Clinical Documentation Improvement Program Physician Program
7 Slides95.24 KB
Clinical Documentation Improvement Program Physician Program Overview Our CDI program works to ensure the documentation in the medical record captures the true acuity of our patients. Accurate documentation will reflect appropriate severity of illness and risk of mortality to support resource intensity and length of stay for our patients. If a CDI nurse recognizes the need for additional documentation, a question (query) will be presented to you. This packet is intended to give you a little more information behind the program.
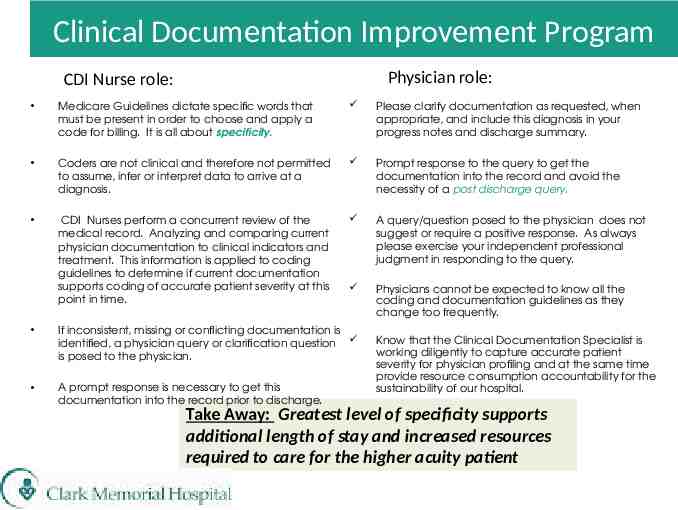
Clinical Documentation Improvement Program Physician role: CDI Nurse role: Medicare Guidelines dictate specific words that must be present in order to choose and apply a code for billing. It is all about specificity. Please clarify documentation as requested, when appropriate, and include this diagnosis in your progress notes and discharge summary. Coders are not clinical and therefore not permitted to assume, infer or interpret data to arrive at a diagnosis. Prompt response to the query to get the documentation into the record and avoid the necessity of a post discharge query. CDI Nurses perform a concurrent review of the medical record. Analyzing and comparing current physician documentation to clinical indicators and treatment. This information is applied to coding guidelines to determine if current documentation supports coding of accurate patient severity at this point in time. A query/question posed to the physician does not suggest or require a positive response. As always please exercise your independent professional judgment in responding to the query. Physicians cannot be expected to know all the coding and documentation guidelines as they change too frequently. If inconsistent, missing or conflicting documentation is identified, a physician query or clarification question is posed to the physician. A prompt response is necessary to get this documentation into the record prior to discharge. Know that the Clinical Documentation Specialist is working diligently to capture accurate patient severity for physician profiling and at the same time provide resource consumption accountability for the sustainability of our hospital. Take Away: Greatest level of specificity supports additional length of stay and increased resources required to care for the higher acuity patient
Clinical Documentation Improvement Program Query Process The physician is alerted of a query in SAC within the signature manager as an incomplete document when you log into SAC. Open the document, which will describe the clarification of documentation that is requested. Review, modify and save your response. If unable to answer at that time, close and return when able to determine. Questions or unclear of what to do contact the CDI nurse listed on the query. Sample cases to show how documentation clarification impacts your severity of illness (SOI), risk of mortality (ROM) and expected LOS (GMLOS)to follow.
