Patient Care Delivery Chapter 5- Colleen Person
25 Slides63.00 KB
Patient Care Delivery Chapter 5- Colleen Person
Patient Care Delivery System A template for organizing and providing care to patients. The delivery system used is one of the most powerful tools a manager has in creating an environment of stability, with increased predictability and decreased uncertainty being by-products. (Marie Manthey) The purpose is to establish a therapeutic relationship between nurses and patients/families. The most effective care delivery systems are those designed with the patient always held in the highest regard.
Bureaucratic Nursing vs. Professional Nursing Nation wide movement from a task based view of care delivery to a principles-based, holistic view. Bureaucratic nursing: tasks drives activities, cure of disease, focus is on physical, diagnosis-centered care, policies and procedures drive decision making, rules, habits and routines determine nurse’s behavior
Professional Nursing Knowledge based, healing is the goal, focus is on holistic care, professional standards and current research drive decision making, critical thinking and innovation determine nurse’s behavior. Studies show that nursing care is the most important predictor of overall patient satisfaction with their hospital care
Designing Delivery Systems The authors base care delivery design on the following: Purpose- caring for patients/families Most effective when we know what matters most to each patient/family Patients share more when they feel safe Continuity of care improves productivity, efficiency, and patient and staff satisfaction Each element needs to be clearly defined
Elements of Care Delivery Systems Nurse/patient relationship and decision making: clearly define R A A How long does a relationship last between nurse and patient? Work allocation/patient assignments: How are staff scheduling, patient assignments, and delegation of care activities achieved?
Elements cont. Communication between members of the health care team: standards of communication Addresses values, beliefs, and group norms Management of unit /environment of care: unit manager creates the culture of care When all four elements are clearly defined a delivery system can function efficiently and effectively
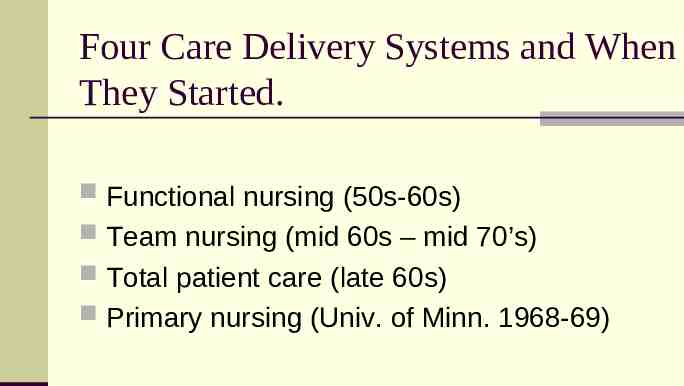
Four Care Delivery Systems and When They Started. Functional nursing (50s-60s) Team nursing (mid 60s – mid 70’s) Total patient care (late 60s) Primary nursing (Univ. of Minn. 1968-69)
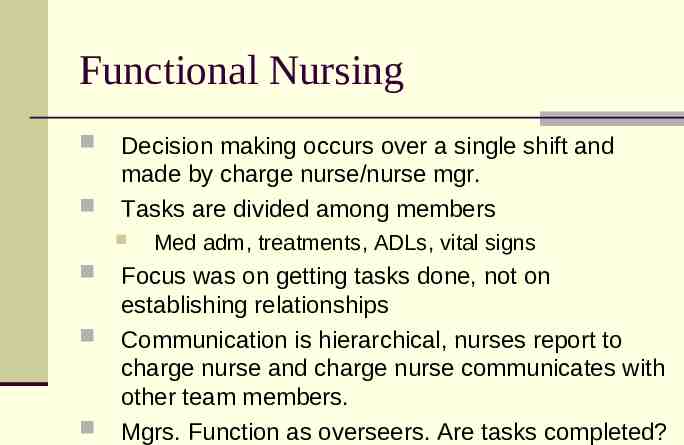
Functional Nursing Decision making occurs over a single shift and made by charge nurse/nurse mgr. Tasks are divided among members Med adm, treatments, ADLs, vital signs Focus was on getting tasks done, not on establishing relationships Communication is hierarchical, nurses report to charge nurse and charge nurse communicates with other team members. Mgrs. Function as overseers. Are tasks completed?
