Evaluation and Management 2021 A C S M E D I C A L B I L L I N G
37 Slides95.24 KB
Evaluation and Management 2021 A C S M E D I C A L B I L L I N G S O LU T I O N S
Why Change? Clinicians have long objected to the bullet counting and systems listing required for high-level E/M services. Sometimes, missing only family history for an 85-year-old patient would cause the visit to be coded at a low level, no matter how complex the patient was. With the addition of electronic health records, everyone agreed that there was often unnecessary and repetitive information in the record, and at times the information was contradictory or unbelievable. Many clinicians thought that complexity should guide code selection. In 2021, they will get their wish. Codes 99202—99215 may be selected based on time or medical decision making.
Overview of Changes CPT code 99201 has been deleted CPT has significantly changed the documentation requirements for new and established outpatient codes (99202-99215) Providers will now determine the level of service based on either Time or Medical Decision A Medically appropriate history and/or exam will be included in the encounter note, but the content of these elements is no longer a factor in code selection The extent of History and Exam elements will be determined by the Physician or other Non Physician providers, as dictated by the patient’s medical condition
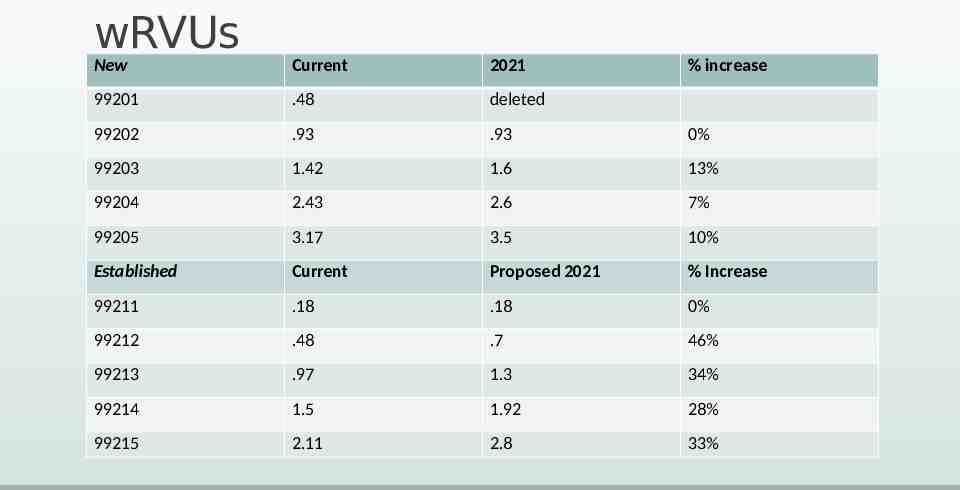
wRVUs New Current 2021 % increase 99201 .48 deleted 99202 .93 .93 0% 99203 1.42 1.6 13% 99204 2.43 2.6 7% 99205 3.17 3.5 10% Established Current Proposed 2021 % Increase 99211 .18 .18 0% 99212 .48 .7 46% 99213 .97 1.3 34% 99214 1.5 1.92 28% 99215 2.11 2.8 33%
Future Changes to Evaluation and Management Services All other Evaluation and Management services will remain the same with respect to documentation requirements to include: Inpatient services 99221-99233 Emergency services 99281-99285 Nursing Facility services 99304-99310 Domiciliary and Home services 99324-99337 ***however the CPT panel is looking at these other codes sets moving forward.
Billing Based on Time
Definition and Elements of Time Time is defined as total time spent for the visit, including non face to face time, (for example documenting encounter elements, or phone calls) that requires the professional skill of the provider on the same calendar day. It is recommended that the provider document what they spent a significant amount of time on, in rendering care. Time is no longer dependent on counseling and coordination of care Face to Face is still required Time ranges have been assigned versus a fixed amount of time Time spent on separately billable services may not be included in the total time of the visit (for example if you interpret an EKG, you may not include that time in the total time of the visit) CPT codes 99202-99204 and 99212-99214 are no longer eligible for Prolonged service code
Activities contributing to Time Time spent preparing to see the patient, for example review of diagnostics Time spent reviewing a separately collected history Time spent on physical exam Time spent on ordering treatment(s) Time spent on referrals to other health care professionals Time spent documenting the encounter Time spent on independent review of diagnostics and interpretation of findings (unless the provider is separately billing for the interpretation of the study). Care coordination when not billed as a separate service
Separately Reported If The Provider or the provider’s practice performed a service that is separately reported, (an additional published CPT code) the time spent on that service may not be included in determining the code selection for an Evaluation and Management service. For example: the provider orders, performs, and interprets an abdominal ultrasound. The provider bills 76775 in addition to the E/M based on the activities contributing to total time.
