Hot Topics in Pediatrics Patricia Farmer, DNP, APRN-CNP September
31 Slides6.32 MB

Hot Topics in Pediatrics Patricia Farmer, DNP, APRN-CNP September 24, 2021
Objectives At the completion of the presentation, the participant shall be able to: 1. Discuss criteria for returning to sports after COVID-19. 2. Discuss the Ten-4 Rule of Bruising 3. Identify at least two less common but "cannot afford to miss" diagnosis treated in pediatric primary care 4. Identify at least two references/sources for treatment of common pediatric diagnosis
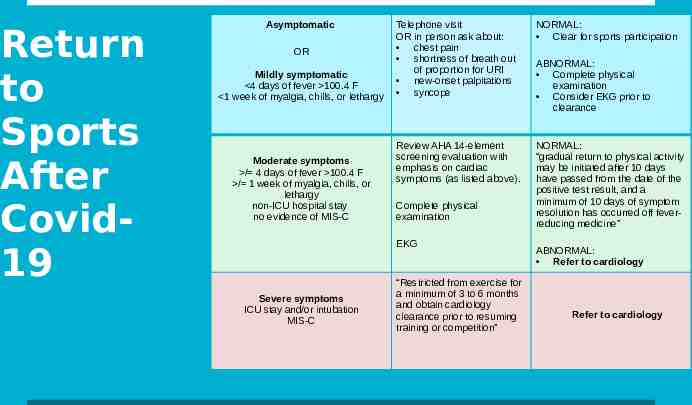
Return to Sports After Covid19 Asymptomatic OR Mildly symptomatic 4 days of fever 100.4 F 1 week of myalgia, chills, or lethargy Moderate symptoms / 4 days of fever 100.4 F / 1 week of myalgia, chills, or lethargy non-ICU hospital stay no evidence of MIS-C Telephone visit OR in person ask about: chest pain shortness of breath out of proportion for URI new-onset palpitations syncope NORMAL: Clear for sports participation Review AHA 14-element screening evaluation with emphasis on cardiac symptoms (as listed above). NORMAL: “gradual return to physical activity may be initiated after 10 days have passed from the date of the positive test result, and a minimum of 10 days of symptom resolution has occurred off feverreducing medicine” Complete physical examination EKG Severe symptoms ICU stay and/or intubation MIS-C “Restricted from exercise for a minimum of 3 to 6 months and obtain cardiology clearance prior to resuming training or competition” ABNORMAL: Complete physical examination Consider EKG prior to clearance ABNORMAL: Refer to cardiology Refer to cardiology
Multisystem Inflammatory Syndrome-Children (MIS-C) 21 yrs of age with fever, lab indicated inflammation, requires hospitalization with organ involvement of 2 organs AND no other plausible dx AND Positive for current or recent SARS-CoV-2 infection by PCR, serology or antigen test or exposure to COVID-19 in the previous 4 weeks Reported or known fever of 38.0 C (100.4 F) Do not know the causes Inflammation of heart, lungs, brain, kidneys, eyes, skin or GI organs Can be life threatening Can fully or partially meet criteria for Kawasaki Disease
