Electronic Health Records Robert A. Jenders, MD, MS, FACP
76 Slides8.67 MB
Electronic Health Records Robert A. Jenders, MD, MS, FACP Associate Professor, Department of Medicine Cedars-Sinai Medical Center University of California, Los Angeles Co-Chair, Clinical Decision Support Technical Committee, HL7 6 October 2005 http://jenders.bol.ucla.edu - Documents & Presentations

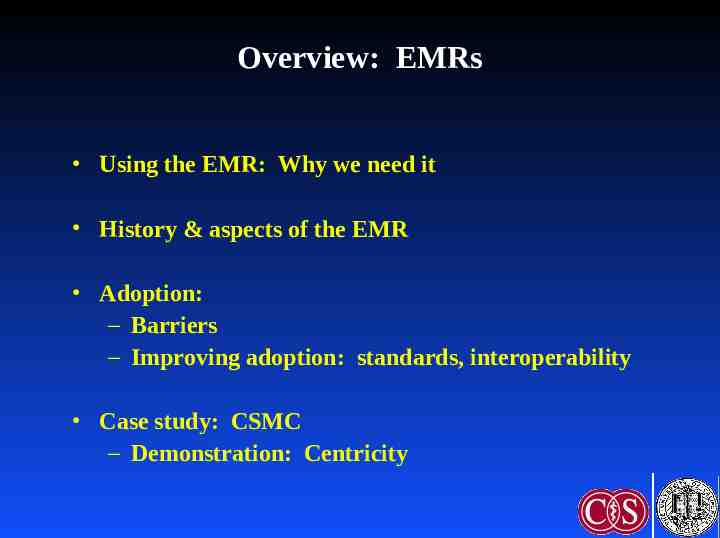
Overview: EMRs Using the EMR: Why we need it History & aspects of the EMR Adoption: – Barriers – Improving adoption: standards, interoperability Case study: CSMC – Demonstration: Centricity

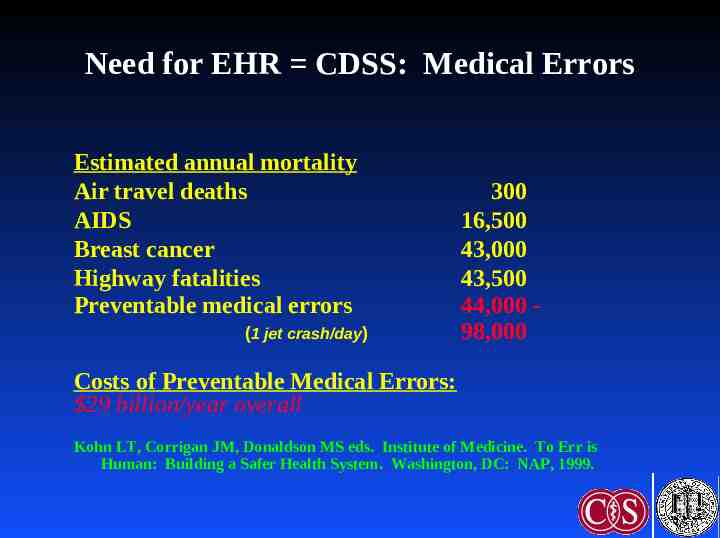
Need for EHR CDSS: Medical Errors Estimated annual mortality Air travel deaths AIDS Breast cancer Highway fatalities Preventable medical errors (1 jet crash/day) 300 16,500 43,000 43,500 44,000 98,000 Costs of Preventable Medical Errors: 29 billion/year overall Kohn LT, Corrigan JM, Donaldson MS eds. Institute of Medicine. To Err is Human: Building a Safer Health System. Washington, DC: NAP, 1999.
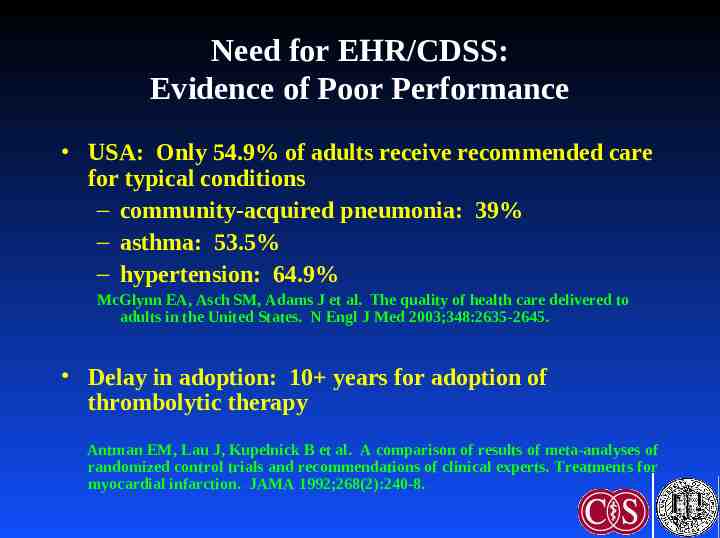
Need for EHR/CDSS: Evidence of Poor Performance USA: Only 54.9% of adults receive recommended care for typical conditions – community-acquired pneumonia: 39% – asthma: 53.5% – hypertension: 64.9% McGlynn EA, Asch SM, Adams J et al. The quality of health care delivered to adults in the United States. N Engl J Med 2003;348:2635-2645. Delay in adoption: 10 years for adoption of thrombolytic therapy Antman EM, Lau J, Kupelnick B et al. A comparison of results of meta-analyses of randomized control trials and recommendations of clinical experts. Treatments for myocardial infarction. JAMA 1992;268(2):240-8.
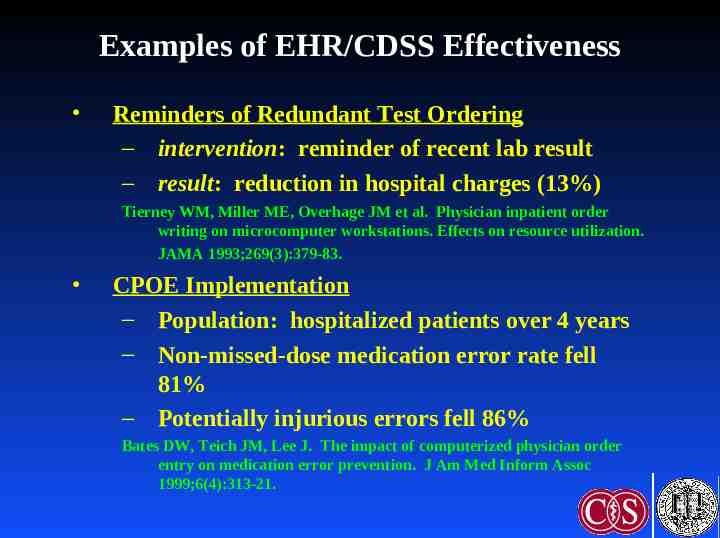
Examples of EHR/CDSS Effectiveness Reminders of Redundant Test Ordering – intervention: reminder of recent lab result – result: reduction in hospital charges (13%) Tierney WM, Miller ME, Overhage JM et al. Physician inpatient order writing on microcomputer workstations. Effects on resource utilization. JAMA 1993;269(3):379-83. CPOE Implementation – Population: hospitalized patients over 4 years – Non-missed-dose medication error rate fell 81% – Potentially injurious errors fell 86% Bates DW, Teich JM, Lee J. The impact of computerized physician order entry on medication error prevention. J Am Med Inform Assoc 1999;6(4):313-21.
