Evidence-Based Practice in Clinical Psychology: What It Is, Why It
54 Slides2.40 MB
Evidence-Based Practice in Clinical Psychology: What It Is, Why It Matters, What You Need to Know Bonnie Spring, Ph.D., ABPP Northwestern University
Why it matters: EBBP Rationale improve quality and accountability for health care practice (IOM, 2001, Crossing the Quality Chasm) shared vocabulary and concepts for transdisciplinary, biopsychosocial research, practice, health care policy stimulate development of evidence base for behavioral treatments
Why it matters: Potentionally Useful Infrastructure Clinical Practice Guidelines: Increasingly based on ongoing systematic review of research (esp. RCTs) (e.g., USPTF, Cochrane, CDC/AHRQ) Research reporting guidelines (CONSORT, TREND, QUOROM) Evidence grading & knowledge synthesis systems (e.g., GRADE, AHRQ) Policy, often coverage/reimbursement implications (VA/DOD, CMS, NICE) (P4P?) Evidence-Based Practice: (life-long learning) Question formulation, search strategies, critical appraisal SUMSEARCH Clinical Evidence, First Consult, BMJ updates, Best Evidence Topics, CATCRAWLER, CATBANK – clinical scenario & bottom line
Overview History of evidence-based practice (EBP) Core elements of EBP EBP pedagogy in psychology EBP pedagogy in other health disciplines Useful infrastructure and potential opportunities for synergy
Origins of Evidence-Based Practice
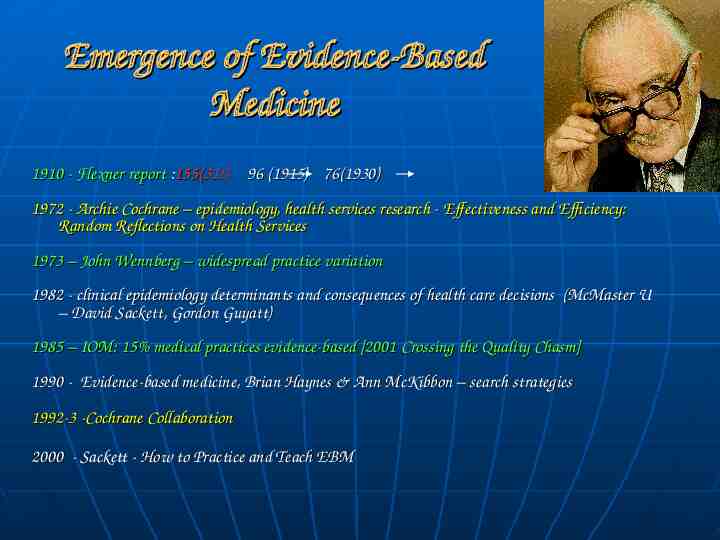
Emergence of Evidence-Based Medicine 1910 - Flexner report :155(31!) 96 (1915) 76(1930) 1972 - Archie Cochrane – epidemiology, health services research - Effectiveness and Efficiency: Random Reflections on Health Services 1973 – John Wennberg – widespread practice variation 1982 - clinical epidemiology determinants and consequences of health care decisions (McMaster U – David Sackett, Gordon Guyatt) 1985 – IOM: 15% medical practices evidence-based [2001 Crossing the Quality Chasm] 1990 - Evidence-based medicine, Brian Haynes & Ann McKibbon – search strategies 1992-3 -Cochrane Collaboration 2000 - Sackett - How to Practice and Teach EBM