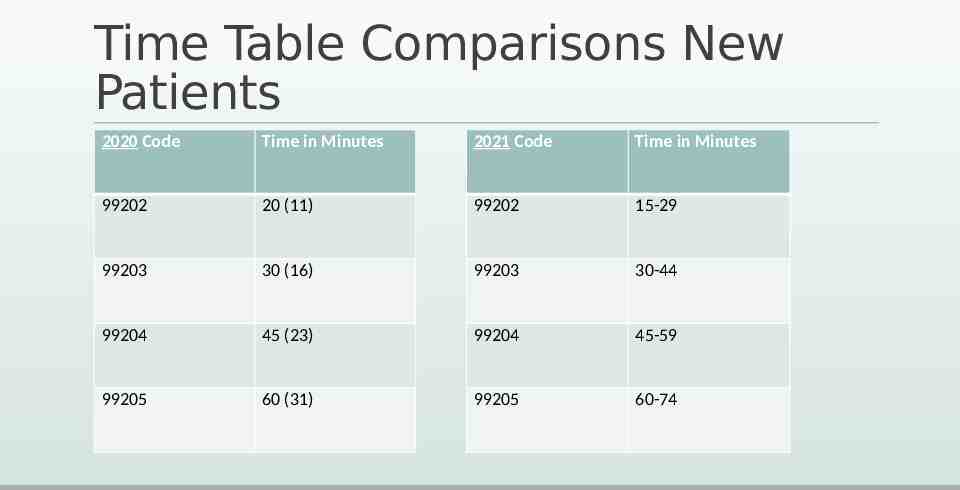
Time Table Comparisons New Patients 2020 Code Time in Minutes 2021 Code Time in Minutes 99202 20 (11) 99202 15-29 99203 30 (16) 99203 30-44 99204 45 (23) 99204 45-59 99205 60 (31) 99205 60-74
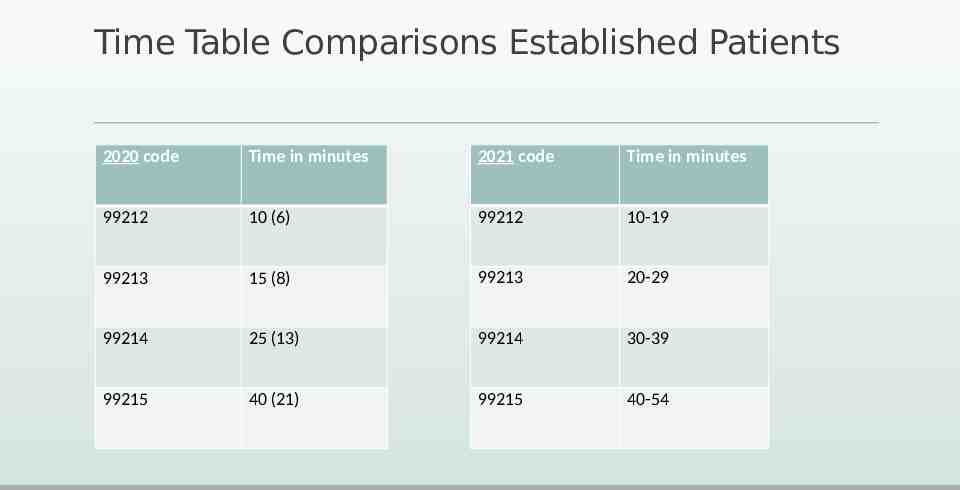
Time Table Comparisons Established Patients 2020 code Time in minutes 2021 code Time in minutes 99212 10 (6) 99212 10-19 99213 15 (8) 99213 20-29 99214 25 (13) 99214 30-39 99215 40 (21) 99215 40-54
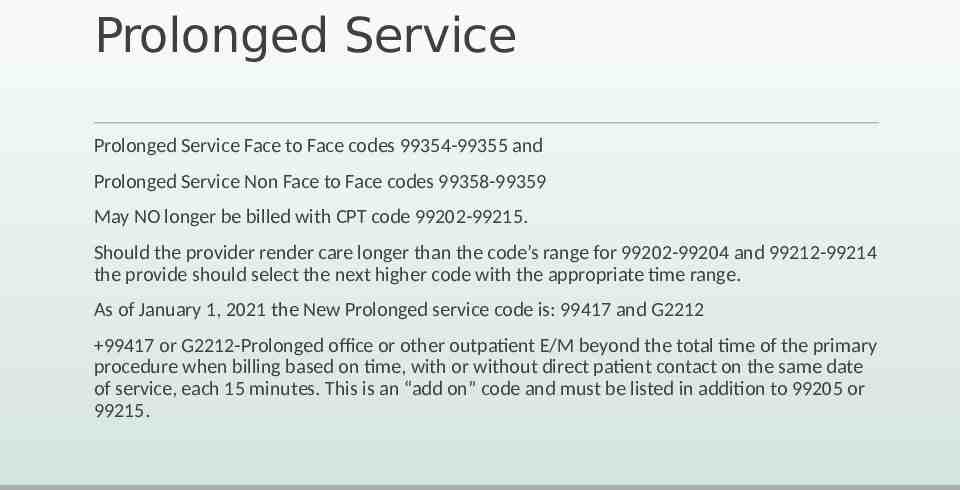
Prolonged Service Prolonged Service Face to Face codes 99354-99355 and Prolonged Service Non Face to Face codes 99358-99359 May NO longer be billed with CPT code 99202-99215. Should the provider render care longer than the code’s range for 99202-99204 and 99212-99214 the provide should select the next higher code with the appropriate time range. As of January 1, 2021 the New Prolonged service code is: 99417 and G2212 99417 or G2212-Prolonged office or other outpatient E/M beyond the total time of the primary procedure when billing based on time, with or without direct patient contact on the same date of service, each 15 minutes. This is an “add on” code and must be listed in addition to 99205 or 99215.
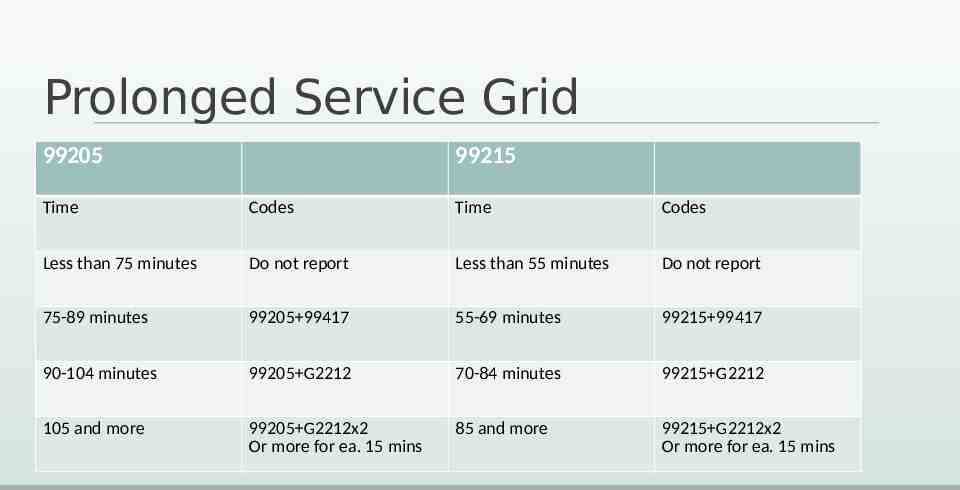
Prolonged Service Grid 99205 99215 Time Codes Time Codes Less than 75 minutes Do not report Less than 55 minutes Do not report 75-89 minutes 99205 99417 55-69 minutes 99215 99417 90-104 minutes 99205 G2212 70-84 minutes 99215 G2212 105 and more 99205 G2212x2 Or more for ea. 15 mins 85 and more 99215 G2212x2 Or more for ea. 15 mins
Questions about billing based on Time?
