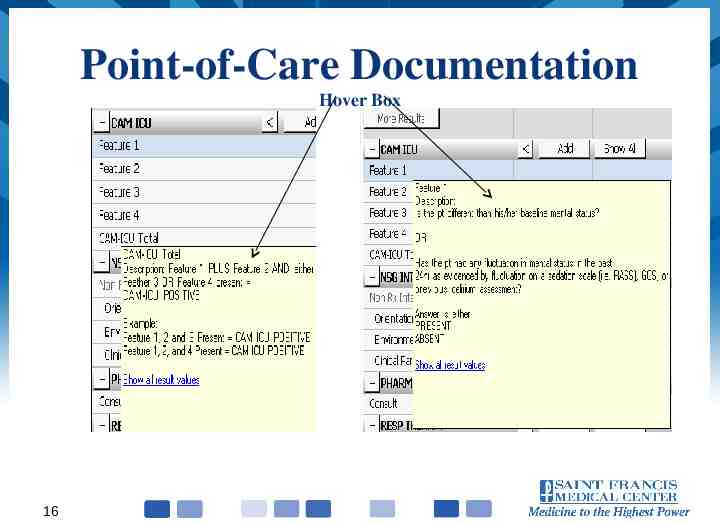
Point-of-Care Documentation Hover Box 16
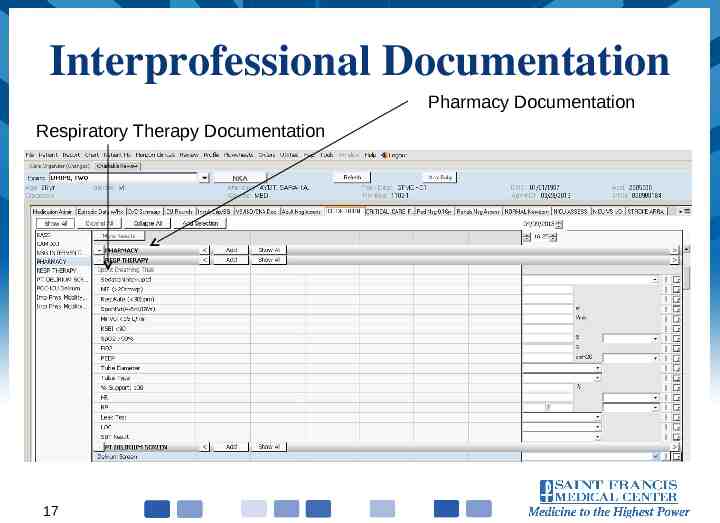
Interprofessional Documentation Pharmacy Documentation Respiratory Therapy Documentation 17
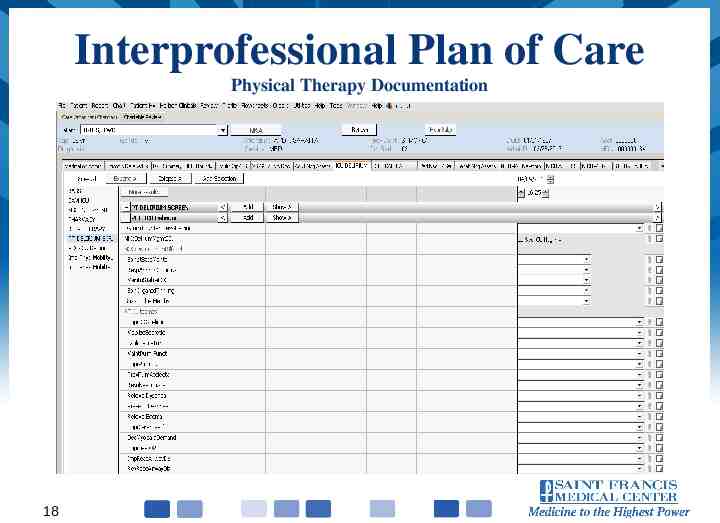
Interprofessional Plan of Care Physical Therapy Documentation 18
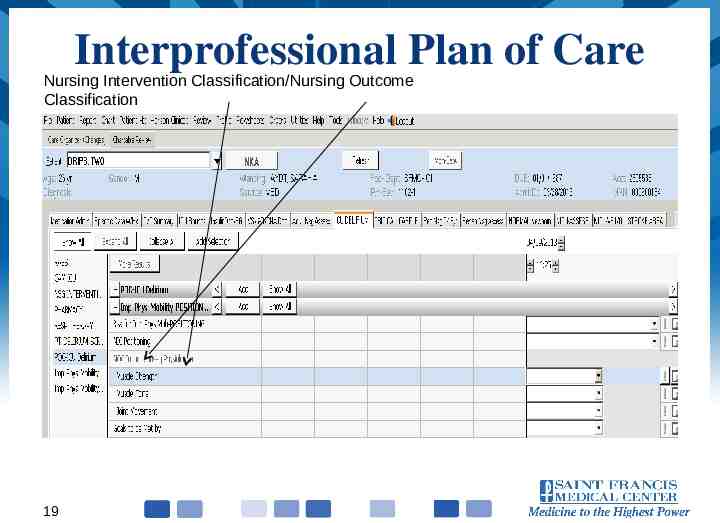
Interprofessional Plan of Care Nursing Intervention Classification/Nursing Outcome Classification 19
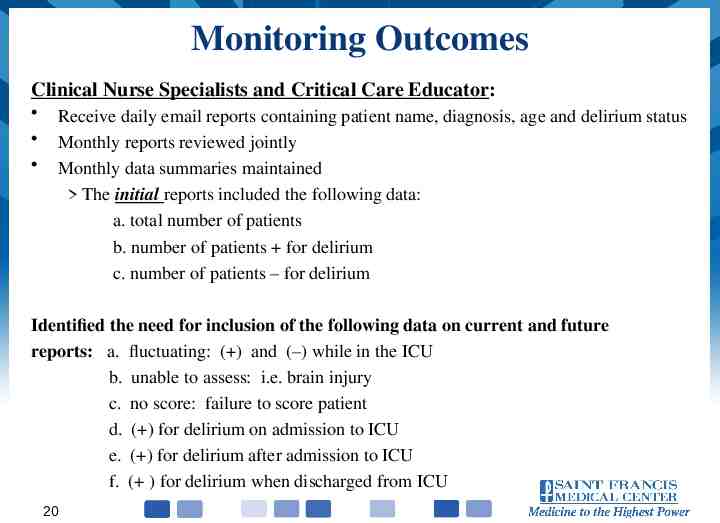
Monitoring Outcomes Clinical Nurse Specialists and Critical Care Educator: Receive daily email reports containing patient name, diagnosis, age and delirium status Monthly reports reviewed jointly Monthly data summaries maintained The initial reports included the following data: a. total number of patients b. number of patients for delirium c. number of patients – for delirium Identified the need for inclusion of the following data on current and future reports: a. fluctuating: ( ) and (–) while in the ICU b. unable to assess: i.e. brain injury c. no score: failure to score patient d. ( ) for delirium on admission to ICU e. ( ) for delirium after admission to ICU f. ( ) for delirium when discharged from ICU 20
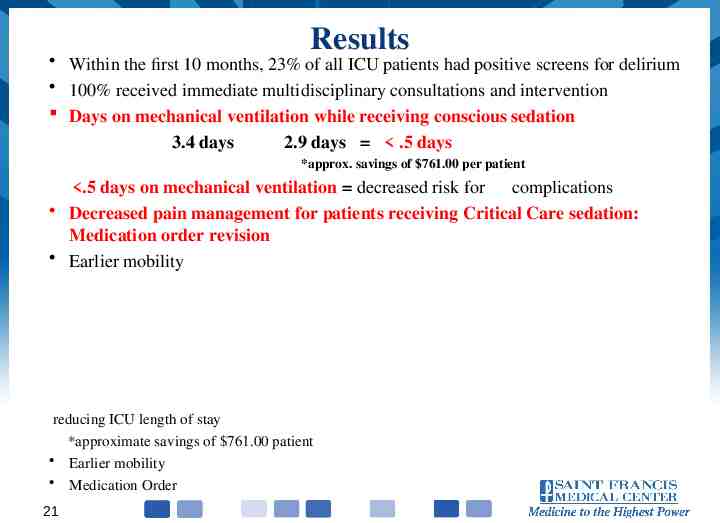
Results Within the first 10 months, 23% of all ICU patients had positive screens for delirium 100% received immediate multidisciplinary consultations and intervention Days on mechanical ventilation while receiving conscious sedation 3.4 days 2.9 days .5 days *approx. savings of 761.00 per patient .5 days on mechanical ventilation decreased risk for complications Decreased pain management for patients receiving Critical Care sedation: Medication order revision Earlier mobility reducing ICU length of stay *approximate savings of 761.00 patient Earlier mobility Medication Order 21
Implementation of Delirium Project Appoint an advanced practice nurse as coordinator of the project Establish an interprofessional team Provide delirium education for the Delirium Team and Critical Care Nursing staff Review existing institutional policies that increase the risk for delirium i.e. Critical Care Sedation, Spontaneous Breathing Trials, Mobility Orders for Critical Care Establish current Clinical Information Technology (CIT) capabilities to support the project 22