What do we mean by “evidence-based practice?”
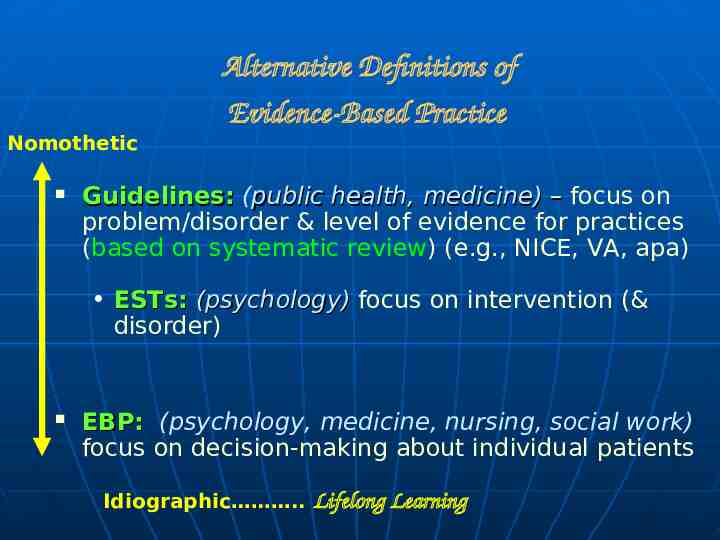
Nomothetic Alternative Definitions of Evidence-Based Practice Guidelines: (public health, medicine) – focus on problem/disorder & level of evidence for practices (based on systematic review) (e.g., NICE, VA, apa) ESTs: (psychology) focus on intervention (& disorder) EBP: (psychology, medicine, nursing, social work) focus on decision-making about individual patients Idiographic . Lifelong Learning
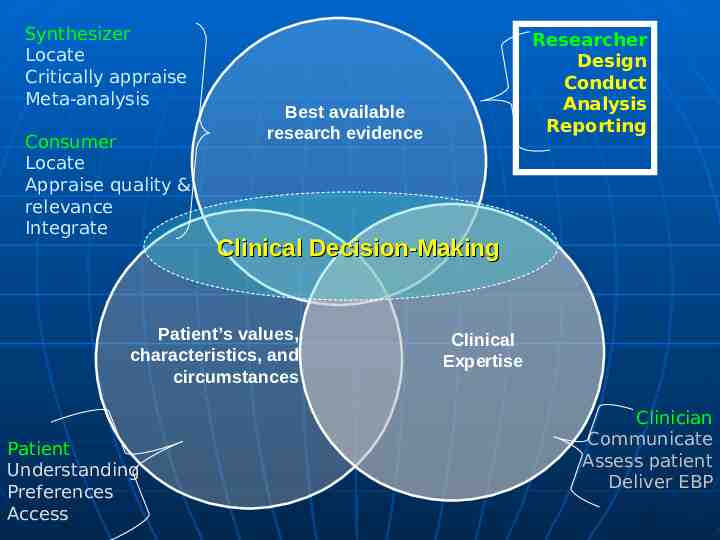
APA Policy Statement adopted August 2005 “Evidence-based practice in psychology is the integration of the best available research with clinical expertise in the context of patient characteristics, culture, and preferences.” -adapted from IOM, 2001 & Sackett, 2000
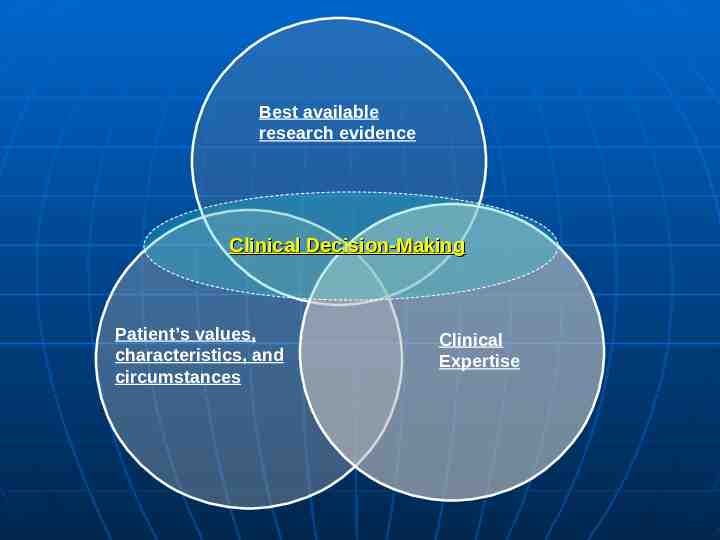
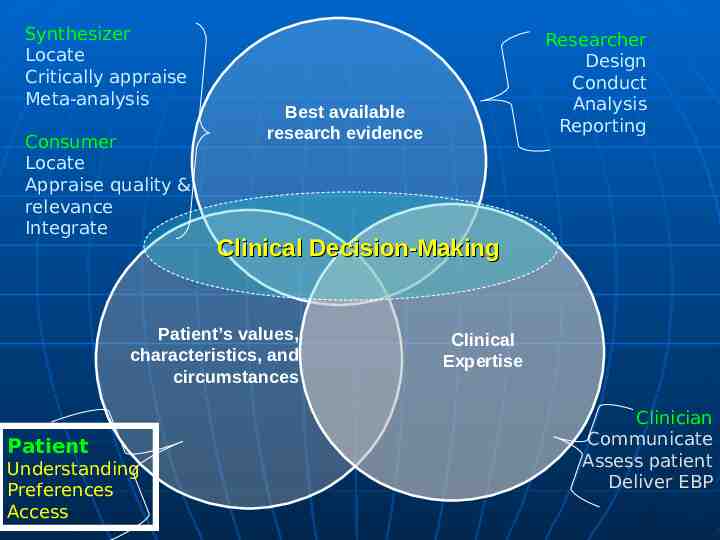
Best available research evidence Clinical Decision-Making Patient’s values, characteristics, and circumstances Clinical Expertise
Syllabus Project Prompt: Does anyone on the list teach a course on evidencebased practice (EBP)? Specifically, I am searching for syllabi that cover one or more "legs" of the three-legged EBP stool: a) research evidence, b) clinical expertise, c) patient values, preferences, characteristics. November, 2006
Listservs Sampled ABCT APA Division 12 SSCPNET (Section III, Div 12) CUDCP APA Division 38 ABMR SBM EBBM, MRBC, Obesity, CA SIGs
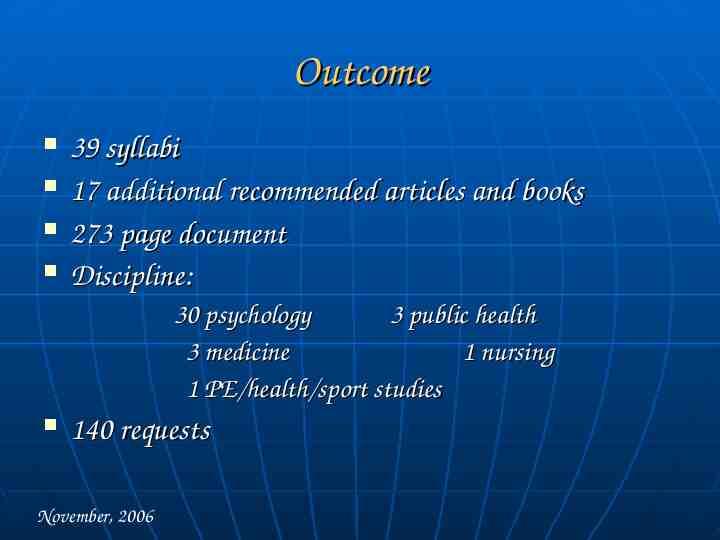
Outcome 39 syllabi 17 additional recommended articles and books 273 page document Discipline: 30 psychology 3 public health 3 medicine 1 nursing 1 PE/health/sport studies 140 requests November, 2006
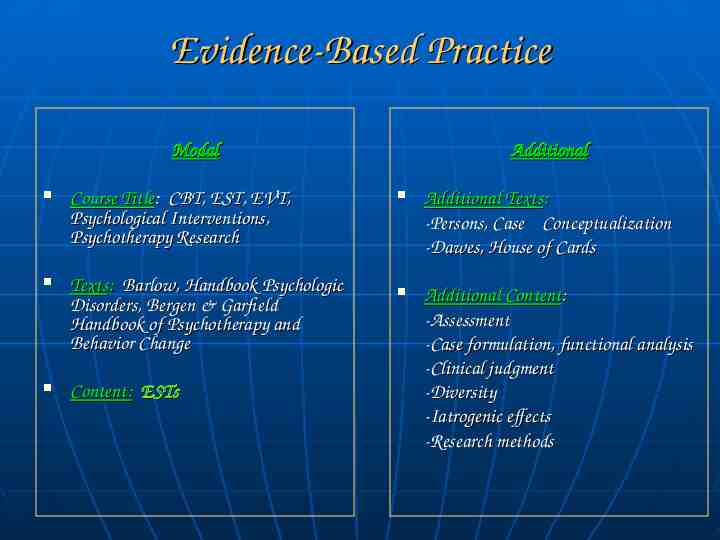