Selecting an E/M based on Medical Decision
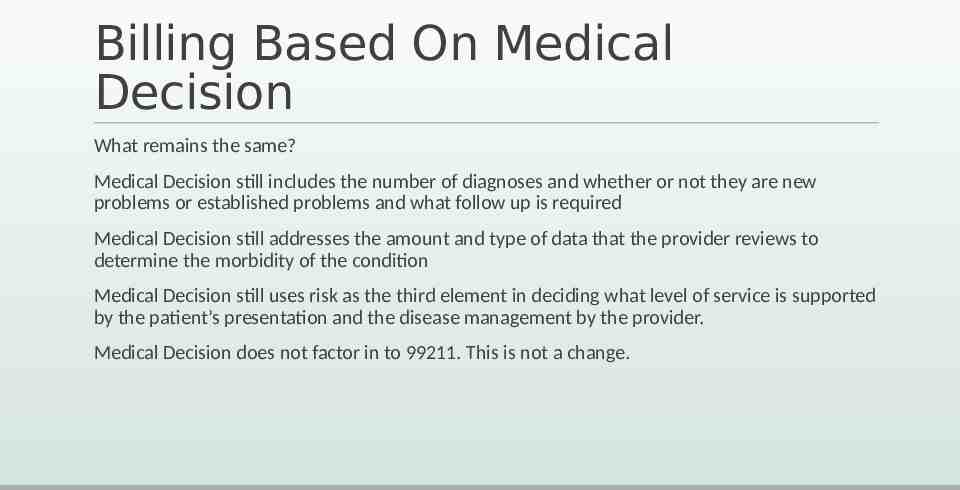
Billing Based On Medical Decision What remains the same? Medical Decision still includes the number of diagnoses and whether or not they are new problems or established problems and what follow up is required Medical Decision still addresses the amount and type of data that the provider reviews to determine the morbidity of the condition Medical Decision still uses risk as the third element in deciding what level of service is supported by the patient’s presentation and the disease management by the provider. Medical Decision does not factor in to 99211. This is not a change.
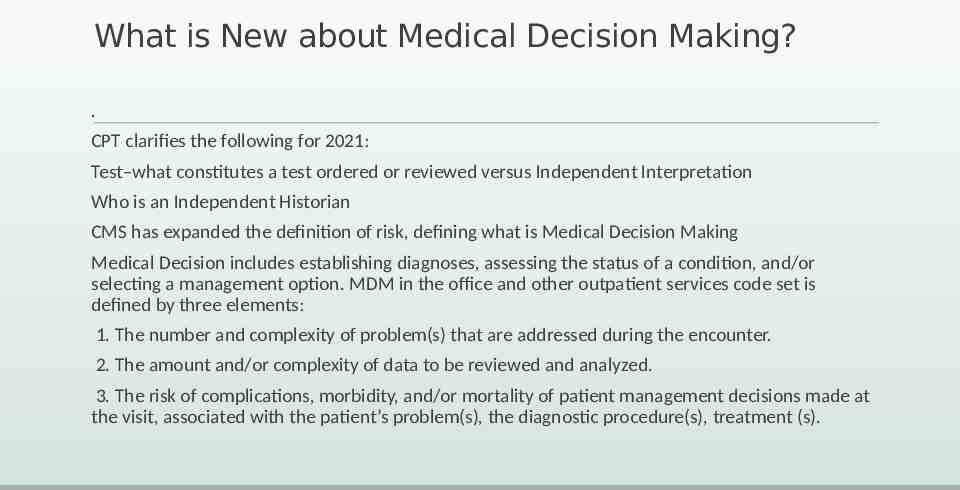
What is New about Medical Decision Making? . CPT clarifies the following for 2021: Test–what constitutes a test ordered or reviewed versus Independent Interpretation Who is an Independent Historian CMS has expanded the definition of risk, defining what is Medical Decision Making Medical Decision includes establishing diagnoses, assessing the status of a condition, and/or selecting a management option. MDM in the office and other outpatient services code set is defined by three elements: 1. The number and complexity of problem(s) that are addressed during the encounter. 2. The amount and/or complexity of data to be reviewed and analyzed. 3. The risk of complications, morbidity, and/or mortality of patient management decisions made at the visit, associated with the patient’s problem(s), the diagnostic procedure(s), treatment (s).
Levels of Medical Decision Making The level of MDM reflected in the proposed changes is the same level of MDM currently associated with these levels of service as we know them today. The providers must still meet 2 of the three broad categories: The Number/complexity of problems Data, collected ordered or reviewed Risk Levels of Medical Decision Making
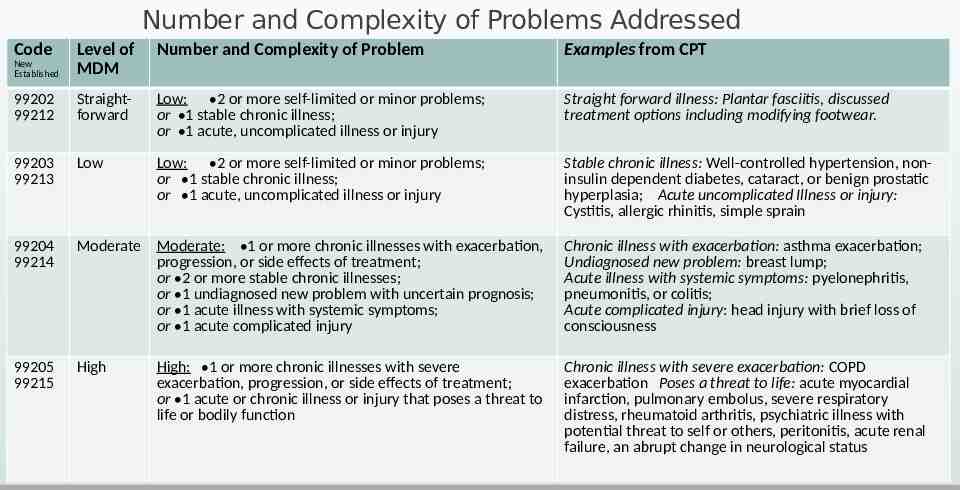
Number and Complexity of Problems Addressed Code Level of MDM Number and Complexity of Problem Examples from CPT New Established 99202 99212 Straightforward Low: 2 or more self-limited or minor problems; or 1 stable chronic illness; or 1 acute, uncomplicated illness or injury Straight forward illness: Plantar fasciitis, discussed treatment options including modifying footwear. 