Implementation of Delirium Project Provide patient and advocate education materials regarding delirium Initiate daily rounding on all shifts, by Clinical Nurse Specialists and Critical Care Educator, with Critical Care nursing staff and interprofessional team to review, assist and confirm the presence of delirium and subsequent need for specific clinical interventions Share communication strategies for capturing more detailed information about delirium between team members and Critical Care nursing staff 23
Key Considerations to Apply Initiative Delirium affects every patient admitted to critical care. The project’s outcomes, and future development to identify the best interventional strategies for patients with delirium, will minimize the risk and long term complication it imposes. Quality of life can be improved for these patients while decreasing health care costs. The results should be replicable throughout all patient populations. Assessment tools, appropriate to each age group, must be implemented: Geriatric syndromes require ongoing, comprehensive physical, functional, and psychosocial assessments tailored to older adults. 24
Challenges Complexity of delirium Transitions to new health information systems Rapid turnover of Critical Care staff and interprofessional team requiring continual education Specificity of documentation to address clinical findings Transitional Care follow-up In the last 4 months the 192 patients that had delirium in the ICU: 49.6% had delirium upon admission to the ICU 25
Future Considerations Tracking of interprofessional consultations during ICU stay Outcomes during stay in ICU Outcomes following hospital discharge Cost analysis for trajectory of care Recommendation: Clinic follow-up visits at 3 and 6 months post hospital discharge for cognitive and functional evaluations 26
References Bell, L. (2013). Medications, delirium , and older adults. American Journal of Critical Care Nursing, 22(5), 444. Clinical practice guidelines for acute confusion and delirium. Agency for Healthcare Research and Quality, Retrieved September 5, 2012 from http://www.guideline.gov/content.aspx?id 14340%20 Clinical practice guidelines for