Evidence-Based Practice Modal Course Title: CBT, EST, EVT, Psychological Interventions, Psychotherapy Research Texts: Barlow, Handbook Psychologic Disorders, Bergen & Garfield Handbook of Psychotherapy and Behavior Change Content: ESTs Additional Additional Texts: -Persons, Case Conceptualization -Dawes, House of Cards Additional Content: -Assessment -Case formulation, functional analysis -Clinical judgment -Diversity -Iatrogenic effects -Research methods
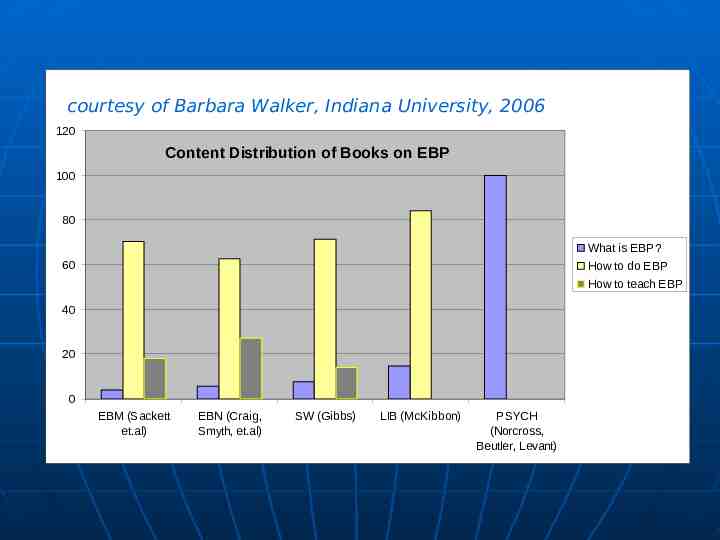
courtesy of Barbara Walker, Indiana University, 2006 120 Content Distribution of Books on EBP 100 80 What is EBP? 60 How to do EBP How to teach EBP 40 20 0 EBM (Sackett et.al) EBN (Craig, Smyth, et.al) SW (Gibbs) LIB (McKibbon) PSYCH (Norcross, Beutler, Levant)
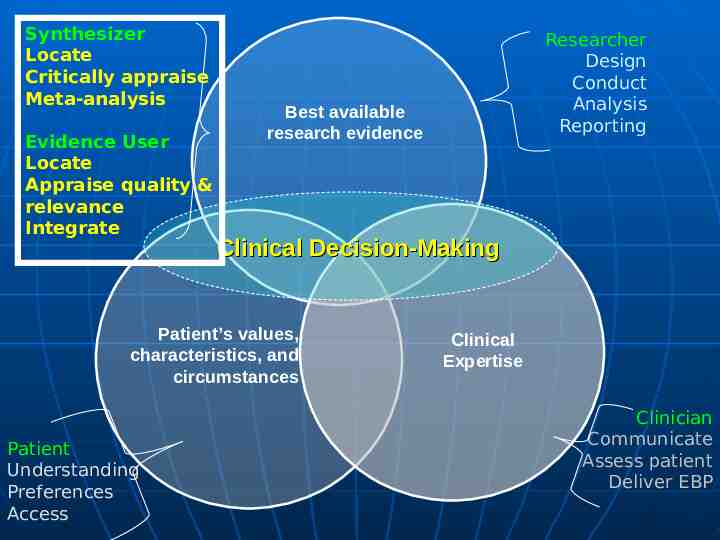
Synthesizer Locate Critically appraise Meta-analysis Consumer Locate Appraise quality & relevance Integrate Best available research evidence Clinical Decision-Making Patient’s values, characteristics, and circumstances Patient Understanding Preferences Access Researcher Design Conduct Analysis Reporting Clinical Expertise Clinician Communicate Assess patient Deliver EBP
Researcher Training in Psychology versus Medicine Psychology Design Correlational (convenience classes) Experimental (from animal studies) Conduct Brief, tight control Little missing data; replace cases Analysis - completer Reporting Clinical Medicine Design Observational (population) Clinical Trial –test – of policy applied to population Conduct Long, intercurrent events Missing data; Analysis – ITT Reporting – CONSORT
Researcher, Synthesizer, Consumer Training in Analysis Psychology ANOVA/regression Clinical Medicine Odds Ratios Epidemiology Terminology Absolute risk (p[disease] in a particular population) Relative risk (p[disease/exposed]/p[disease/unexposed) Attributable risk (p[disease/exposed] -p[disease/unexposed) Number needed to harm (1/attributable risk) Odds ratio (odds[disease/exposed]/odds[disease/unexposed])