99203 99213 Low Low: 2 or more self-limited or minor problems; or 1 stable chronic illness; or 1 acute, uncomplicated illness or injury Stable chronic illness: Well-controlled hypertension, noninsulin dependent diabetes, cataract, or benign prostatic hyperplasia; Acute uncomplicated Illness or injury: Cystitis, allergic rhinitis, simple sprain 99204 99214 Moderate Moderate: 1 or more chronic illnesses with exacerbation, progression, or side effects of treatment; or 2 or more stable chronic illnesses; or 1 undiagnosed new problem with uncertain prognosis; or 1 acute illness with systemic symptoms; or 1 acute complicated injury Chronic illness with exacerbation: asthma exacerbation; Undiagnosed new problem: breast lump; Acute illness with systemic symptoms: pyelonephritis, pneumonitis, or colitis; Acute complicated injury: head injury with brief loss of consciousness 99205 99215 High Chronic illness with severe exacerbation: COPD exacerbation Poses a threat to life: acute myocardial infarction, pulmonary embolus, severe respiratory distress, rheumatoid arthritis, psychiatric illness with potential threat to self or others, peritonitis, acute renal failure, an abrupt change in neurological status High: 1 or more chronic illnesses with severe exacerbation, progression, or side effects of treatment; or 1 acute or chronic illness or injury that poses a threat to life or bodily function
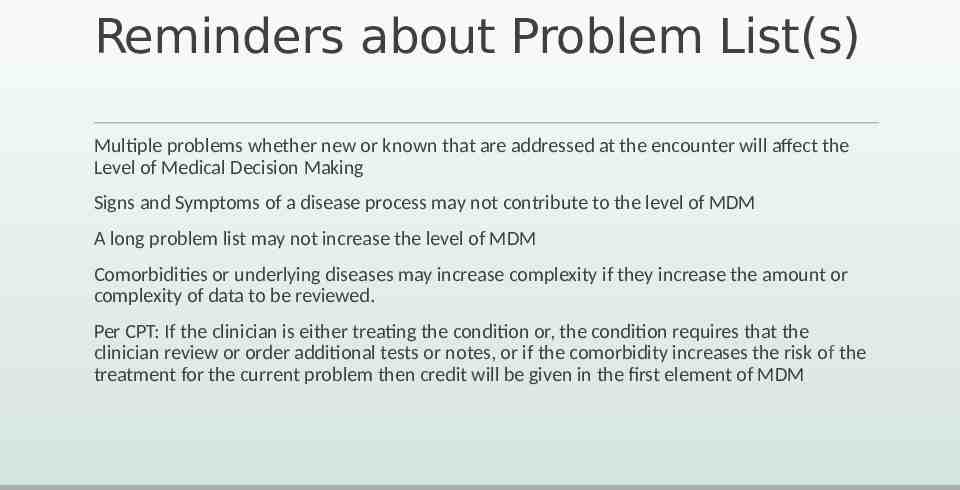
Reminders about Problem List(s) Multiple problems whether new or known that are addressed at the encounter will affect the Level of Medical Decision Making Signs and Symptoms of a disease process may not contribute to the level of MDM A long problem list may not increase the level of MDM Comorbidities or underlying diseases may increase complexity if they increase the amount or complexity of data to be reviewed. Per CPT: If the clinician is either treating the condition or, the condition requires that the clinician review or order additional tests or notes, or if the comorbidity increases the risk of the treatment for the current problem then credit will be given in the first element of MDM
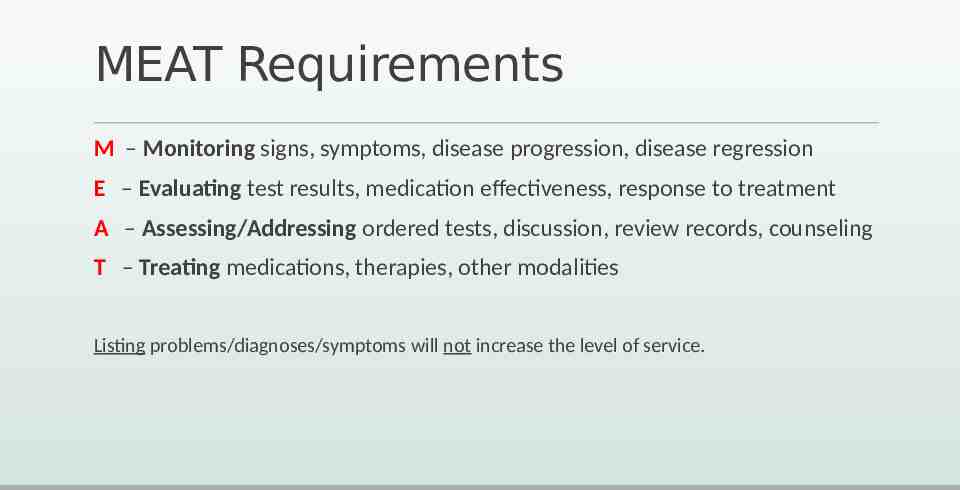
MEAT Requirements M – Monitoring signs, symptoms, disease progression, disease regression E – Evaluating test results, medication effectiveness, response to treatment A – Assessing/Addressing ordered tests, discussion, review records, counseling T – Treating medications, therapies, other modalities Listing problems/diagnoses/symptoms will not increase the level of service.