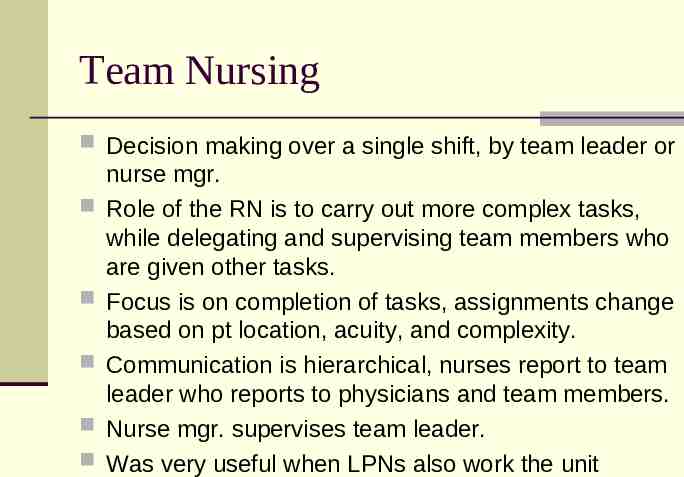
Team Nursing Decision making over a single shift, by team leader or nurse mgr. Role of the RN is to carry out more complex tasks, while delegating and supervising team members who are given other tasks. Focus is on completion of tasks, assignments change based on pt location, acuity, and complexity. Communication is hierarchical, nurses report to team leader who reports to physicians and team members. Nurse mgr. supervises team leader. Was very useful when LPNs also work the unit
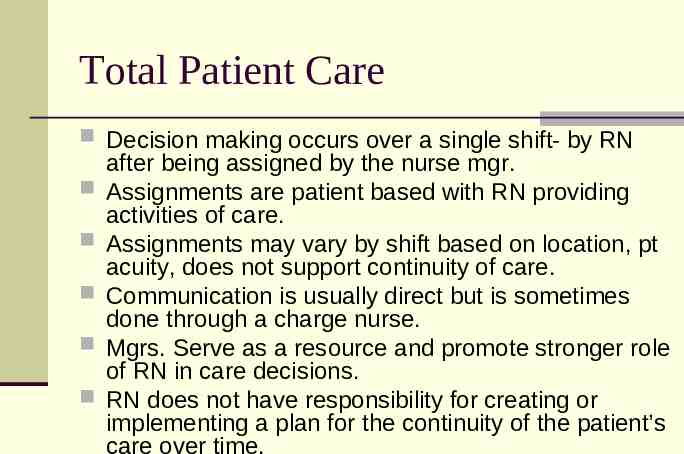
Total Patient Care Decision making occurs over a single shift- by RN after being assigned by the nurse mgr. Assignments are patient based with RN providing activities of care. Assignments may vary by shift based on location, pt acuity, does not support continuity of care. Communication is usually direct but is sometimes done through a charge nurse. Mgrs. Serve as a resource and promote stronger role of RN in care decisions. RN does not have responsibility for creating or implementing a plan for the continuity of the patient’s care over time.
Primary Nursing RN makes the decision for patients based on therapeutic relationship. Relationship is sustained for length of stay Assignments ensure continuity of care. Associate nurse takes care of pt when primary is not there. Communication is direct. Primary nurse is responsible for integrating information and coordinating care. Mgrs. Promote nurse/pt relationship. Create a healthy work environment and empower staff.
Role of RN in Primary Nursing RNs clearly accept responsibility for decision making regarding pt care, authority, and accountability. Determine and prioritizes needs of the pt/family, establishes an individualized plan of care, delegates tasks. Communicates and coordinates needs with other members of the health care team. RBC has evolved from the basic tenet of Primary nursing.
Partners in practice-New Concept RN, LPN, CNA agree to partner with one another in the provision of the activities of care. They choose to work together with consistent scheduling, building relationship, and focused around patient needs. RN is responsible for developing the knowledge and skill of his/her team It can work with the 12 hour shift, and supports continuity of care Reduces turnover of RNs, improves patient quality, promotes professional nursing.
Myths about Primary Nursing It requires an All RN staff: nurse extenders play a vital role in meeting needs of patients/families. The primary nurse does all the bedside care: their role is to accept RAA. It is not practical for RN to do all of bedside care. Primary nursing eliminates teamwork. You only know your patients: this model is based on a shared commitment to all patients. The nurse must work collaboratively. Complex scheduling requirements prohibit continuity of the nurse-patient-relationship central to the primary care model: scheduling must be creative. Nurses report perceived increase in productivity when continuity of care is supported.