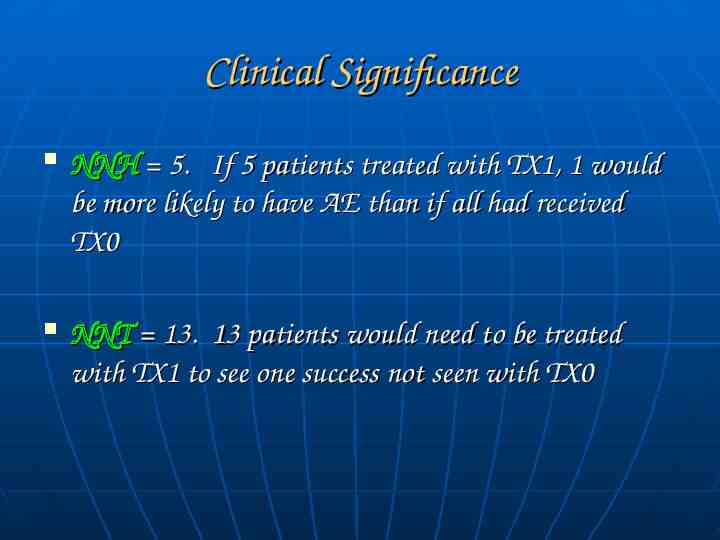
Clinical Significance NNH 5. If 5 patients treated with TX1, 1 would be more likely to have AE than if all had received TX0 NNT 13. 13 patients would need to be treated with TX1 to see one success not seen with TX0

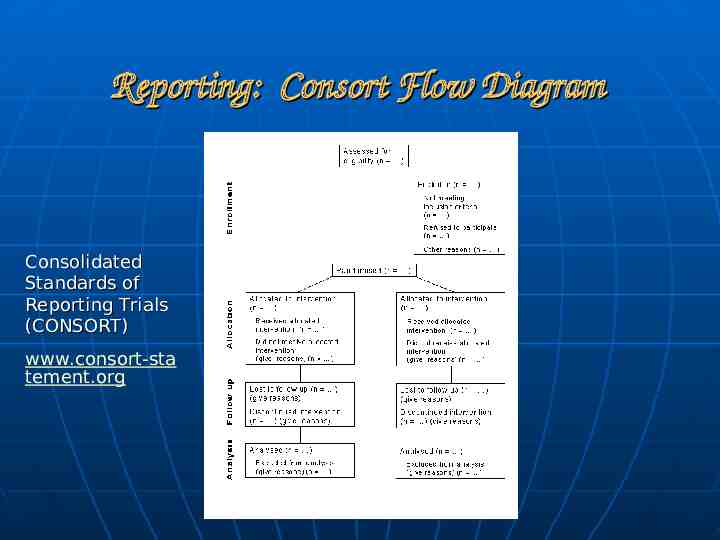
Reporting: Consort Flow Diagram Consolidated Standards of Reporting Trials (CONSORT) www.consort-sta tement.org
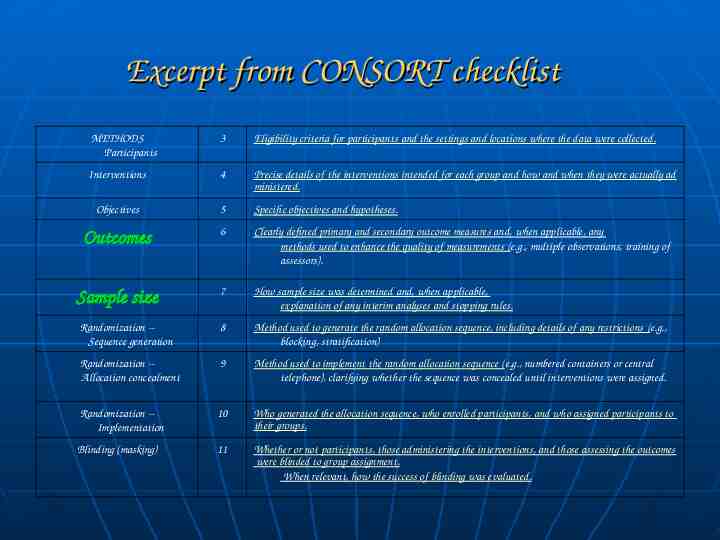
Excerpt from CONSORT checklist METHODS Participants 3 Eligibility criteria for participants and the settings and locations where the data were collected. Interventions 4 Precise details of the interventions intended for each group and how and when they were actually ad ministered. Objectives 5 Specific objectives and hypotheses. Outcomes 6 Clearly defined primary and secondary outcome measures and, when applicable, any methods used to enhance the quality of measurements (e.g., multiple observations, training of assessors). Sample size 7 How sample size was determined and, when applicable, explanation of any interim analyses and stopping rules. Randomization -Sequence generation 8 Method used to generate the random allocation sequence, including details of any restrictions (e.g., blocking, stratification) Randomization -Allocation concealment 9 Method used to implement the random allocation sequence (e.g., numbered containers or central telephone), clarifying whether the sequence was concealed until interventions were assigned. Randomization -Implementation 10 Who generated the allocation sequence, who enrolled participants, and who assigned participants to their groups. Blinding (masking) 11 Whether or not participants, those administering the interventions, and those assessing the outcomes were blinded to group assignment. When relevant, how the success of blinding was evaluated.