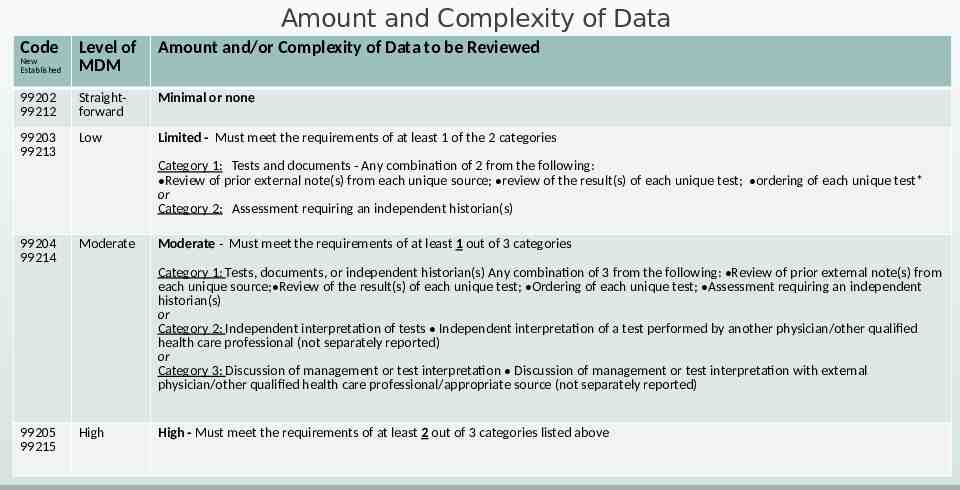
Amount and Complexity of Data Code Level of MDM Amount and/or Complexity of Data to be Reviewed New Established 99202 99212 Straightforward Minimal or none 99203 99213 Low Limited - Must meet the requirements of at least 1 of the 2 categories Category 1: Tests and documents - Any combination of 2 from the following: Review of prior external note(s) from each unique source; review of the result(s) of each unique test; ordering of each unique test* or Category 2: Assessment requiring an independent historian(s) 99204 99214 Moderate Moderate - Must meet the requirements of at least 1 out of 3 categories Category 1: Tests, documents, or independent historian(s) Any combination of 3 from the following: Review of prior external note(s) from each unique source; Review of the result(s) of each unique test; Ordering of each unique test; Assessment requiring an independent historian(s) or Category 2: Independent interpretation of tests Independent interpretation of a test performed by another physician/other qualified health care professional (not separately reported) or Category 3: Discussion of management or test interpretation Discussion of management or test interpretation with external physician/other qualified health care professional/appropriate source (not separately reported) 99205 99215 High High - Must meet the requirements of at least 2 out of 3 categories listed above
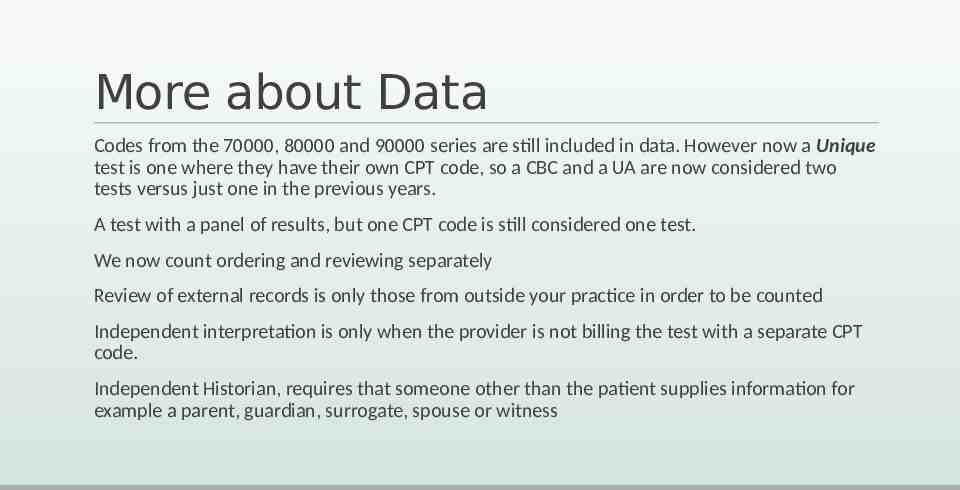
More about Data Codes from the 70000, 80000 and 90000 series are still included in data. However now a Unique test is one where they have their own CPT code, so a CBC and a UA are now considered two tests versus just one in the previous years. A test with a panel of results, but one CPT code is still considered one test. We now count ordering and reviewing separately Review of external records is only those from outside your practice in order to be counted Independent interpretation is only when the provider is not billing the test with a separate CPT code. Independent Historian, requires that someone other than the patient supplies information for example a parent, guardian, surrogate, spouse or witness
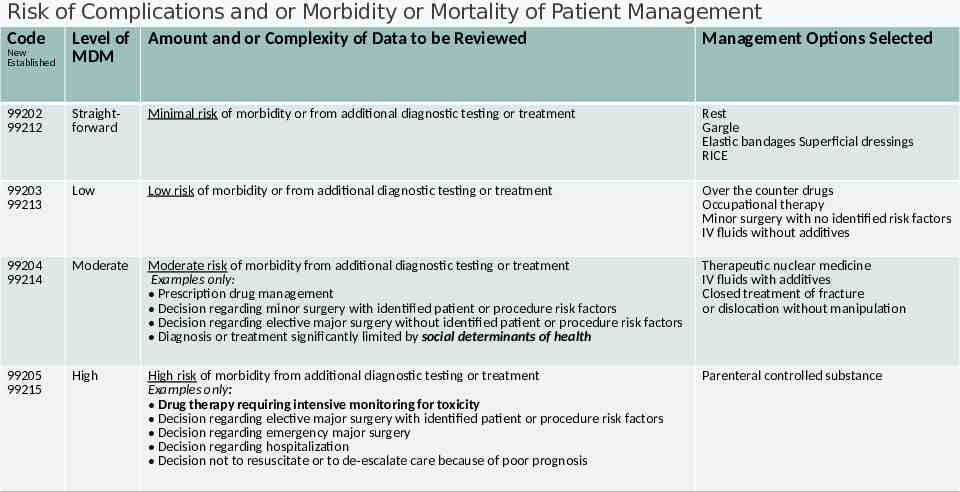
Risk of Complications and or Morbidity or Mortality of Patient Management Code New Established Level of Amount and or Complexity of Data to be Reviewed MDM Management Options Selected 99202 99212 Straightforward Minimal risk of morbidity or from additional diagnostic testing or treatment Rest Gargle Elastic bandages Superficial dressings RICE 99203 99213 Low Low risk of morbidity or from additional diagnostic testing or treatment Over the counter drugs Occupational therapy Minor surgery with