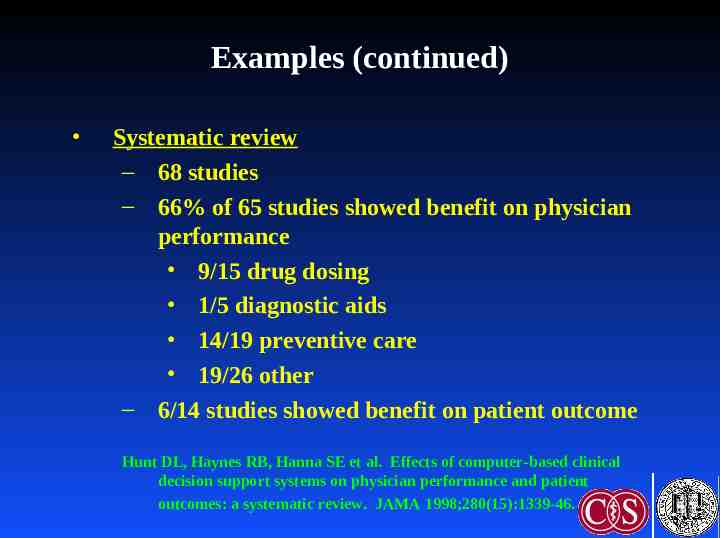
Examples (continued) Systematic review – 68 studies – 66% of 65 studies showed benefit on physician performance 9/15 drug dosing 1/5 diagnostic aids 14/19 preventive care 19/26 other – 6/14 studies showed benefit on patient outcome Hunt DL, Haynes RB, Hanna SE et al. Effects of computer-based clinical decision support systems on physician performance and patient outcomes: a systematic review. JAMA 1998;280(15):1339-46.
Summary: Need for EHR (CDSS) Medical errors are costly – Charges/Costs – Morbidity/Mortality CDSS technology can help reduce – errors – costs EHR – Collection and organization of data – Vehicle for decision support
Definitions Computer-based Patient Record (CPR): Electronic documentation of care, integrating data from multiple sources (clinical, demographic info) – EMR: Single computer application for recording and viewing data related to patient care, typically ambulatory – EHR: Suite of applications for recording, organizing and viewing clinical data Ancillary systems, clinical data repository, results review, “CIS”, “HIS”
Uses of the Medical Record Main purpose: Facilitate patient care Historical record: What happened, what was done Communication among providers (& patients) Preventive care (immunizations, etc) Quality assurance Legal record Financial: coding, billing Research: prospective, retrospective
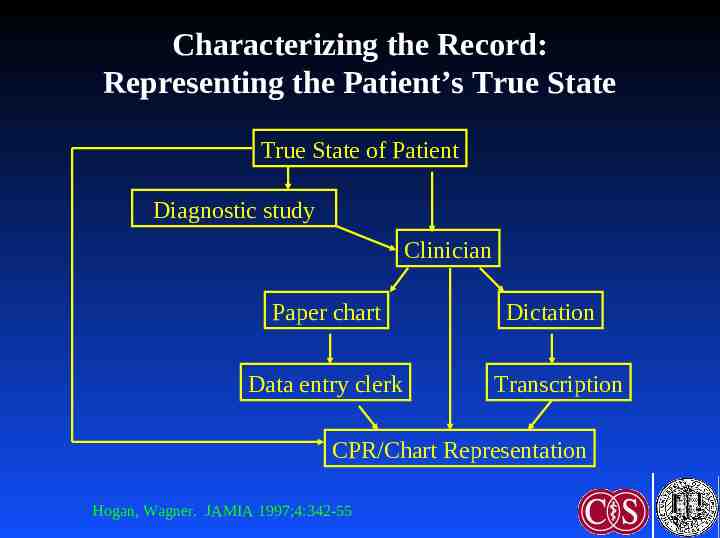
Characterizing the Record: Representing the Patient’s True State True State of Patient Diagnostic study Clinician Paper chart Data entry clerk Dictation Transcription CPR/Chart Representation Hogan, Wagner. JAMIA 1997;4:342-55
Characterizing the Record: Representing the Patient’s True State Completeness: Proportion of observations actually recorded – 67 - 100% Correctness: Proportion of recorded observations that are correct – 67 - 100%
Functional Components Integration of data – Standards: Messaging (HL7), terminology (LOINC, SNOMED, ICD9, etc), data model (HL7 RIM) – Interface engine Clinical decision support Order entry Knowledge sources Communication support: Multidisciplinary, consultation
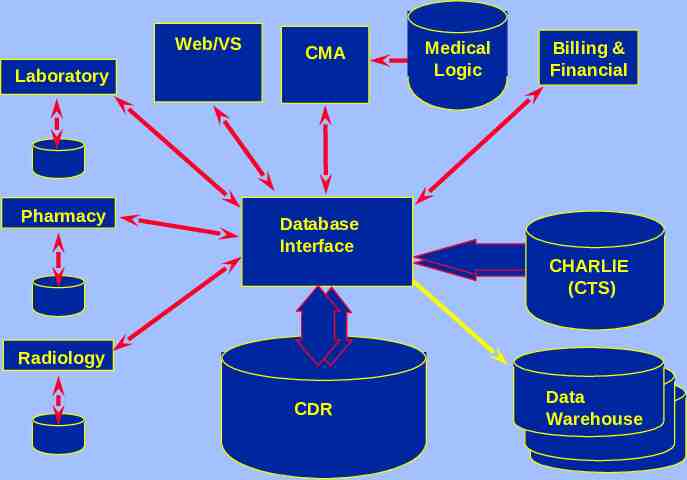
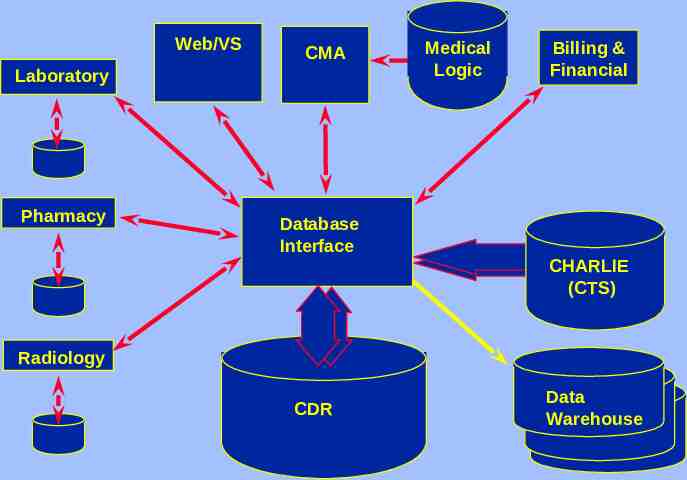
Web/VS CMA Laboratory Pharmacy Medical Logic Billing & Financial Database Interface CHARLIE (CTS) Radiology CDR Data Warehouse
History of the Medical Record 1910: Flexner Report--Advocated maintaining patient records 1940s: Hospitals need records for accreditation 1960s: Electronic HIS--communication (routing orders) & charge capture 1969: Weed--POMR 1980s: IOM report, academic systems 1990s - present: Increasing commercial systems, increasing prevalence, emphasis on interoperability & standards (ONCHIT, etc)