Evidence Synthesizer and Consumer Skills
Synthesizer Locate Critically appraise Meta-analysis Evidence User Locate Appraise quality & relevance Integrate Best available research evidence Clinical Decision-Making Patient’s values, characteristics, and circumstances Patient Understanding Preferences Access Researcher Design Conduct Analysis Reporting Clinical Expertise Clinician Communicate Assess patient Deliver EBP
Synthesizer: Systematic Reviewer- explicit, systematic, transparent to avoid bias Specific research question (PICO) Search protocol to select papers – key words systematic search of the literature (EMBASE, CINAHL, Cochrane Controlled Trial register, DARE) explicit inclusion and exclusion criteria Explicit, transparent rating of methodological quality Data extraction Analysis: qualitative or quantitative Conclusion Discussion of strengths and limitations
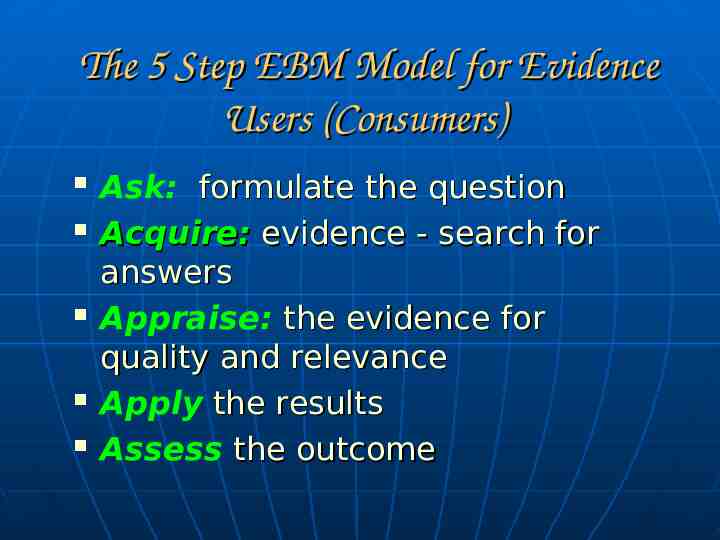
The 5 Step EBM Model for Evidence Users (Consumers) Ask: formulate the question Acquire: evidence - search for answers Appraise: the evidence for quality and relevance Apply the results Assess the outcome

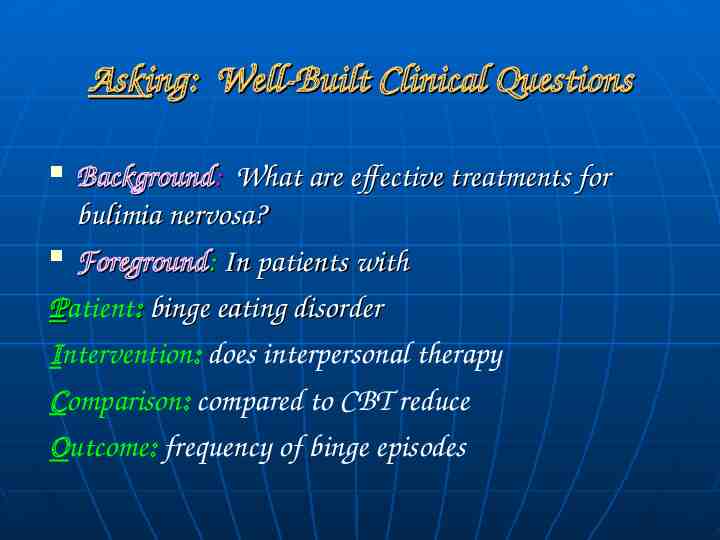
Asking: Well-Built Clinical Questions Background: What are effective treatments for bulimia nervosa? Foreground: In patients with Patient: binge eating disorder Intervention: does interpersonal therapy Comparison: compared to CBT reduce Outcome: frequency of binge episodes
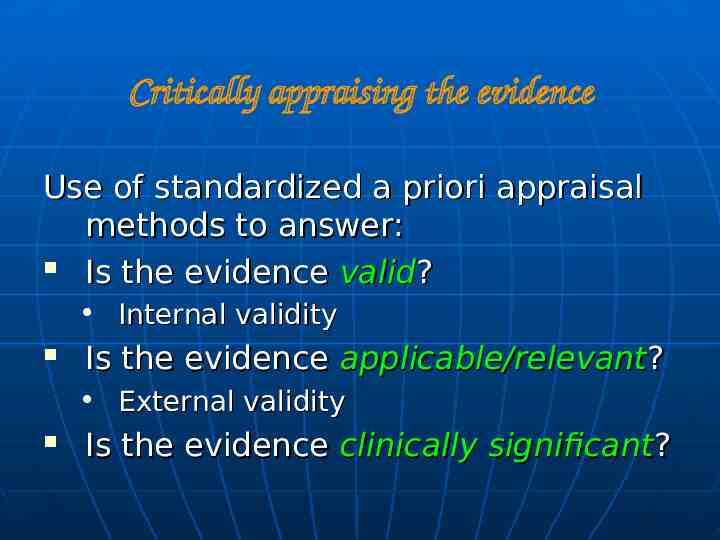
Critically appraising the evidence Use of standardized a priori appraisal methods to answer: Is the evidence valid? Internal validity Is the evidence applicable/relevant? External validity Is the evidence clinically significant?
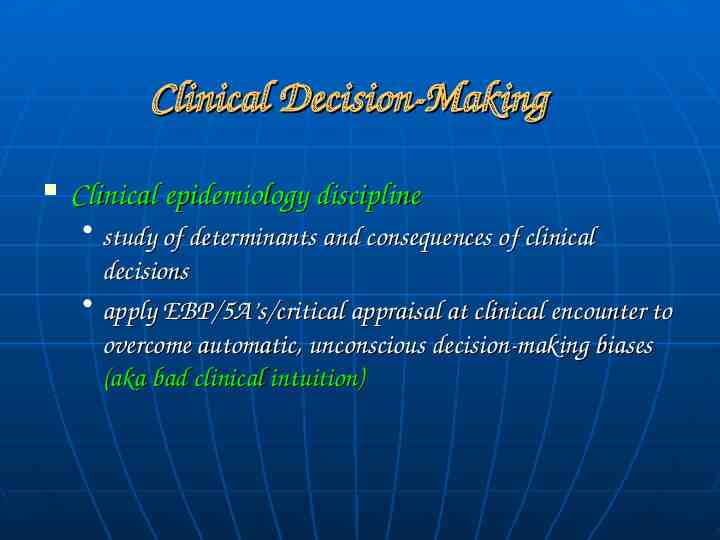
Clinical Decision-Making Clinical epidemiology discipline study of determinants and consequences of clinical decisions apply EBP/5A’s/critical appraisal at clinical encounter to overcome automatic, unconscious decision-making biases (aka bad clinical intuition)
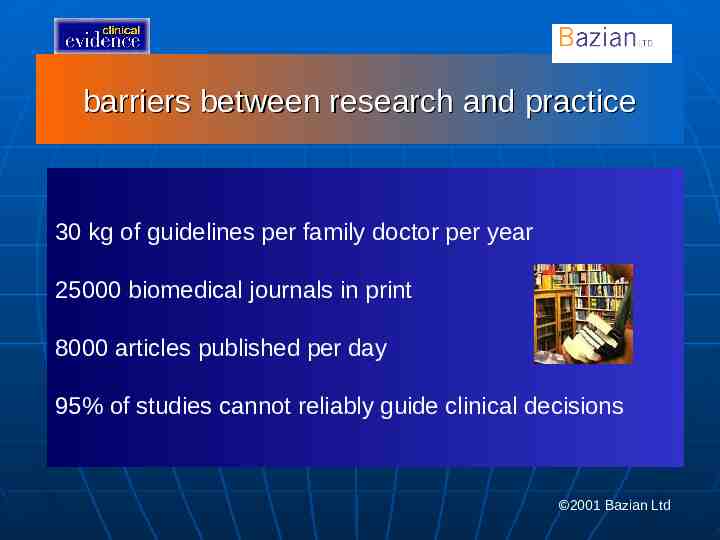
barriers between research and practice 30 kg of guidelines per family doctor per year 25000 biomedical journals in print 8000 articles published per day 95% of studies cannot reliably guide clinical decisions 2001 Bazian Ltd
Clinical Decision-Making Health Informatics discipline infrastructure, resources, devices, structures (e.g., algorithms, guidelines) needed to store, retrieve, manage and use health information and the time and place that a decision needs to be made. -Decision support.