management of pain, agitation and delirium in the intensive care unit. Critical Care Medicine Retrieved August 28, 2013, from: http://www.learnicu.org/SiteCollectionDocuments/Pain,%20Agitation,%20Delirium.pdf Dasta, J., McLaughlin, Mody, S., & Piech, C. (2005). Daily costs of intensive care unit day: the contribution of mechanical ventilation. Critical Care Medicine, 33(6), 1266-71. DiLibero, J., O’Donoghue, S.C., DeSanto-Madeya,S., & Felix, J. (2016). An innovative approach to improving the accuracy of delirium assessments using the confusion assessment method for the intensive care unit, Dimensions of Critical Care Nursing, 35(2), 74-80. (3), 163-173 Ely, E., Gautam, S., Margolin, R., Francis, J., May, L., Speroff, T., Truman, B., Dittus, R., Bernard, G. & Inouye, S. The impact of delirium in the intensive care unit on hospital length of stay. Intensive Care Medicine,(2001),27,1892-1900. Jablonski, J., Gray, J., Miano, T. , Redline, G., Teufel, H., Collins, T., Pascual-Lopez, J., Sylvia, M. & Niels, M. (2017). Pain, agitation, and delirium guidelines: Interprofessional perspectives to translate the evidence. Dimensions in Critical Care, 36(3), 163-173. . . 27
References Leslie, D., Marcantonio, E., Zhang, Y. Leo-Summers, L. & Inouye, S. (2008). One-year health care costs associated with delirium in the elderly population. Archives of Internal Medicine, 168 (1), 27-32. Louzon, P., Jennings, H., & Mahmood, A., & Kraisinger, M. (2017). Impact of pharmacist management of pain, agitation and delirium in the intensive care unit through participation in multidisciplinary bundle rounds. American Journal of Health Systems-Pharmacists, 74(4), 253-262. Perme, C. & Chandrashekar. R. (2009). Early mobility and walking program for patients in intensive care units: Creating a standard of care. American Journal of Critical Care, 18, 212221. Pun, B. & Boehm, L. (2011). Delirium in the intensive care unit. AACN Advanced Critical Care, 22, (3), 225-237 Reade, M.C. & Finfer, S. (2014). Sedation and delirium in the intensive care unit. New England Journal of Medicine, 370, 1-5. Schweickert, W.D. & Kress, J.P. (2011). Implementing early mobilization interventions in mechanically ventilated patients in the ICU. Chest, 140(6), 1612-1617. 28