no identified risk factors IV fluids without additives 99204 99214 Moderate Moderate risk of morbidity from additional diagnostic testing or treatment Examples only: Prescription drug management Decision regarding minor surgery with identified patient or procedure risk factors Decision regarding elective major surgery without identified patient or procedure risk factors Diagnosis or treatment significantly limited by social determinants of health Therapeutic nuclear medicine IV fluids with additives Closed treatment of fracture or dislocation without manipulation 99205 99215 High High risk of morbidity from additional diagnostic testing or treatment Examples only: Drug therapy requiring intensive monitoring for toxicity Decision regarding elective major surgery with identified patient or procedure risk factors Decision regarding emergency major surgery Decision regarding hospitalization Decision not to resuscitate or to de-escalate care because of poor prognosis Parenteral controlled substance
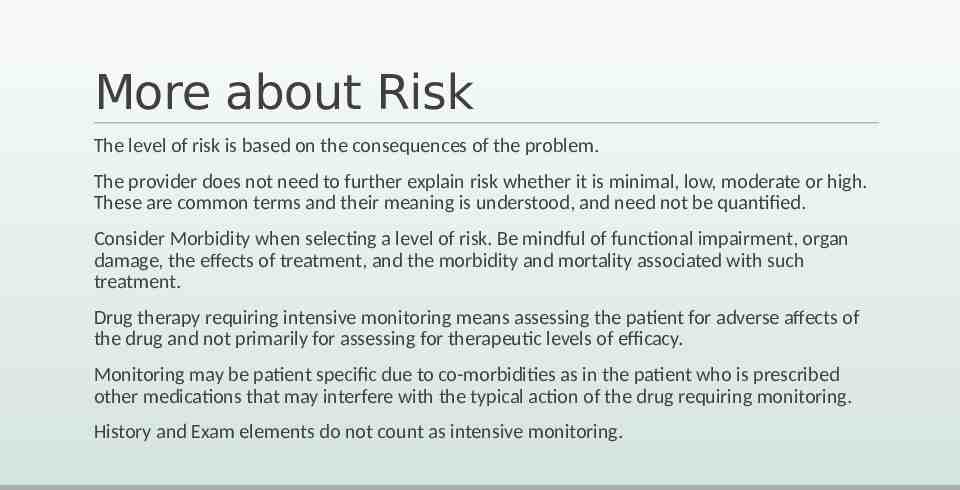
More about Risk The level of risk is based on the consequences of the problem. The provider does not need to further explain risk whether it is minimal, low, moderate or high. These are common terms and their meaning is understood, and need not be quantified. Consider Morbidity when selecting a level of risk. Be mindful of functional impairment, organ damage, the effects of treatment, and the morbidity and mortality associated with such treatment. Drug therapy requiring intensive monitoring means assessing the patient for adverse affects of the drug and not primarily for assessing for therapeutic levels of efficacy. Monitoring may be patient specific due to co-morbidities as in the patient who is prescribed other medications that may interfere with the typical action of the drug requiring monitoring. History and Exam elements do not count as intensive monitoring.
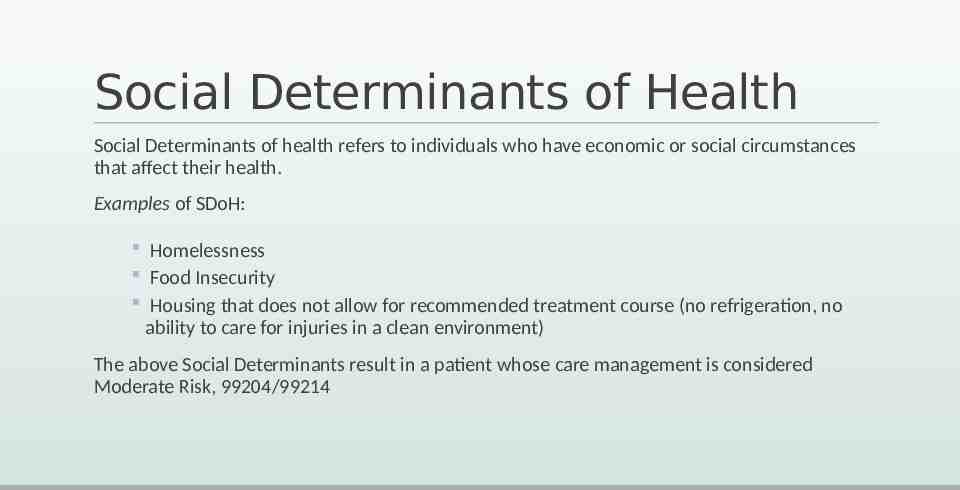
Social Determinants of Health Social Determinants of health refers to individuals who have economic or social circumstances that affect their health. Examples of SDoH: Homelessness Food Insecurity Housing that does not allow for recommended treatment course (no refrigeration, no ability to care for injuries in a clean environment) The above Social Determinants result in a patient whose care management is considered Moderate Risk, 99204/99214
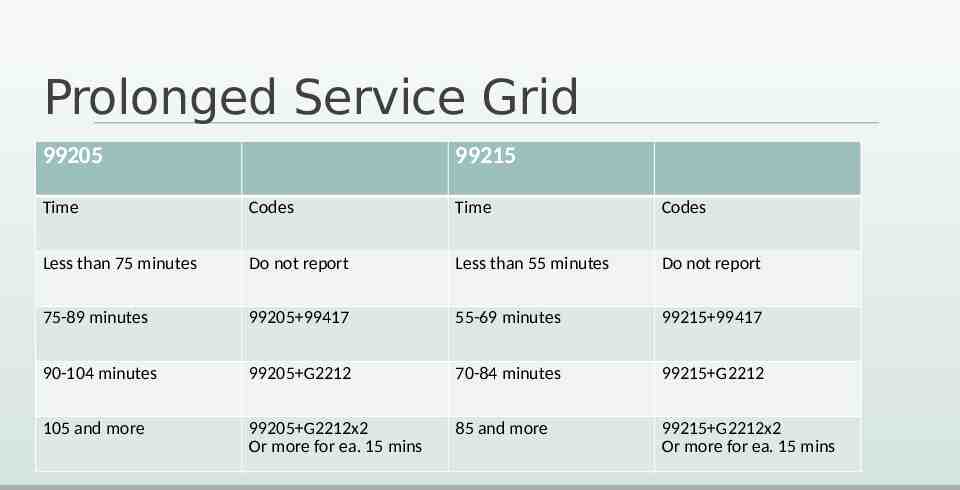
Prolonged Service Grid 99205 99215 Time Codes Time Codes Less than 75 minutes Do not report Less than 55 minutes Do not report 75-89 minutes 99205 99417 55-69 minutes 99215 99417 90-104 minutes 99205 G2212 70-84 minutes 99215 G2212 105 and more 99205 G2212x2 Or more for ea. 15 mins 85 and more 99215 G2212x2 Or more for ea. 15 mins