Secondary Synthesized Evidence (AKA “evidence-based capitulation”) Research proliferates rapidly. Clinical performance demands increase. Practicing clinicians too busy to use all EBM steps will all patients. Increased focus on pithy clinical practice guidelines, synopses, and structured abstracts MD Consult ACP Journal Club Cochrane Database of Systematic Reviews “Up-to-date” InfoPOEMS (Patient Oriented Evidence that Matters)
Synthesizer Locate Critically appraise Meta-analysis Consumer Locate Appraise quality & relevance Integrate Researcher Design Conduct Analysis Reporting Best available research evidence Clinical Decision-Making Patient’s values, characteristics, and circumstances Clinical Expertise Clinician Patient Understanding Preferences Access Communicate Assess patient Deliver EBP
Clinically Supervised Training in EvidenceBased Treatment Needs work: 2005-2006 papers by Woody and by Weissman
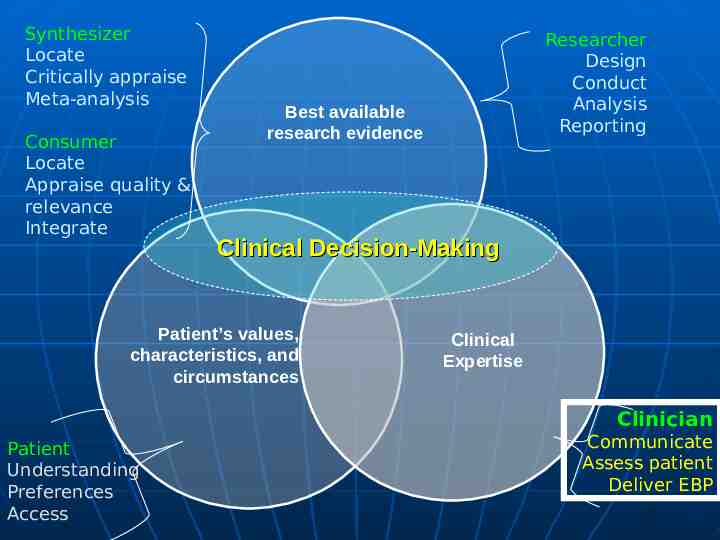
Synthesizer Locate Critically appraise Meta-analysis Consumer Locate Appraise quality & relevance Integrate Best available research evidence Clinical Decision-Making Patient’s values, characteristics, and circumstances Patient Understanding Preferences Access Researcher Design Conduct Analysis Reporting Clinical Expertise Clinician Communicate Assess patient Deliver EBP
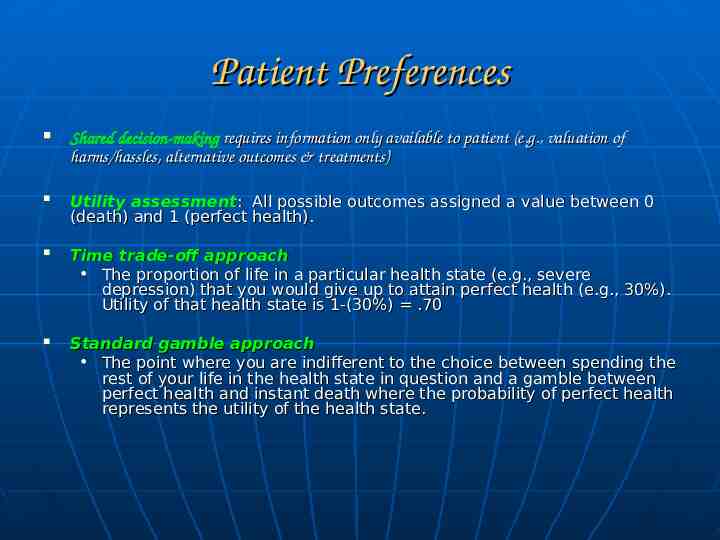
Patient Preferences Shared decision-making requires information only available to patient (e.g., valuation of harms/hassles, alternative outcomes & treatments) Utility assessment: All possible outcomes assigned a value between 0 (death) and 1 (perfect health). Time trade-off approach The proportion of life in a particular health state (e.g., severe depression) that you would give up to attain perfect health (e.g., 30%). Utility of that health state is 1-(30%) .70 Standard gamble approach The point where you are indifferent to the choice between spending the rest of your life in the health state in question and a gamble between perfect health and instant death where the probability of perfect health represents the utility of the health state.