Trend Toward Outpatient Records Inpatient record structured first – Regulatory requirement – Many contributors (vs solo family practitioner) – Reimbursement: More money than outpatient visits Now, more attention to outpatient records – Multidisciplinary/team care – Managed care
Who Enters Data Clerk Physician: Primary, consultant, extender Nurse Therapist Lab reports/ancillary systems Machines: Monitors, POC testing
Fundamental Issue: Data Entry Data capture: External sources – Laboratory information systems, monitors, etc – Challenges: Interfaces, standards Data input: Direct entry by clinicians & staff – Challenge: Time-consuming and expensive – “Free text” vs structured entry
Data Input Transcription of dictation: Very expensive, errorprone Encounter form: Various types – Free-text entry – Scannable forms Turnaround document: Both presents & captures data Direct electronic entry – Free-text typing – Structured entry: Pick lists, etc – Voice recognition
Weakness of Paper Record Find the record: Lost, being used elsewhere Find data within the record: Poorly organized, missing, fragmented Read data: Legibility Update data: Where to record if chart is missing (e.g., “shadow chart”) Only one view – Redundancy: Re-entry of data in multiple forms – Research: Difficult to search across patients Passive: No decision support
Advantages of Computer Records Access: Speed, remote location, simultaneous use (even if just an “electronic typewriter”) Legibility Reduced data entry: Reuse data, reduce redundant tests Better organization: Structure Multiple views: Aggregation – Example: Summary report, structured flow sheet (contrast different data types) – Alter display based on context
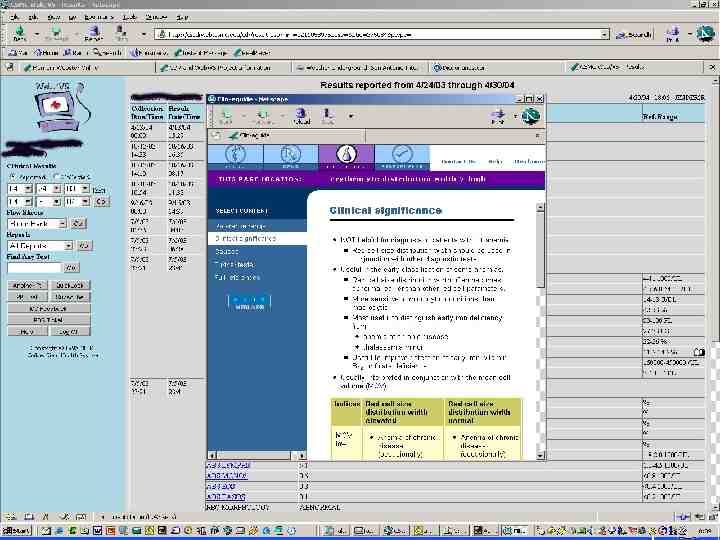
Advantages of Computer Records (continued) Automated checks on data entry – Data prompts: Completeness – Range check (reference range) – Pattern check (# digits in MRN) – Computed check (CBC differential adds to 100) – Consistency check (pregnant man!) – Delta check – Spelling check
Advantages of Computer Records (continued) Automated decision support – Reminders, alerts, calculations, ordering advice – Limited by scope/accuracy of electronic data Tradeoff: Data specificity/depth of advice vs time/cost of completeness Cross-patient analysis – Research – Stratify patient prognosis, treatment by risks Data review: Avoid overlooking uncommon but important events
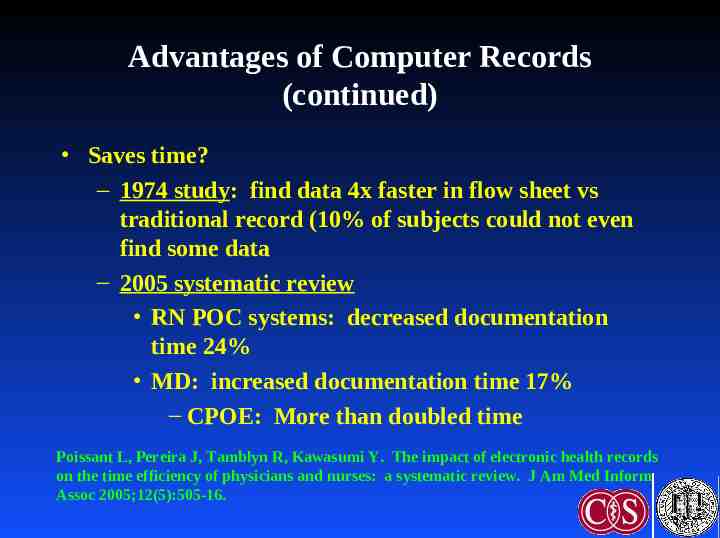
Advantages of Computer Records (continued) Saves time? – 1974 study: find data 4x faster in flow sheet vs traditional record (10% of subjects could not even find some data – 2005 systematic review RN POC systems: decreased documentation time 24% MD: increased documentation time 17% – CPOE: More than doubled time Poissant L, Pereira J, Tamblyn R, Kawasumi Y. The impact of electronic health records on the time efficiency of physicians and nurses: a systematic review. J Am Med Inform Assoc 2005;12(5):505-16.