MIS-C Treatment: Antibiotics, Steroids, IVIG Reportable illness Close follow up Peds cardiology and possible activity restriction, if myocardial injury Peds rheumatologist for those that received steroid s or biologics Primary care As of July 25, 2021: 4404 cases and 37 deaths Median age was 9 yrs, ranging 5-13 yrs 63% were Hispanic/Latino or Black, Non-Hispanic 99% were test positive 60% were male FYI: There is a MIS-Adult (CDC.gov)
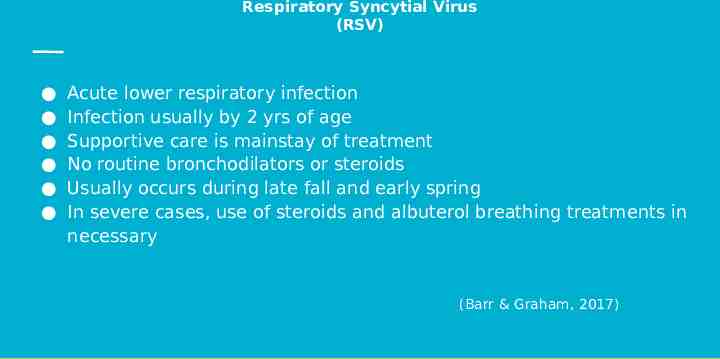
Respiratory Syncytial Virus (RSV) Acute lower respiratory infection Infection usually by 2 yrs of age Supportive care is mainstay of treatment No routine bronchodilators or steroids Usually occurs during late fall and early spring In severe cases, use of steroids and albuterol breathing treatments in necessary (Barr & Graham, 2017)
Pediatric Hospital Bed Shortage Pediatric patients are being sent out of state: TX, Little Rock, Memphis, St Louis, Kansas City, Wichita, etc. Nursing shortage and RSV and primary reasons COVID-19 has been an influence Pregnancy and COVID-19
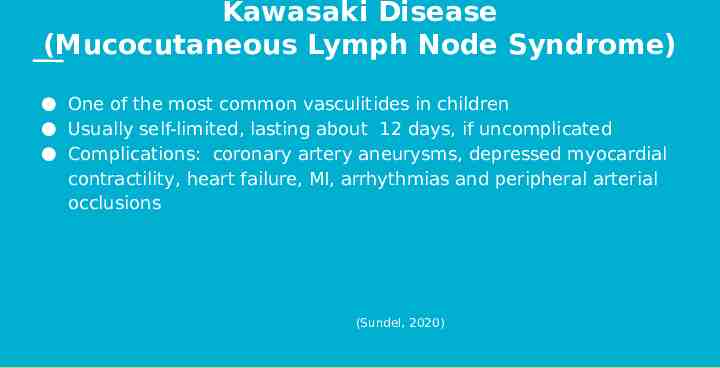
Kawasaki Disease (Mucocutaneous Lymph Node Syndrome) One of the most common vasculitides in children Usually self-limited, lasting about 12 days, if uncomplicated Complications: coronary artery aneurysms, depressed myocardial contractility, heart failure, MI, arrhythmias and peripheral arterial occlusions (Sundel, 2020)
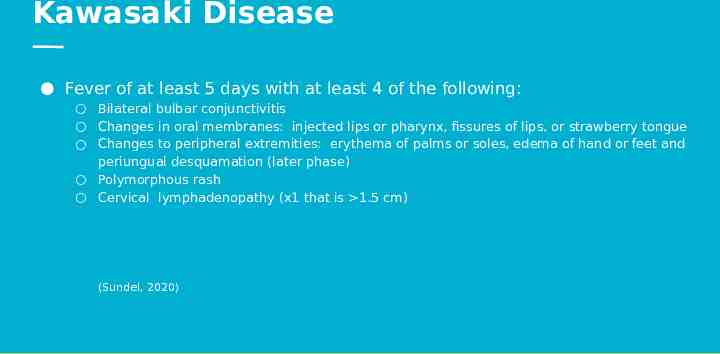
Kawasaki Disease Fever of at least 5 days with at least 4 of the following: Bilateral bulbar conjunctivitis Changes in oral membranes: injected lips or pharynx, fissures of lips, or strawberry tongue Changes to peripheral extremities: erythema of palms or soles, edema of hand or feet and periungual desquamation (later phase) Polymorphous rash Cervical lymphadenopathy (x1 that is 1.5 cm) (Sundel, 2020)