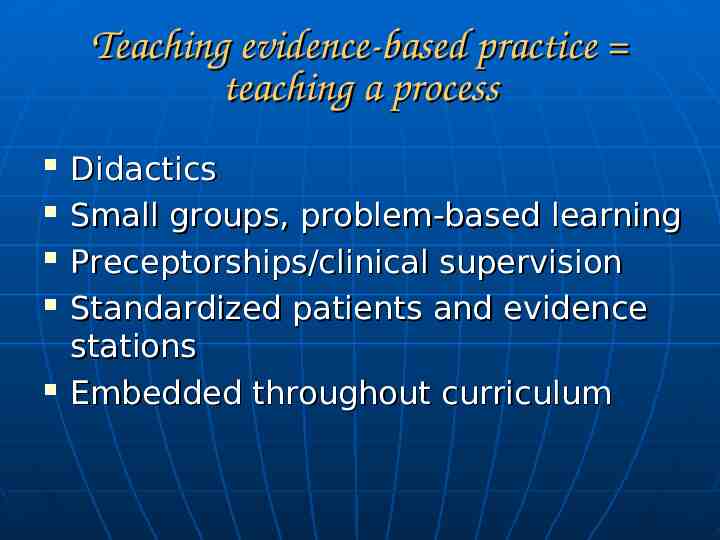
Teaching evidence-based practice teaching a process Didactics Small groups, problem-based learning Preceptorships/clinical supervision Standardized patients and evidence stations Embedded throughout curriculum
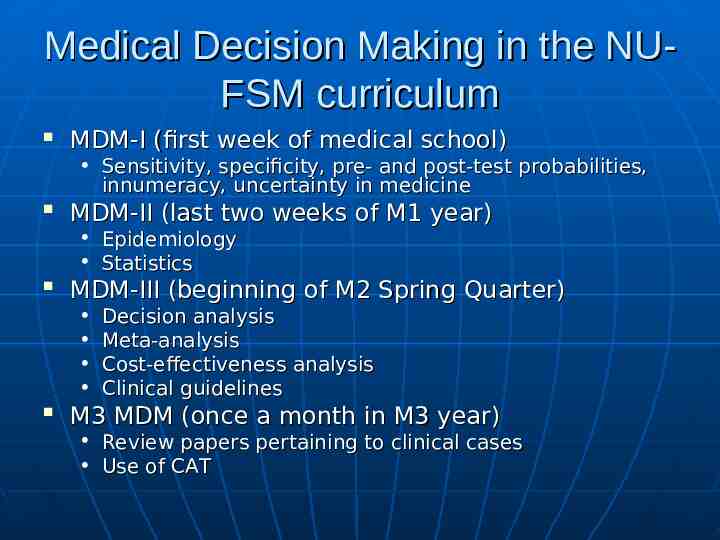
Medical Decision Making in the NUFSM curriculum MDM-I (first week of medical school) Sensitivity, specificity, pre- and post-test probabilities, innumeracy, uncertainty in medicine MDM-II (last two weeks of M1 year) Epidemiology Statistics MDM-III (beginning of M2 Spring Quarter) Decision analysis Meta-analysis Cost-effectiveness analysis Clinical guidelines M3 MDM (once a month in M3 year) Review papers pertaining to clinical cases Use of CAT
Evidence-Based Behavioral Practice (EBBP) NIH Office of Behavioral and Social Sciences Research contract N01-LM-6-3512: Resources for Training in EvidenceBased Behavioral Practice, 2006 - 2011
OBSSR 5-Year Plan Year 1: develop training website, Council, Scientific Advisory Board, white paper on training, skills, competencies reflecting education in evidence-based behavioral practice (EBBP) Year 2: develop, implement a web-based, research-focused training module(s) on EBBP; field test in graduate curricula Year 3: launch interactive web-based training courses; establish practice network, develop first EBBP clinical practice training module
OBSSR 5-Year Plan Year 4: With practice network, develop modules on application of evidence-based clinical decisionmaking to intervention with specific cases. Field test in internship/residency/post-doctoral training programs and practice network. Year 5: Link website to systematic reviews of behavioral interventions, treatment manuals, outcome assessments. Develop and field test clinical decision-making modules that integrate patient preference and clinical competency assessments.
Suggestions To enhance the evidence base for psychological treatments and support lifelong learning, clinical psychology training might benefit from enhanced coverage of: Researcher skills in methods: clinical trial design, analysis, reporting, synthesis Clinician training in 5-step (5A’s) EBP model – cover 2 A’s
Suggestions Psychology informatics could use infrastructure development (PSYCinfo & Cochrane; library access; coverage in secondary synthesized sources like Up-to-Date; practice-based research networks) Psychology could use appropriate patient preference measures that support shared decision-making A discipline of clinical psychology decision-making needs to develop to systematize integration of research evidence, clinical expertise, and patient clinical data and preferences
Concluding Questions What training modules and materials would be helpful? Will you partner with us to help develop and try these out?