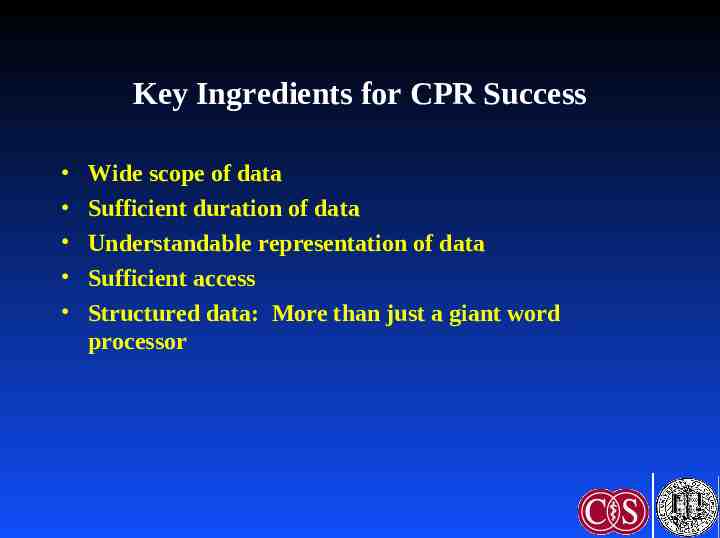
Key Ingredients for CPR Success Wide scope of data Sufficient duration of data Understandable representation of data Sufficient access Structured data: More than just a giant word processor
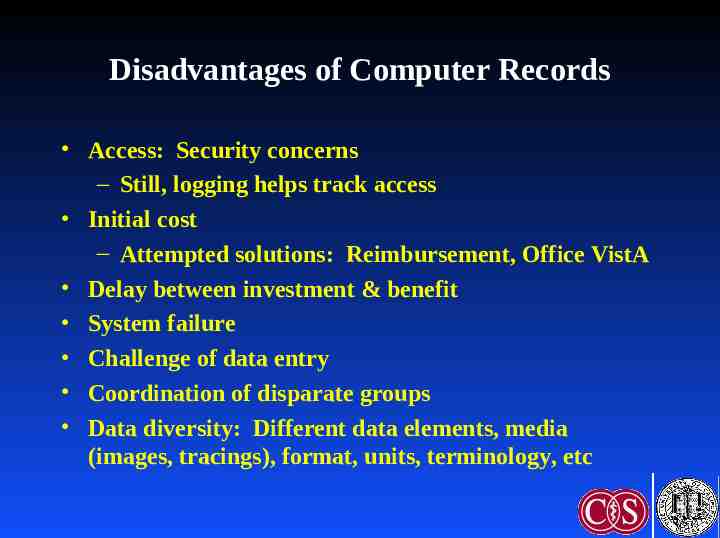
Disadvantages of Computer Records Access: Security concerns – Still, logging helps track access Initial cost – Attempted solutions: Reimbursement, Office VistA Delay between investment & benefit System failure Challenge of data entry Coordination of disparate groups Data diversity: Different data elements, media (images, tracings), format, units, terminology, etc
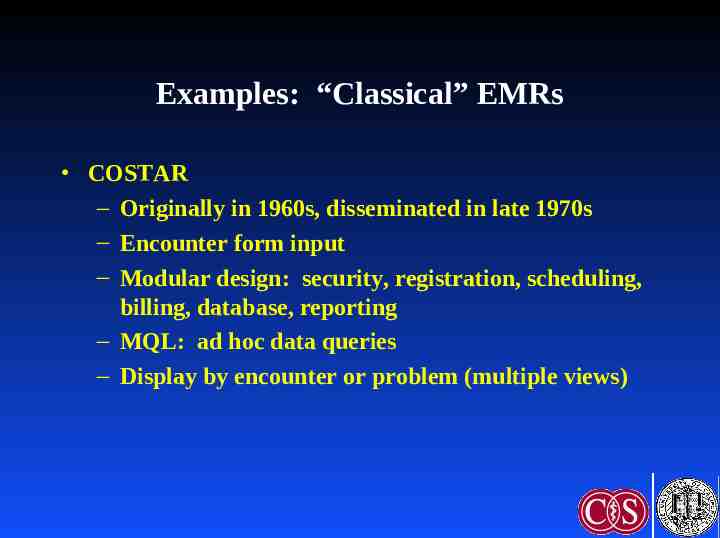
Examples: “Classical” EMRs COSTAR – Originally in 1960s, disseminated in late 1970s – Encounter form input – Modular design: security, registration, scheduling, billing, database, reporting – MQL: ad hoc data queries – Display by encounter or problem (multiple views)
“Classical” EMRs (continued) RMRS: McDonald (IU), 1974 TMR: Stead & Hammond (Duke), 1975 STOR: Whiting-O’Keefe (UCSF), 1985
Adoption No advantage if not used! Varying prevalence in USA – 20-25% (CHCF, “Use and Adoption of Computerbased Patient Records,” October, 2003) – 20% (MGMA, January, 2005) – 17% (CDC ambulatory medical care survey 2001-3, published March, 2005) Higher prevalence elsewhere – Netherlands 90%, Australia 65% – Reasons: Single-payer system, certification, costsharing
Barriers to EHR Adoption Financial: Up-front costs, training, uncertain ROI (misalignment of benefits & costs), finding the right system Cultural: Attitude toward IT Technological: Interoperability, support, data exchange Organizational: Integrate with workflow, migration from paper
Improving Adoption Interoperability: Increase chance that EHRs can be used with each other other systems – Systemic Interoperability Commission Compensation – CPT code: CMS trial – P4P: Reporting measures; decision support to improve performance Standards – Certification: CCR, EHR Functional Model & Specification – HIPAA/NCVHS & CHI
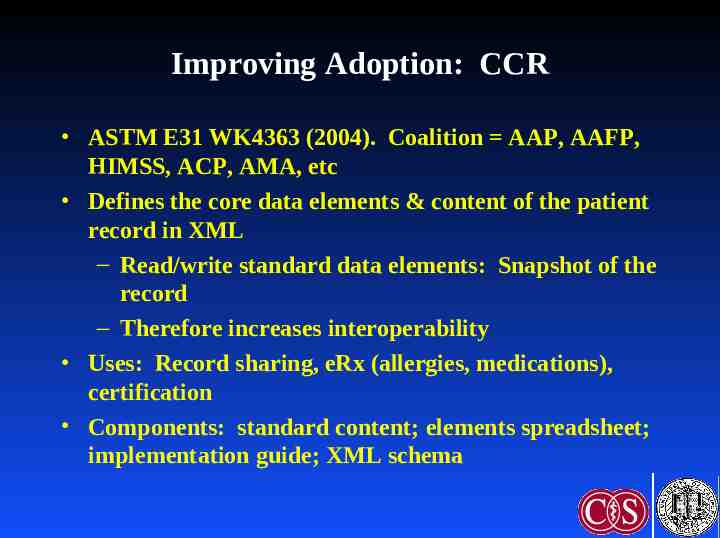
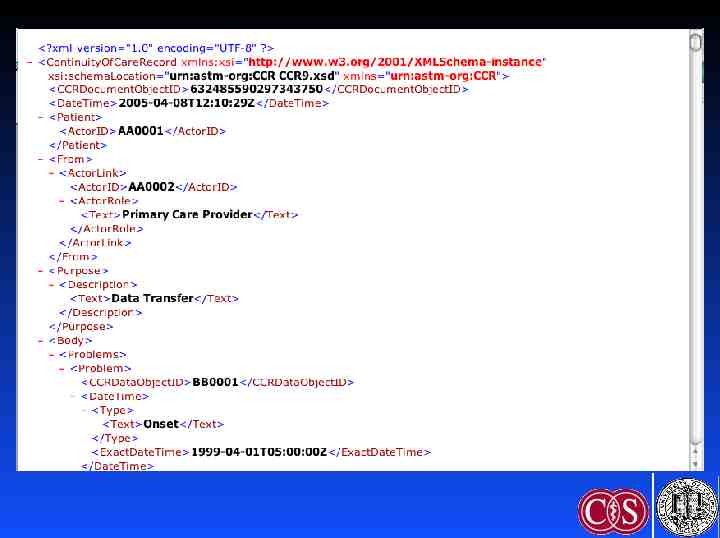
Improving Adoption: CCR ASTM E31 WK4363 (2004). Coalition AAP, AAFP, HIMSS, ACP, AMA, etc Defines the core data elements & content of the patient record in XML – Read/write standard data elements: Snapshot of the record – Therefore increases interoperability Uses: Record sharing, eRx (allergies, medications), certification Components: standard content; elements spreadsheet; implementation guide; XML schema
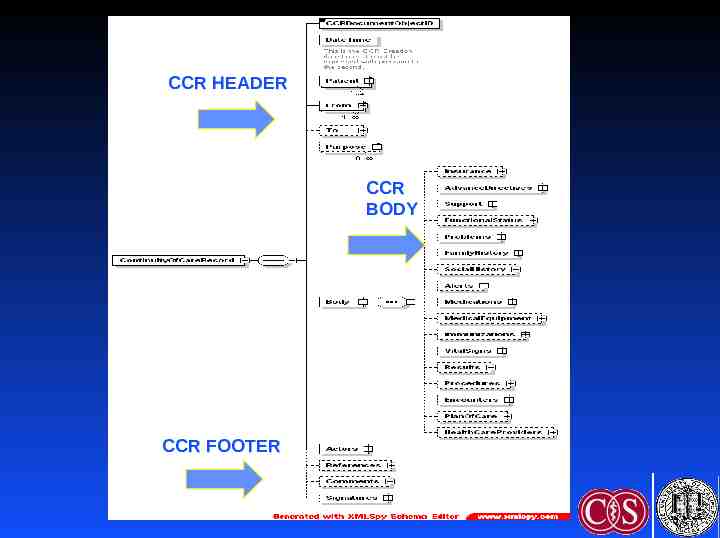
CCR HEADER CCR BODY CCR FOOTER
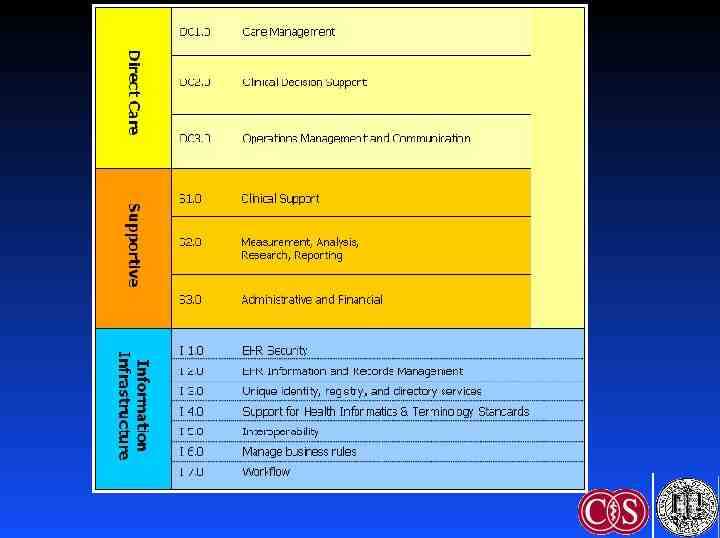
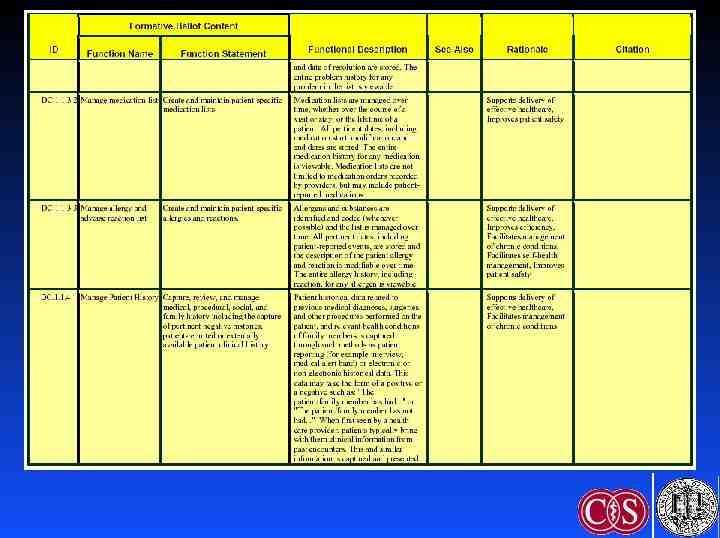