Are all primary nursing models the same? Systems must be customized to what works for that individual organization. Each organization determines the best terminology with which to clarify R A A. The organization identifies key principles of each of the four elements
Role of the Consumer Health care consumers are becoming increasingly educated about nursing care and staffing issues. Find out the RN to patient ratio is managed by the acuity of the patients (Some suggest no greater than 1:4) Check also the ratio of RNs to LPNs Study the facility’s “report card.” (Leepfrog, JCAHO reports) Locate the nearest Magnet Hospital
Magnet Status Magnet hospitals have demonstrated: Ability to retain well qualified nursing staff; provide higher quality care; decrease error rates; decrease morbidity and mortality; Improved pt/family satisfaction (Aiken, Clarke, Sloane, Sochalski, & Silber, 2002; Ingersoll, Schultz, Hoffart, & Ryan, 1996; Prescott, 1993; Scott et al., 1999) Three goals of the Magnet Program: 1. 2. 3. Promoting quality in a setting that supports professional practice; Identifying excellence in the delivery of nursing services to patients/residents; and Disseminating “best practices” in nursing services.

Forces of magnetism Evolved out of a study conducted by the American Academy of Nursing’s Task Force ANCC provides programs and credentialing services to hospitals desiring to achieve Magnet Status http://www.nursecredentialing.org/ All of the standards are grounded in therapeutic, continuous relationship between the RN and patient.
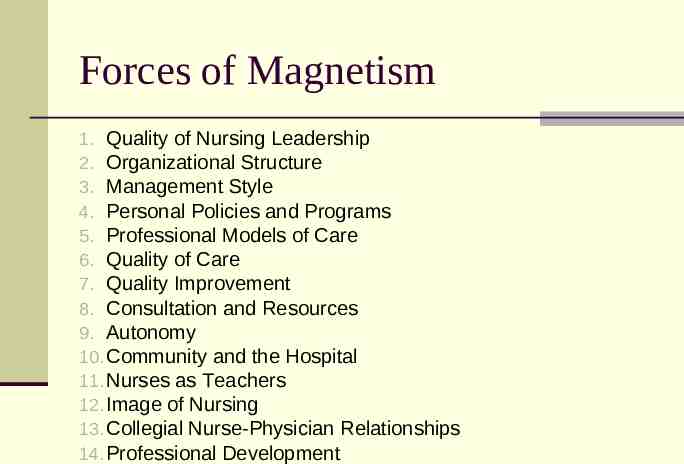
Forces of Magnetism 1. Quality of Nursing Leadership 2. Organizational Structure 3. Management Style 4. Personal Policies and Programs 5. Professional Models of Care 6. Quality of Care 7. Quality Improvement 8. Consultation and Resources 9. Autonomy 10. Community and the Hospital 11. Nurses as Teachers 12. Image of Nursing 13. Collegial Nurse-Physician Relationships 14. Professional Development
Transformational Leadership Forces #1 & #3 today's leaders are required to transform their organization's values, beliefs, and behaviors. This requires vision, influence, clinical knowledge, and a strong expertise relating to professional nursing practice. It also acknowledges that transformation may create turbulence and involve atypical approaches to solutions. The organization's senior leadership team creates the vision for the future, and the systems and environment necessary to achieve that vision. They must enlighten the organization as to why change is necessary, and communicate each department's part in achieving that change.
Structural Empowerment Forces #2, #4, #10, #12, #14 Staff need to be developed, directed, and empowered to find the best way to accomplish the organizational goals and achieve desired outcomes. This is accomplished through the organization's strategic plan, structure, systems, policies, and programs This may be accomplished through a variety of structures and programs; one size does not fit all.
Exemplary Professional Practice Forces #5, #8, #9, #11, #13 This entails a comprehensive understanding of the role of nursing; the application of that role with patients, families, communities, and the interdisciplinary team; and the application of new knowledge and evidence. The goal of this Component is more than the establishment of strong professional practice; it is what that professional practice can achieve.
New Knowledge, Innovation, & Improvements Force #7 Magnet organizations have an ethical and professional responsibility to contribute to patient care, the organization, and the profession in terms of new knowledge, innovations, and improvements. This Component includes new models of care, application of existing evidence, new evidence, and visible contributions to the science of nursing.
Empirical Quality Results Force #6 Magnet-recognized organizations are in a unique position to become pioneers of the future and to demonstrate solutions to numerous problems inherent in our healthcare systems today. They may do this in a variety of ways through innovative structure and various processes, and they ought to be recognized, not penalized, for their inventiveness. clinical outcomes related to nursing; workforce outcomes; patient and consumer outcomes; and organizational outcomes