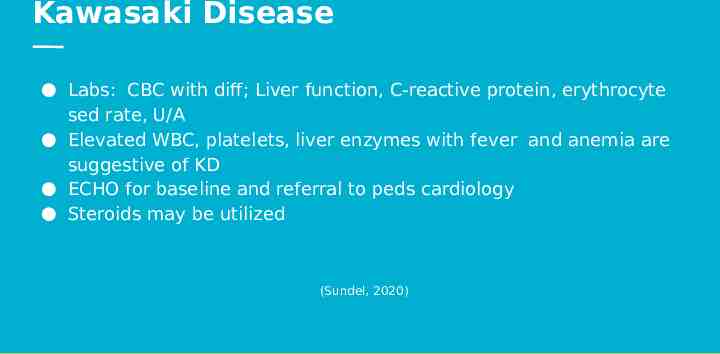
Kawasaki Disease Labs: CBC with diff; Liver function, C-reactive protein, erythrocyte sed rate, U/A Elevated WBC, platelets, liver enzymes with fever and anemia are suggestive of KD ECHO for baseline and referral to peds cardiology Steroids may be utilized (Sundel, 2020)
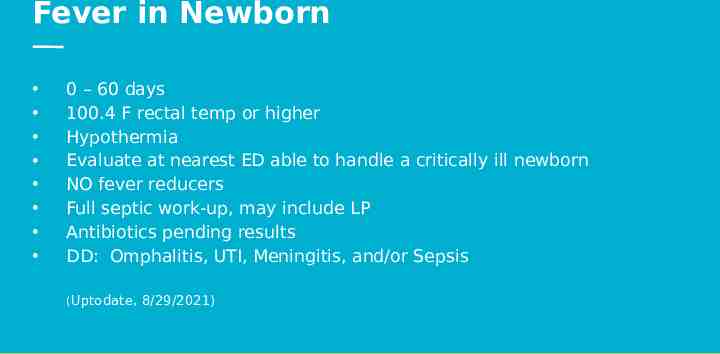
Fever in Newborn 0 – 60 days 100.4 F rectal temp or higher Hypothermia Evaluate at nearest ED able to handle a critically ill newborn NO fever reducers Full septic work-up, may include LP Antibiotics pending results DD: Omphalitis, UTI, Meningitis, and/or Sepsis (Uptodate, 8/29/2021)
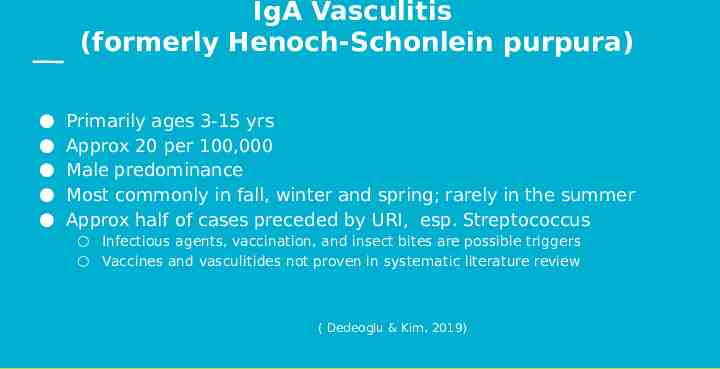
IgA Vasculitis (formerly Henoch-Schonlein purpura) Primarily ages 3-15 yrs Approx 20 per 100,000 Male predominance Most commonly in fall, winter and spring; rarely in the summer Approx half of cases preceded by URI, esp. Streptococcus Infectious agents, vaccination, and insect bites are possible triggers Vaccines and vasculitides not proven in systematic literature review ( Dedeoglu & Kim, 2019)
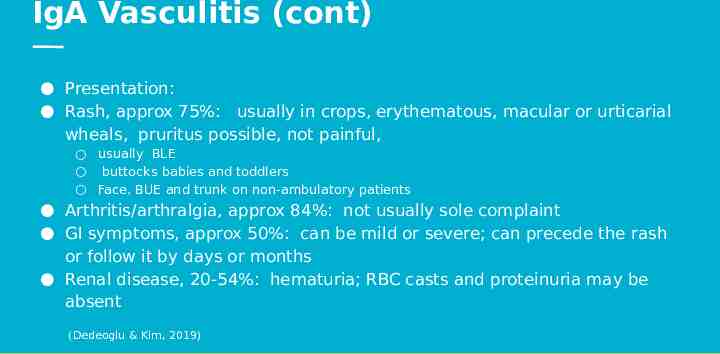
IgA Vasculitis (cont) Presentation: Rash, approx 75%: usually in crops, erythematous, macular or urticarial wheals, pruritus possible, not painful, usually BLE buttocks babies and toddlers Face, BUE and trunk on non-ambulatory patients Arthritis/arthralgia, approx 84%: not usually sole complaint GI symptoms, approx 50%: can be mild or severe; can precede the rash or follow it by days or months Renal disease, 20-54%: hematuria; RBC casts and proteinuria may be absent (Dedeoglu & Kim, 2019)
IgA Vasculitis (cont) Diagnosis: Easy with palpable purpura of LE and combination of 2 or more typical findings Rash may be late developing in 25% of cases See Case Report CBC, CMP and U/A: nonspecific Leukocytosis: 20,000 cell/mm3, if a recent bacterial infection PT, PTT, PLT are usually all WNL U/A initially WNL Biopsy of affected organ, if unusual presentation Imaging of affected areas (Dedeoglu & Kim, 2019)