Improving Adoption: EHR Functional Model & Specification HL7 2004: Funded by US Government Identifies key functions of the EHR Purpose – Guide development by vendors – Facilitate certification – Facilitate interoperability Certification governance: CCHIT
Improving Adoption: DOQ-IT Doctor’s Office Quality - Information Technology – Outgrowth of CMS-funded QIOs – ACP, Lumetra, etc – Goal: Overcome barriers to EHR adoption Interventions – Expert advice: Needs assessment, vendor selection, case management, workflow integration – Peer-to-peer dialog: Share best practices – Does not provide funding, day-to-day assistance
Improving Adoption: Office VistA VistA: Veterans Information System Technology Architecture – M-based comprehensive VA EHR – Includes CPRS Computer-based Patient Record System Office VistA – Outpatient version – Due for release Q4 2005 (available under FOIA) Challenge: Free up front, but need to implement and maintain
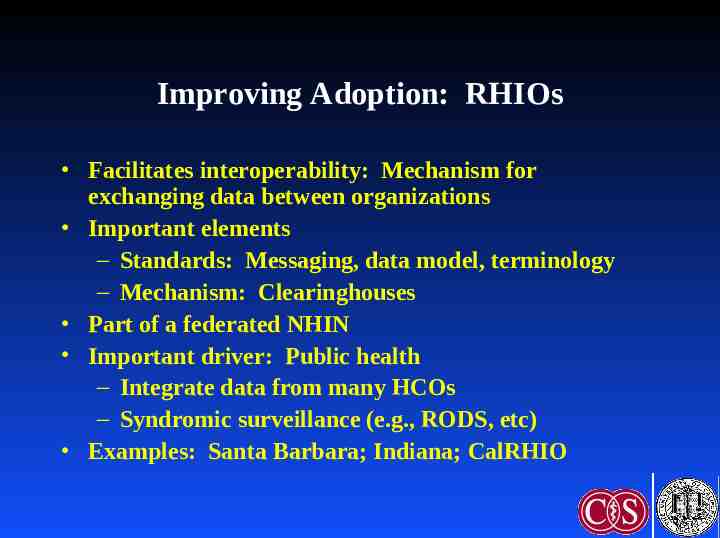
Improving Adoption: RHIOs Facilitates interoperability: Mechanism for exchanging data between organizations Important elements – Standards: Messaging, data model, terminology – Mechanism: Clearinghouses Part of a federated NHIN Important driver: Public health – Integrate data from many HCOs – Syndromic surveillance (e.g., RODS, etc) Examples: Santa Barbara; Indiana; CalRHIO
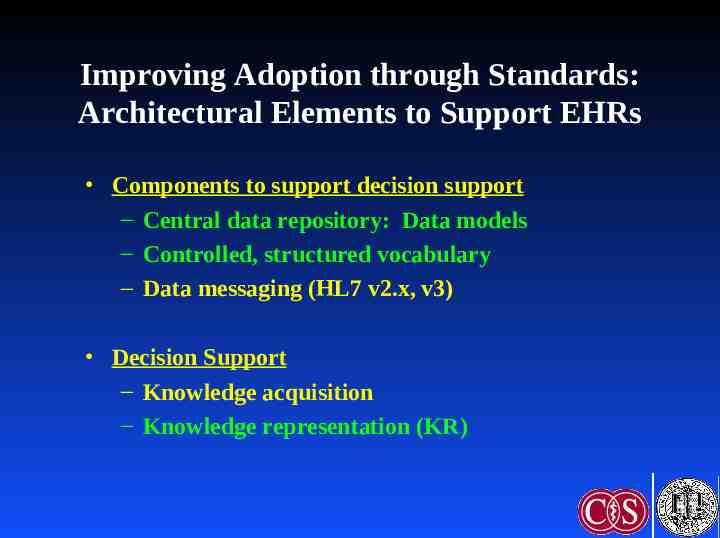
Improving Adoption through Standards: Architectural Elements to Support EHRs Components to support decision support – Central data repository: Data models – Controlled, structured vocabulary – Data messaging (HL7 v2.x, v3) Decision Support – Knowledge acquisition – Knowledge representation (KR)
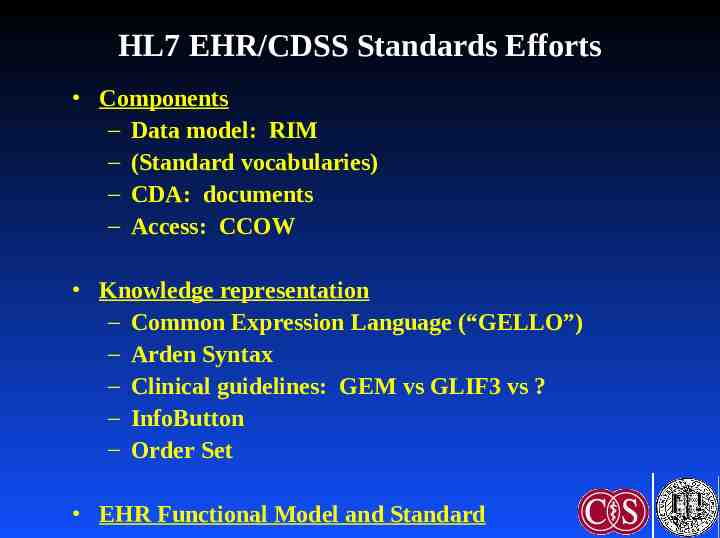
HL7 EHR/CDSS Standards Efforts Components – Data model: RIM – (Standard vocabularies) – CDA: documents – Access: CCOW Knowledge representation – Common Expression Language (“GELLO”) – Arden Syntax – Clinical guidelines: GEM vs GLIF3 vs ? – InfoButton – Order Set EHR Functional Model and Standard
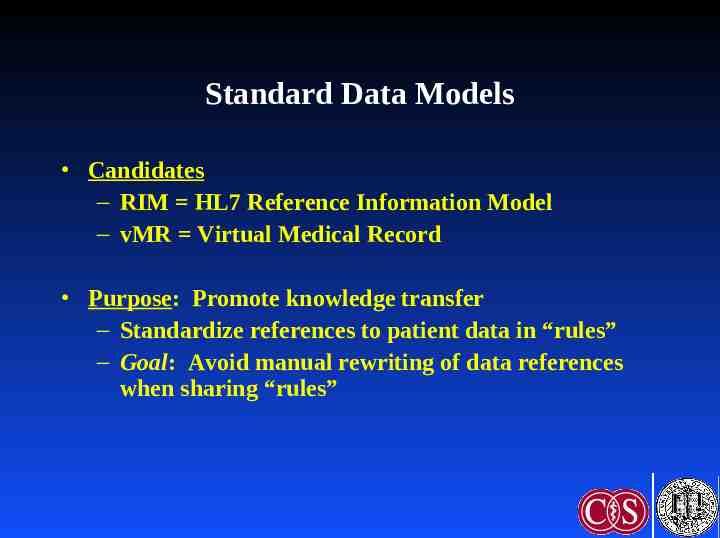
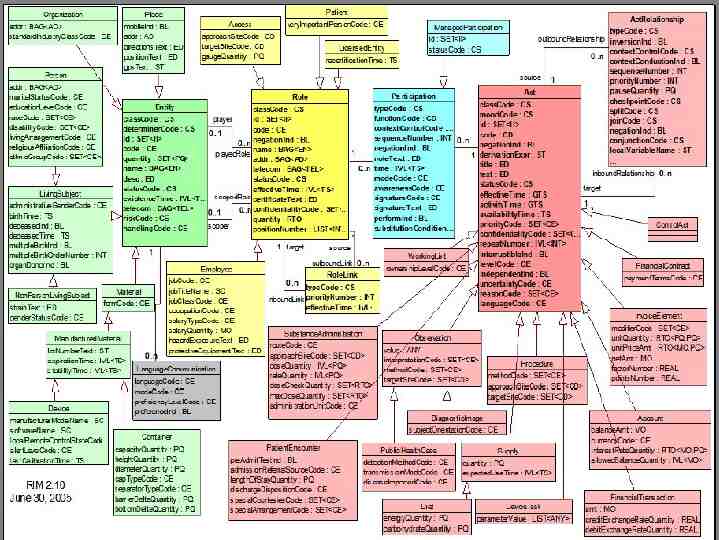
Standard Data Models Candidates – RIM HL7 Reference Information Model – vMR Virtual Medical Record Purpose: Promote knowledge transfer – Standardize references to patient data in “rules” – Goal: Avoid manual rewriting of data references when sharing “rules”
Standard Data Models: HL7 RIM High-level, abstract model of all exchangeable data – Concepts are objects: Act (e.g., observations), Living Subject, etc – Object attributes – Relationship among objects Common reference for all HL7 v3 standards Facilitates interoperability: Common model for messaging, queries Schadow G, Russler DC, Mead CN, McDonald CJ. Integrating medical information and knowledge in the HL7 RIM. Proc AMIA Symp 2000;:764-768.