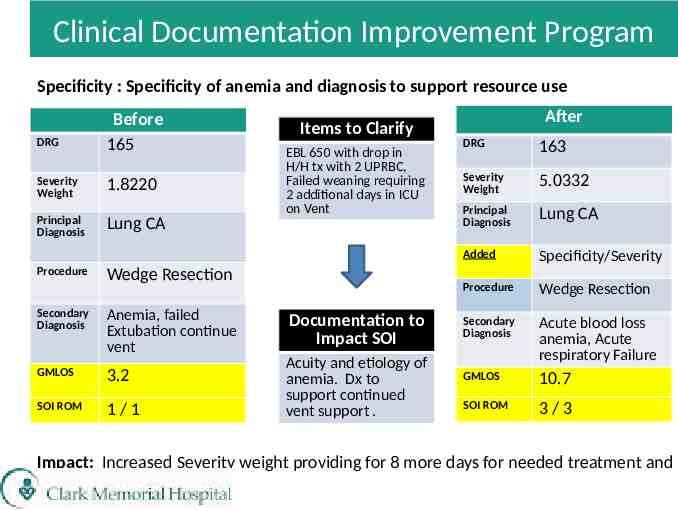
Clinical Documentation Improvement Program Specificity : Specificity of anemia and diagnosis to support resource use DRG Severity Weight Principal Diagnosis Procedure Before 165 1.8220 Lung CA Items to Clarify EBL 650 with drop in H/H tx with 2 UPRBC, Failed weaning requiring 2 additional days in ICU on Vent Wedge Resection Secondary Diagnosis Anemia, failed Extubation continue vent GMLOS 3.2 SOI ROM 1/1 Documentation to Impact SOI Acuity and etiology of anemia. Dx to support continued vent support . After DRG 163 Severity Weight 5.0332 Principal Diagnosis Lung CA Added Specificity/Severity Procedure Wedge Resection Secondary Diagnosis Acute blood loss anemia, Acute respiratory Failure GMLOS 10.7 SOI ROM 3/3 Impact: Increased Severity weight providing for 8 more days for needed treatment and resources
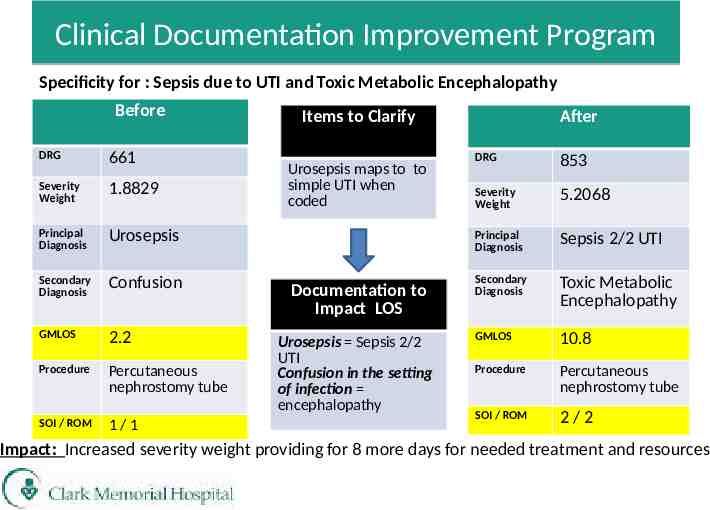
Clinical Documentation Improvement Program Specificity for : Sepsis due to UTI and Toxic Metabolic Encephalopathy Before DRG 661 Severity Weight 1.8829 Principal Diagnosis Urosepsis Secondary Diagnosis Confusion GMLOS 2.2 Procedure Percutaneous nephrostomy tube SOI / ROM 1/1 Items to Clarify Urosepsis maps to to simple UTI when coded Documentation to Impact LOS Urosepsis Sepsis 2/2 UTI Confusion in the setting of infection encephalopathy After DRG 853 Severity Weight 5.2068 Principal Diagnosis Sepsis 2/2 UTI Secondary Diagnosis Toxic Metabolic Encephalopathy GMLOS 10.8 Procedure Percutaneous nephrostomy tube SOI / ROM 2/2 Impact: Increased severity weight providing for 8 more days for needed treatment and resources
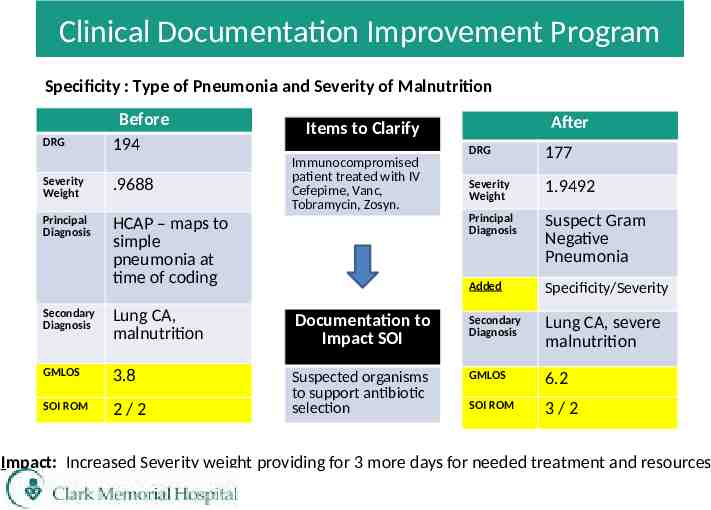
Clinical Documentation Improvement Program Specificity : Type of Pneumonia and Severity of Malnutrition DRG Before 194 Severity Weight .9688 Principal Diagnosis HCAP – maps to simple pneumonia at time of coding After Items to Clarify Immunocompromised patient treated with IV Cefepime, Vanc, Tobramycin, Zosyn. DRG 177 Severity Weight 1.9492 Principal Diagnosis Suspect Gram Negative Pneumonia Added Specificity/Severity Secondary Diagnosis Lung CA, malnutrition Documentation to Impact SOI Secondary Diagnosis Lung CA, severe malnutrition GMLOS 3.8 GMLOS 6.2 SOI ROM 2/2 Suspected organisms to support antibiotic selection SOI ROM 3/2 Impact: Increased Severity weight providing for 3 more days for needed treatment and resources
Clinical Documentation Improvement Program Thank you for taking time to review our program information. If you have questions or need additional information please contact one of our team: CDI Specialists: Vicki Byrd, LPN Debra Roth, RN Laura Steffey, RN Jan Hardy, RN 283-2137 283-2632 283-2137 283-2632 CDI Manager Lisa Strother, RN 283-2358 Medical Director William Templeton, MD 283-2777