6 yr old male presentation Male seen by PCP for headache and abdominal pain Negative for COVID-19 and Strep Throat Instructed on symptomatic care and given instructions for emergent care 4 days later, returned to PCP for increased abdominal pain with N/V and fatigue Sent to Pediatric ER from PCP office Pediatric ER: diagnosed with severe constipation AND developed purpura during the ER stay Urine was WNL Will need U/A weekly x2 months and monthly x4 more months
15 yr old female presentation Presented to PCP office with CC of “rash” CBC, CMP, and U/A: WNL Abdominal U/S: WNL Pharyngitis: negative COVID-19: negative U/A and B/P followed weekly x2 mos and monthly x4 mos Developed UTI x1 approx 4 mos after dx but was thought to be a hygiene and urine holding issue No other concerns noted
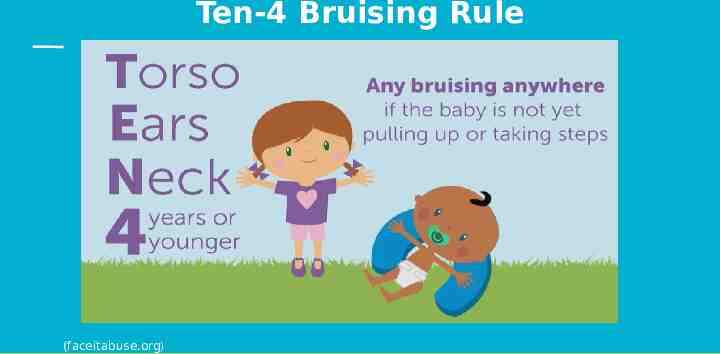
Ten-4 Bruising Rule (faceitabuse.org)
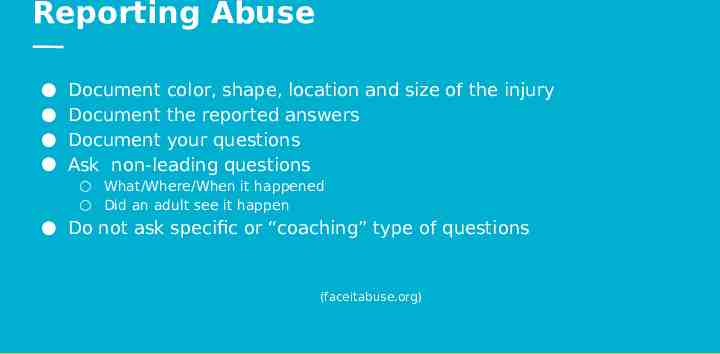
Reporting Abuse Document color, shape, location and size of the injury Document the reported answers Document your questions Ask non-leading questions What/Where/When it happened Did an adult see it happen Do not ask specific or “coaching” type of questions (faceitabuse.org)
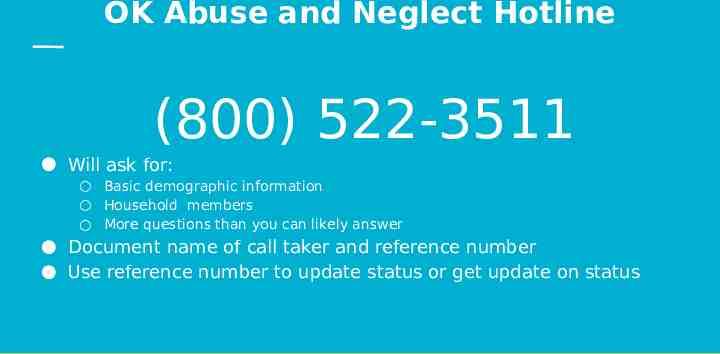
OK Abuse and Neglect Hotline (800) 522-3511 Will ask for: Basic demographic information Household members More questions than you can likely answer Document name of call taker and reference number Use reference number to update status or get update on status
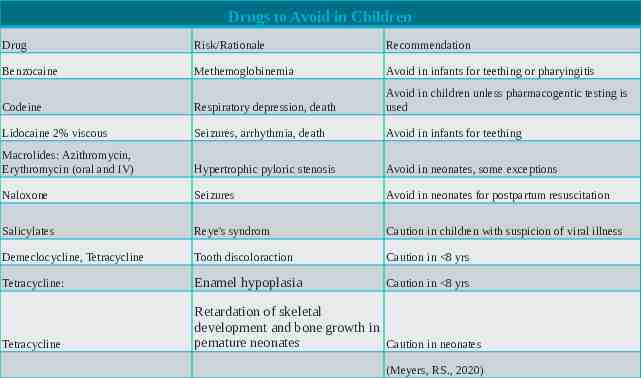