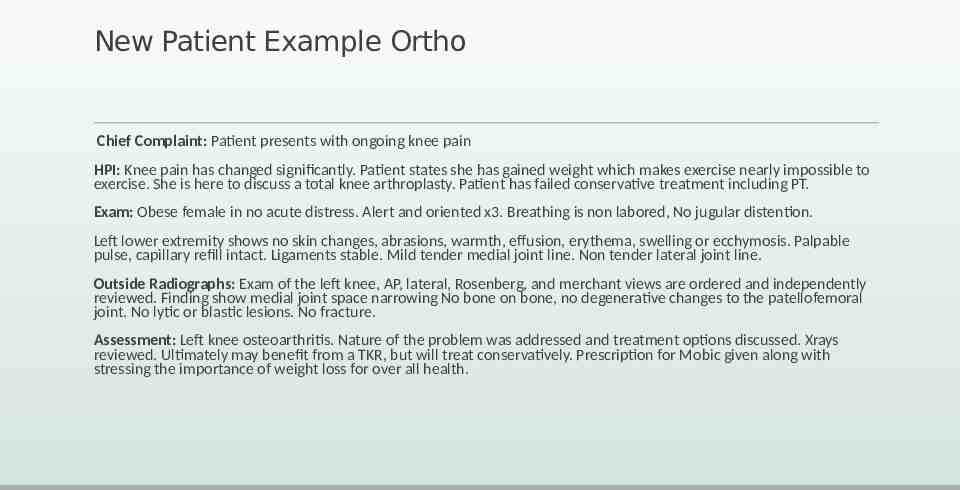
New Patient Example Ortho Chief Complaint: Patient presents with ongoing knee pain HPI: Knee pain has changed significantly. Patient states she has gained weight which makes exercise nearly impossible to exercise. She is here to discuss a total knee arthroplasty. Patient has failed conservative treatment including PT. Exam: Obese female in no acute distress. Alert and oriented x3. Breathing is non labored, No jugular distention. Left lower extremity shows no skin changes, abrasions, warmth, effusion, erythema, swelling or ecchymosis. Palpable pulse, capillary refill intact. Ligaments stable. Mild tender medial joint line. Non tender lateral joint line. Outside Radiographs: Exam of the left knee, AP, lateral, Rosenberg, and merchant views are ordered and independently reviewed. Finding show medial joint space narrowing No bone on bone, no degenerative changes to the patellofemoral joint. No lytic or blastic lesions. No fracture. Assessment: Left knee osteoarthritis. Nature of the problem was addressed and treatment options discussed. Xrays reviewed. Ultimately may benefit from a TKR, but will treat conservatively. Prescription for Mobic given along with stressing the importance of weight loss for over all health.
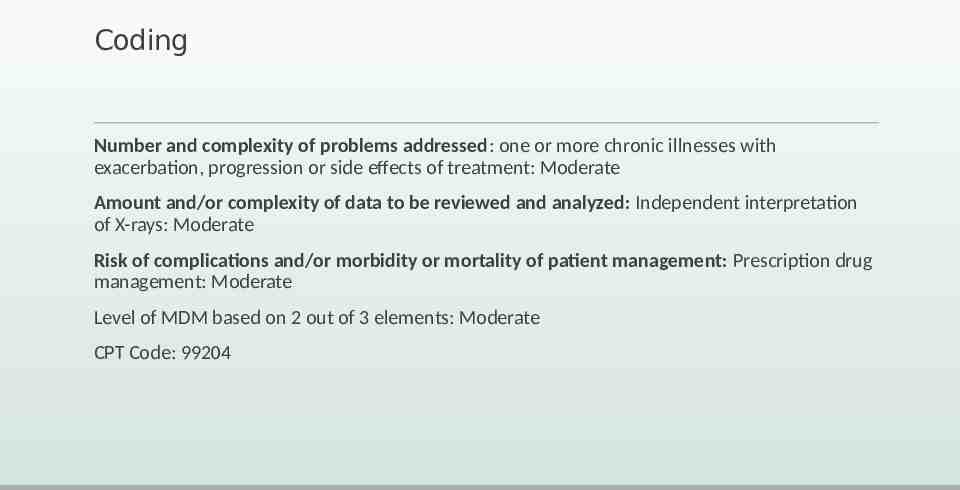
Coding Number and complexity of problems addressed: one or more chronic illnesses with exacerbation, progression or side effects of treatment: Moderate Amount and/or complexity of data to be reviewed and analyzed: Independent interpretation of X-rays: Moderate Risk of complications and/or morbidity or mortality of patient management: Prescription drug management: Moderate Level of MDM based on 2 out of 3 elements: Moderate CPT Code: 99204
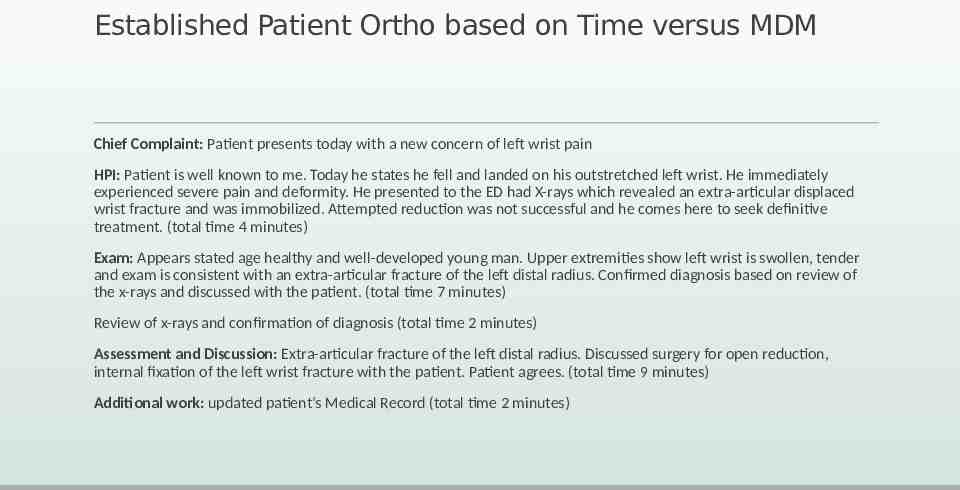
Established Patient Ortho based on Time versus MDM Chief Complaint: Patient presents today with a new concern of left wrist pain HPI: Patient is well known to me. Today he states he fell and landed on his outstretched left wrist. He immediately experienced severe pain and deformity. He presented to the ED had X-rays which revealed an extra-articular displaced wrist fracture and was immobilized. Attempted reduction was not successful and he comes here to seek definitive treatment. (total time 4 minutes) Exam: Appears stated age healthy and well-developed young man. Upper extremities show left wrist is swollen, tender and exam is consistent with an extra-articular fracture of the left distal radius. Confirmed diagnosis based on review of the x-rays and discussed with the patient. (total time 7 minutes) Review of x-rays and confirmation of diagnosis (total time 2 minutes) Assessment and Discussion: Extra-articular fracture of the left distal radius. Discussed surgery for open reduction, internal fixation of the left wrist fracture with the patient. Patient agrees. (total time 9 minutes) Additional work: updated patient’s Medical Record (total time 2 minutes)