Standard Vocabularies CHI NCVHS efforts: Patient Medical Record Information (PMRI) terminology standards Examples: SNOMED-CT, ICD-9, LOINC, CPT, etc Facilitation: Free licensing of SNOMED in USA as part of UMLS Use: HL7 Common Terminology Services (CTS) standard
Common Expression Language (GELLO) Purpose: Share queries and logical expressions – Query data (READ) – Logically manipulate data (IF-THEN, etc) Current work: GELLO (BWH) Guideline Expression Language Current status: ANSI standard release 1, May, 2005 Ogunyemi O, Zeng Q, Boxwala A. Object-oriented guideline expression language (GELLO) specification: Brigham and Women’s Hospital, Harvard Medical School, 2002. Decision Systems Group Technical Report DSG-TR-2002-001.
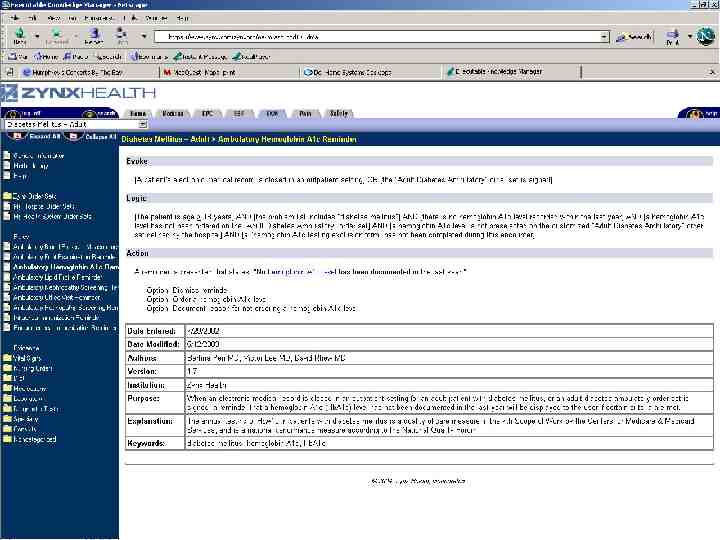
Arden Syntax ASTM v1 1992, HL7 v2 1999, v2.1 (ANSI) 2002, v2.5 2005 http://cslxinfmtcs.csmc.edu/hl7/arden/ Formalism for procedural medical knowledge Unit of representation Medical Logic Module (MLM) – Enough logic data to make a single decision – Generate alerts/reminders Adopted by several major vendors Jenders RA, Dasgupta B. Challenges in implementing a knowledge editor for the Arden Syntax: knowledge base maintenance and standardization of database linkages. Proc AMIA Symp 2002;:355-359.
Guideline Model: GLIF Guideline Interchange Format Origin: Study collaboration in medical informatics Now: GLIF3 – Very limited implementation Guideline Flowchart of temporally ordered steps – Decision & action steps – Concurrency: Branch & synchronization steps Peleg M, Ogunyemi O, Tu S et al. Using features of Arden Syntax with objectoriented medical data models for guideline modeling. Proc AMIA Symp 2001;:523-527.
GLIF (continued): Levels of Abstraction Conceptual: Flowchart Computable: Patient data, algorithm flow, clinical actions specified Implementable: Executable instructions with mappings to local data
Guideline Model: GEM Guideline Elements Model Current ASTM standard Mark up of a narrative guideline into structured format using XML – Not procedural programming – Tool GEM Cutter Resulting structure might be used to translate to executable version Shiffman RN, Agrawal A, Deshpande AM, Gershkovich P. An approach to guideline implementation with GEM. Proc Medinfo 2001;271-275.
GEM (continued) Model 100 discrete elements in 9 major branches – identity and developer, purpose, intended audience, development method, target population, testing, revision plan and knowledge components Iterative refinement: Adds elements not present verbatim but needed for execution Customization: Adding meta-knowledge – controlled vocabulary terms, input controls, prompts for data capture
Infobutton Standard Infobutton: software that mediates between an information system (EHR) and a knowledge source (electronic textbook, drug reference, etc) Goals – Standard interface to maximize access to knowledge sources – Tailored access to relevant bits Status: Under development (HL7).