Drugs to Avoid in Children Drug Risk/Rationale Recommendation Benzocaine Methemoglobinemia Avoid in infants for teething or pharyingitis Codeine Respiratory depression, death Avoid in children unless pharmacogentic testing is used Lidocaine 2% viscous Seizures, arrhythmia, death Avoid in infants for teething Macrolides: Azithromycin, Erythromycin (oral and IV) Hypertrophic pyloric stenosis Avoid in neonates, some exceptions Naloxone Seizures Avoid in neonates for postpartum resuscitation Salicylates Reye's syndrom Caution in children with suspicion of viral illness Demeclocycline, Tetracycline Tooth discoloraction Caution in 8 yrs Tetracycline: Enamel hypoplasia Caution in 8 yrs Tetracycline Retardation of skeletal development and bone growth in pemature neonates Caution in neonates (Meyers, RS., 2020)
Beware of Zebras (discoverwildlife.com)
Anorectal Malformation (Imperforate Anus) Many facilities are no longer doing rectal temperatures Stooling should occur in first 24 hrs Many infants are being discharged at 24 hrs of age
Case Report: Anorectal Malformation 4 day old female presented to PCP 33 wk gestation Weight down 8% Temp 96.3 F, TA due to unable to pass rectal thermometer Admitted to NICU Colostomy placed at 5 days of age
Case Report: Anorectal Malformation 16 day old female presented to PCP office for initial visit History of hospital admission for projectile vomiting, concern for obstruction, malrotation vs. volvulus Dx: Ectopic anus (partial imperforate anus) and Reflux Treatment: rectal dilation but no surgery planned
Case Report: Neuroblastoma 7 mo old female dx with AOM, crying loudly during exam WCC at 6 mos of age, no concerns Returned 5 days later for a diaper Right upper abdominal on exam Infant happy, quiet Abdominal U/S with 5 cm mass to left kidney, metastatic disease Approx 15 mos at St. Jude Doing well Take away: Do the exam the same way every time to keep the quality that we desire
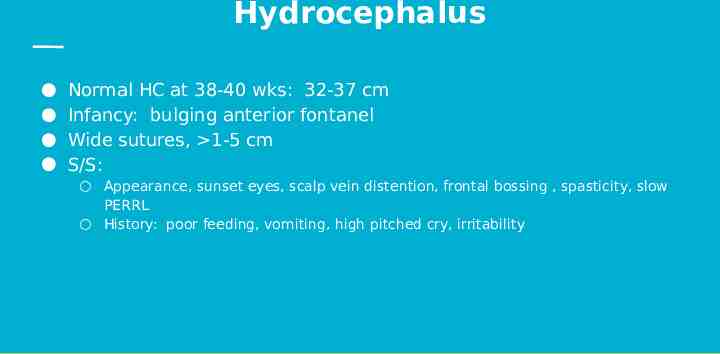
Hydrocephalus Normal HC at 38-40 wks: 32-37 cm Infancy: bulging anterior fontanel Wide sutures, 1-5 cm S/S: Appearance, sunset eyes, scalp vein distention, frontal bossing , spasticity, slow PERRL History: poor feeding, vomiting, high pitched cry, irritability