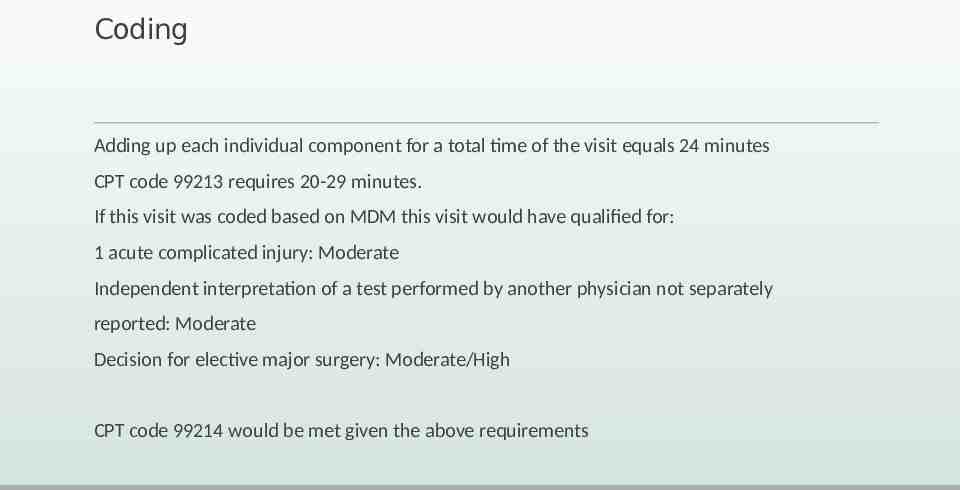
Coding Adding up each individual component for a total time of the visit equals 24 minutes CPT code 99213 requires 20-29 minutes. If this visit was coded based on MDM this visit would have qualified for: 1 acute complicated injury: Moderate Independent interpretation of a test performed by another physician not separately reported: Moderate Decision for elective major surgery: Moderate/High CPT code 99214 would be met given the above requirements
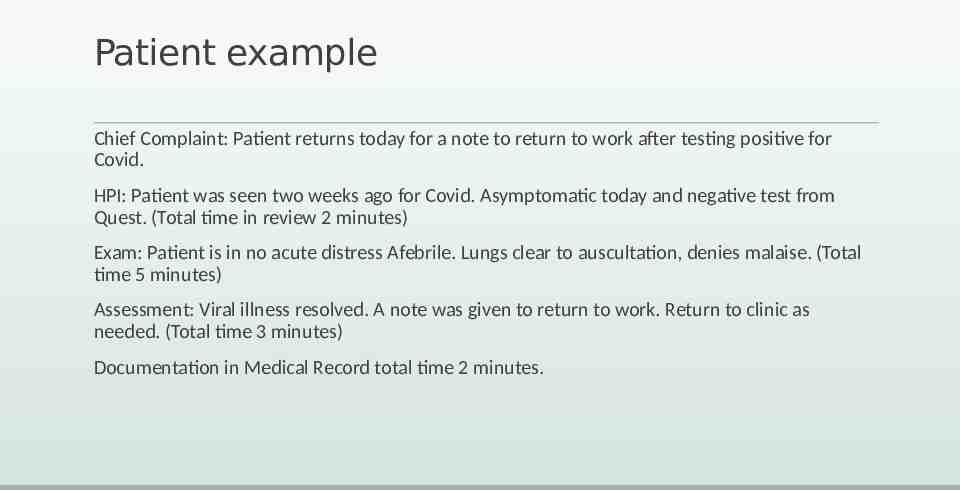
Patient example Chief Complaint: Patient returns today for a note to return to work after testing positive for Covid. HPI: Patient was seen two weeks ago for Covid. Asymptomatic today and negative test from Quest. (Total time in review 2 minutes) Exam: Patient is in no acute distress Afebrile. Lungs clear to auscultation, denies malaise. (Total time 5 minutes) Assessment: Viral illness resolved. A note was given to return to work. Return to clinic as needed. (Total time 3 minutes) Documentation in Medical Record total time 2 minutes.
Coding Code Selected 99212 Rationale 99212 time range is 10-19 minutes MDM comparison: 99211
How do we Prepare for 2021? Consider what is happening currently Take a close look at the new requirements and determine where there may be gaps in documentation What E/M CPT code can be supported with current documentation Begin Education regarding upcoming changes Talk to EMR/EHR vendors to make necessary changes to streamline templates Test the time element now to determine the feasibility Continue to follow your MAC carrier and AMA for any changes prior to 2021 Read the final rule when released
Documentation Guidelines for Providers Encourage the providers to clearly document the complexity of condition(s) and assist in the understanding of the affect it will have on level of service Document assessment and plan to avoid any confusion in the event of an audit Document clearly any diagnostic studies (70000, 80000 and 90000 series codes) and why they were ordered Always include independent interpretation when performed For continuity of care instruct providers to document clinically appropriate history and examination.
References CMS and local MAC CodingIntel AMA CPT the Professional Edition AAPC Decision Health
Thank you/ Questions Tammy G. Heim Director of Physician Education and Compliance [email protected] (o)337-706-1536 337-354-6055