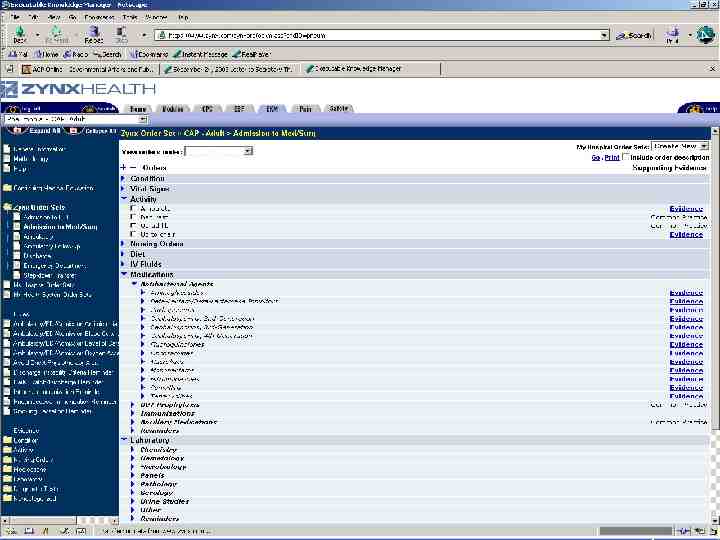
Order Set Standard Order Set: Document containing a group of orders for specific care episodes (disease states or presentations) – Examples: Admission for chest pain; communityacquired pneumonia Features – Checklist: Remind clinicians what to do – Advice: Provide therapeutic options, dosing, etc Goals: Allow selection of parts or all of order set within a CPOE system. Facilitate sharing. Current status (HL7): Under development
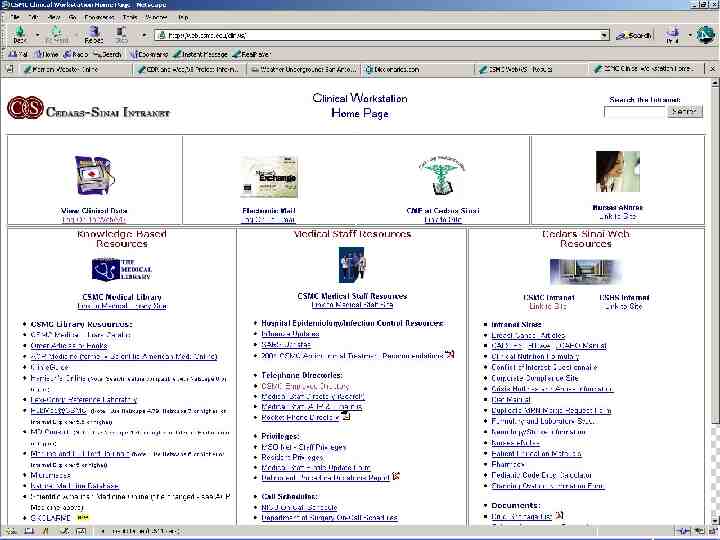
Case Study / Demonstration: Cedars-Sinai Medical Center
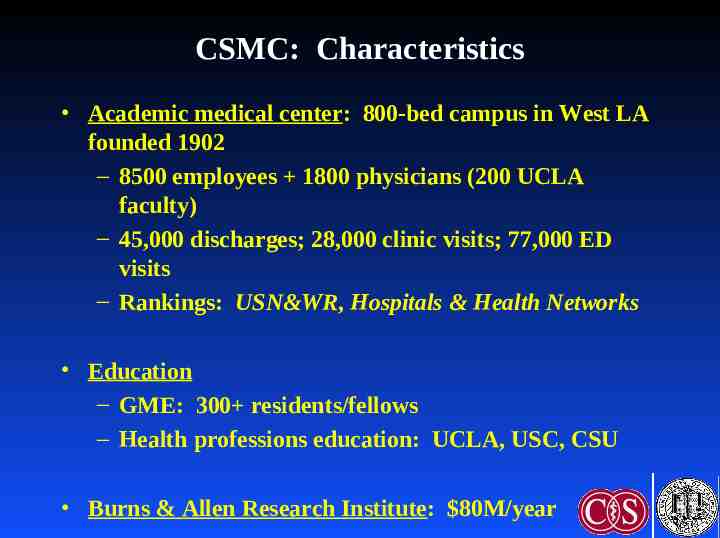
CSMC: Characteristics Academic medical center: 800-bed campus in West LA founded 1902 – 8500 employees 1800 physicians (200 UCLA faculty) – 45,000 discharges; 28,000 clinic visits; 77,000 ED visits – Rankings: USN&WR, Hospitals & Health Networks Education – GME: 300 residents/fellows – Health professions education: UCLA, USC, CSU Burns & Allen Research Institute: 80M/year
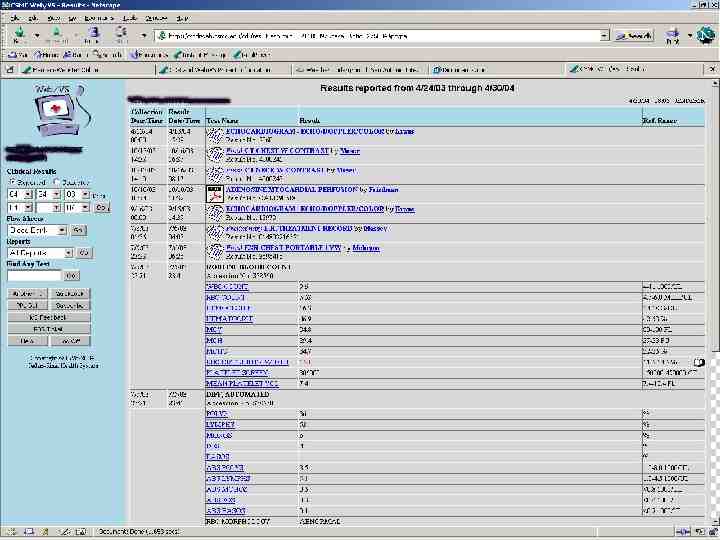
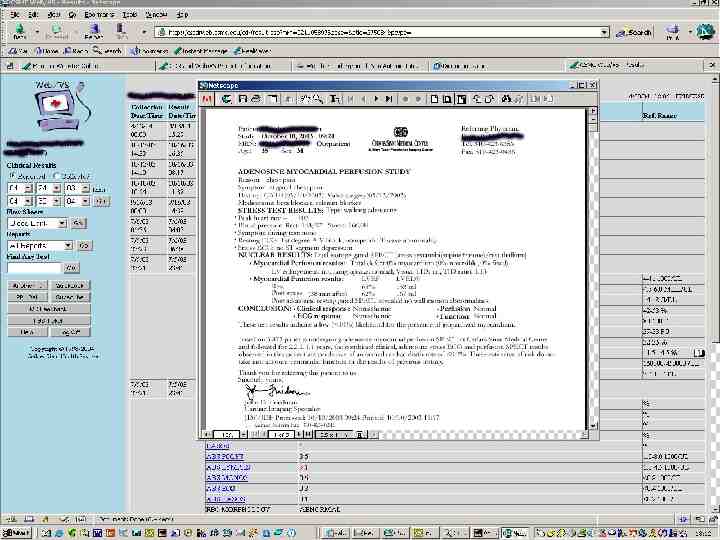
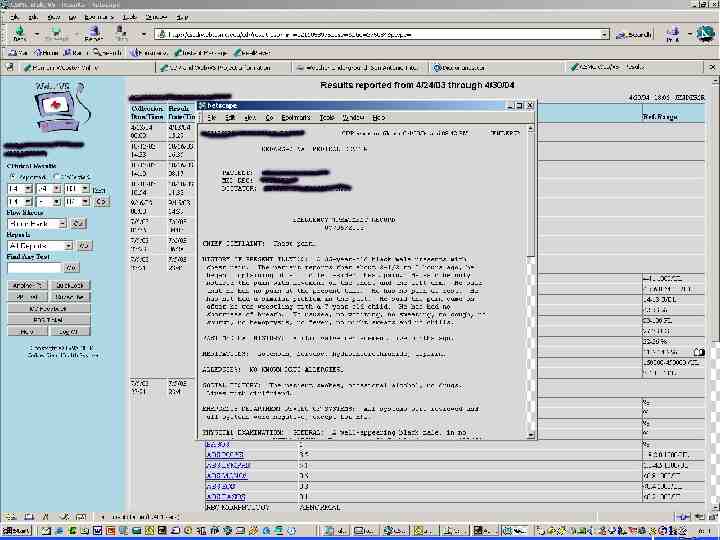
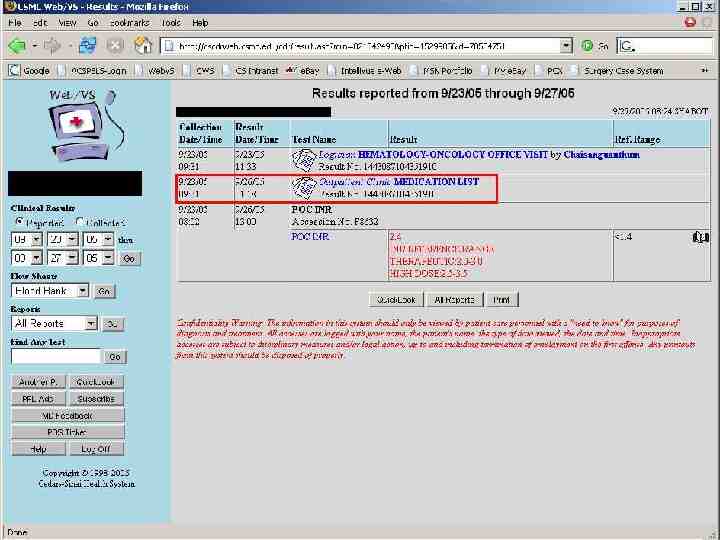
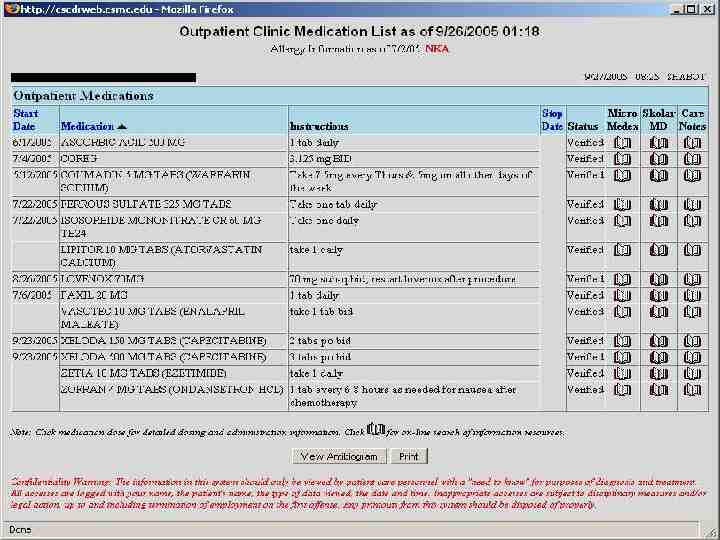
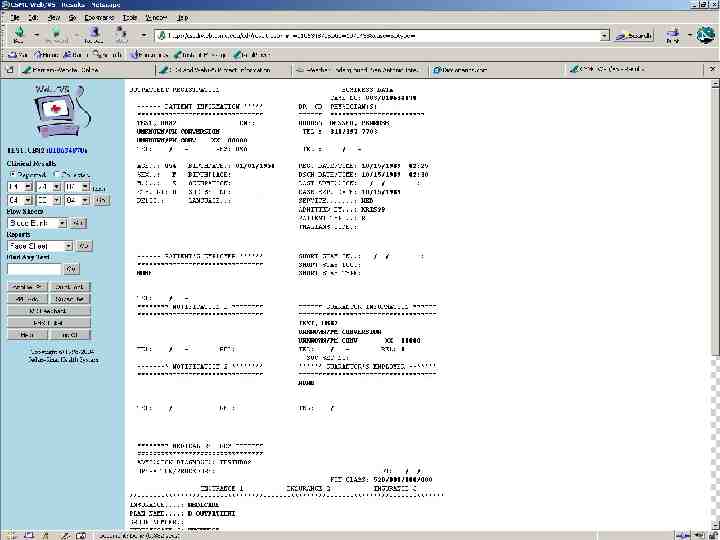
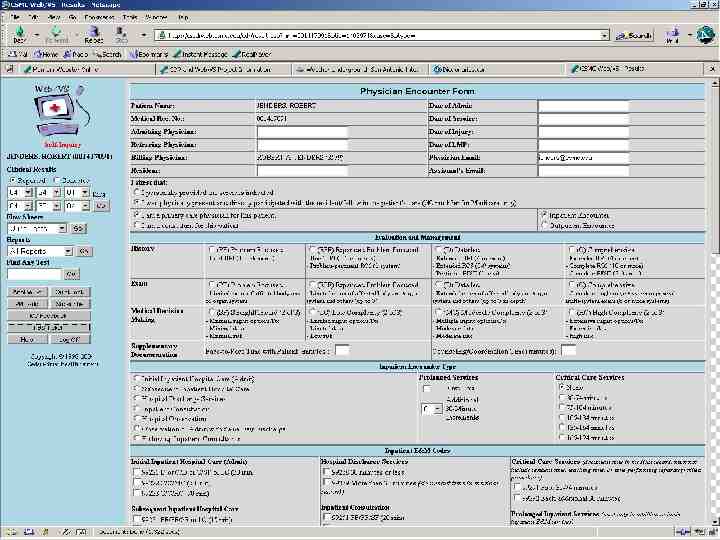
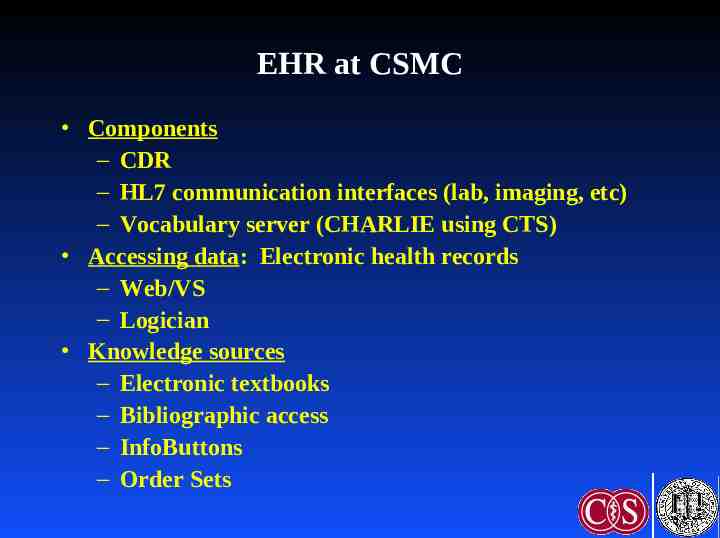