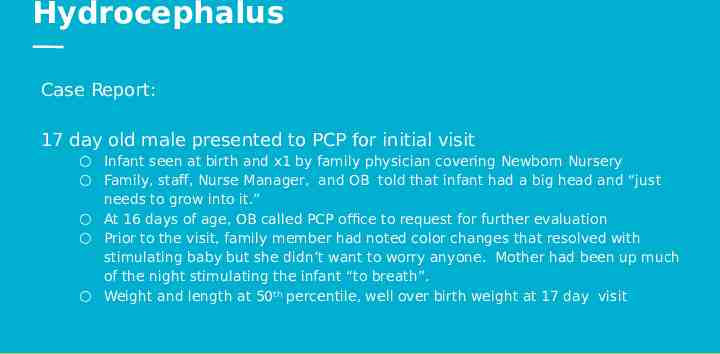
Hydrocephalus Case Report: 17 day old male presented to PCP for initial visit Infant seen at birth and x1 by family physician covering Newborn Nursery Family, staff, Nurse Manager, and OB told that infant had a big head and “just needs to grow into it.” At 16 days of age, OB called PCP office to request for further evaluation Prior to the visit, family member had noted color changes that resolved with stimulating baby but she didn’t want to worry anyone. Mother had been up much of the night stimulating the infant “to breath”. Weight and length at 50th percentile, well over birth weight at 17 day visit
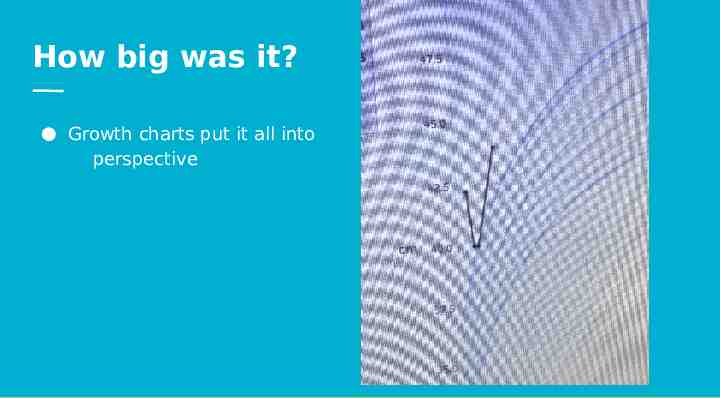
How big was it? Growth charts put it all into perspective
References American Academy of Pediatrics, (n.d.) MIS-C. American Academy of Pediatrics. https://www.aap.org/en/pages/201l-novel-coronavirus-covid-19-invections/clinical -guidance/multisystem-inflammatory-syndrome-in-children-mis-c-interim-guidanc e/ Centers for Disease Control and Prevention, (n.d.) MIS-c. Centers for Disease Control and prevention. https://www.cdc.gov/mis/hcp Centers for Disease Control and Prevention. (n.d.). Coronavirus disease 2019 (COVID-19). Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/index.html.
References Dedeoglu, F., & Kim, S. (2019, November 1). IgA vasculitis (HenochSchönlein purpura): Clinical manifestations and diagnosis. UpToDate. https://www.uptodate.com/home. Meyers, RS. J Pediatric Pharmacol Therapies, 2020; 25(3): 175-191 Ten-4 Bruising Rule. Face It. (2021, August 23). https://faceitabuse.org/. Scarfone, R. J., & Cho, C. S. (n.d.). Approach to the ill appearing infant younger than 90 days of age. UpToDate. https://www.uptodate.com/home. Sundel, R. (2020, June 29). Evidence-based clinical decision support Kawasaki disease: Clinical features and diagnosis. UpToDate. https://www.uptodate.com/home.

Thank you and see you later.