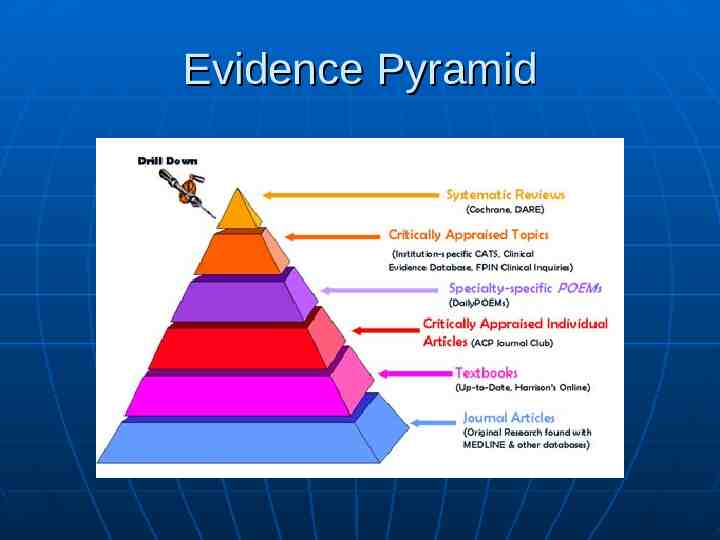
The Evidence Pyramid for Treatment Effectiveness Questions ***USE THE BEST EVIDENCE AVAILABLE***
Alternatives to evidence-based medicine Eminence based medicine Eloquence based medicine Vehemence based medicine Nervousness based medicine (Isaacs and Fitzgerald, 1999, BMJ)
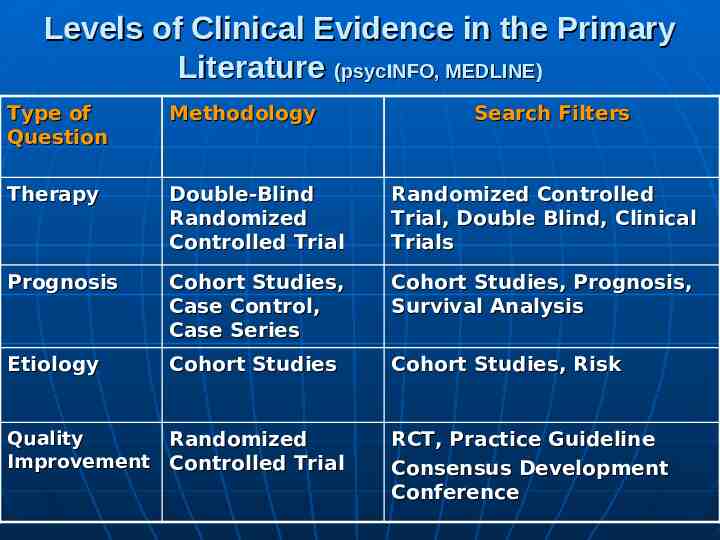
Levels of Clinical Evidence in the Primary Literature (psycINFO, MEDLINE) Type of Question Methodology Therapy Double-Blind Randomized Controlled Trial Randomized Controlled Trial, Double Blind, Clinical Trials Prognosis Cohort Studies, Case Control, Case Series Cohort Studies, Prognosis, Survival Analysis Etiology Cohort Studies Cohort Studies, Risk Quality Randomized Improvement Controlled Trial Search Filters RCT, Practice Guideline Consensus Development Conference
EBM Resources Pocket guides with web-linked updates (Sackett; Guyatt & Rennie) Cochrane Library BMJ: www.clinicalevidence.com Centre for EBM: http:// minerva.minervation.com Centre for Evidence-based mental health: www.cebmh.com
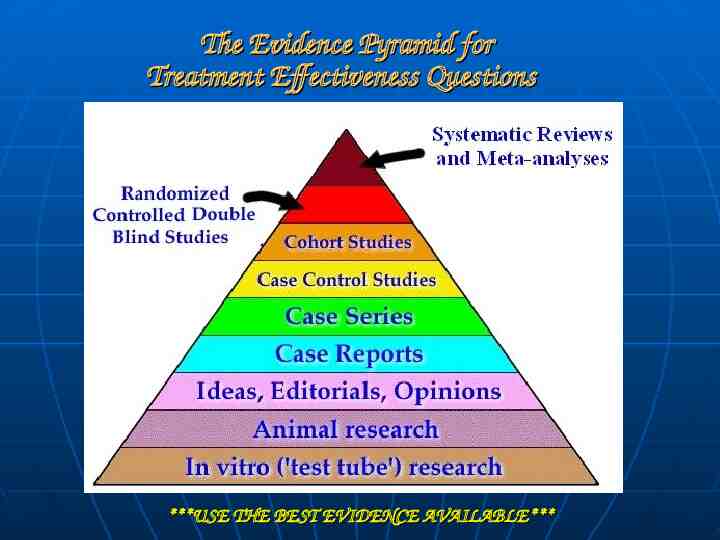
Evidence Pyramid

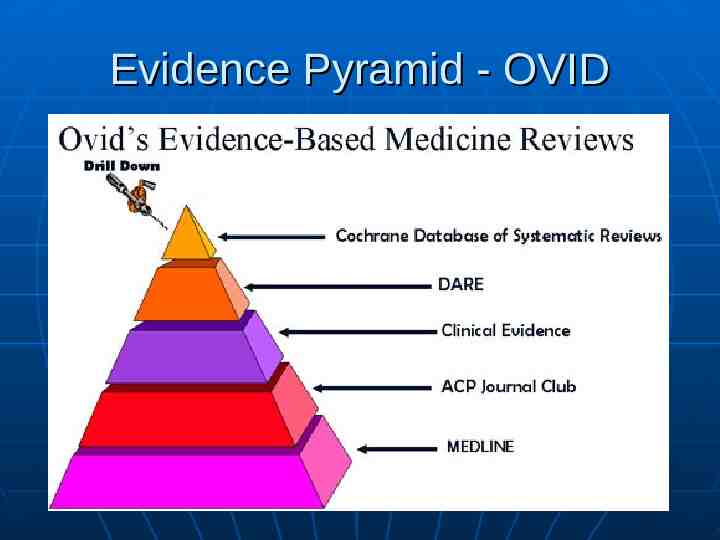
Evidence Pyramid - OVID
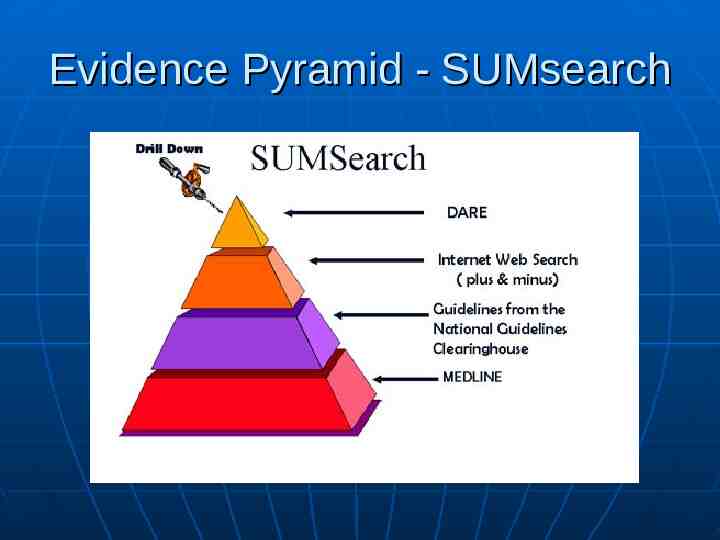
Evidence Pyramid - SUMsearch