EHR at CSMC Components – CDR – HL7 communication interfaces (lab, imaging, etc) – Vocabulary server (CHARLIE using CTS) Accessing data: Electronic health records – Web/VS – Logician Knowledge sources – Electronic textbooks – Bibliographic access – InfoButtons – Order Sets
Web/VS CMA Laboratory Pharmacy Medical Logic Billing & Financial Database Interface CHARLIE (CTS) Radiology CDR Data Warehouse
Centricity Demonstration
Summary EHR needed – Many advantages, some disadvantages – Key: integration of data Aspects of the EHR: Functions, advantages, disadvantages Improving adoption – Standards, interoperability
Additional Resources Shortliffe Chapter 9 (new edition due 2006) Degoulet P, Fieschi M. Managing patient records. Chapter 9 in Introduction to Clinical Informaitcs. New York: SpringerVerlag, 1997;117-30. van Bemmel JH, Musen MA. The patient record (chapter 7) & Structuring the computer-based patient record (chapter 29) in Handbook of Medical Informatics. Houten, Netherlands: Springer, 1997. Bates DW, Ebell M, Gottlieb E et al. A proposal for electronic medical records U.S. primary care. J Am Med Inform Assoc 2003;10:1-10.
Additional Resources: Web www.astm.org www.hl7.org www.calrhio.org www.cchit.org
Thanks! [email protected] http://jenders.bol.ucla.edu - Documents & Presentations