Anesthesia Billing & Reimbursement Sho Me da Money Jerry Stonemetz MD
29 Slides385.90 KB
Anesthesia Billing & Reimbursement Sho Me da Money Jerry Stonemetz MD
Billing Basics There are many clinical settings within anesthesia that have unique billing concerns. – OB – Critical Care – Pain Management – PEC Here we will concentrate on billing for anesthesia for surgical procedures.
Billing Basics Every surgical procedure generates three fees – Facility Fee: charged by the hospital/surgical center for the OR and support services – Surgeon’s Professional Fee – Anesthesiologists Professional Fee
Billing Basics The each procedure has a certain value in units based on: – Surgical Procedure (Base Units) – Length of Procedure (Time Units) – Special Circumstances, Procedures or Techniques (Qualifying Circumstances Units) BU TU QCU Total Units
Billing Basics Our fee is then calculated by: – Total Units x Conversion Factor
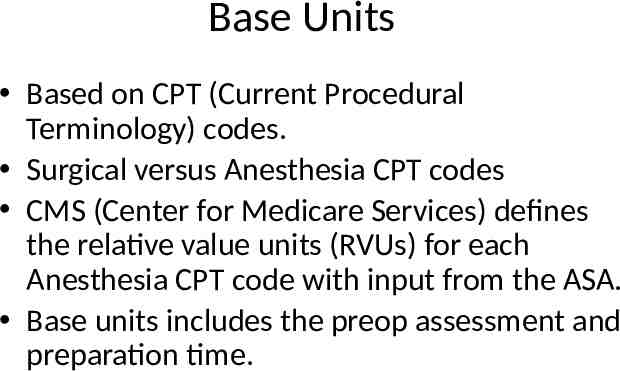
Base Units Based on CPT (Current Procedural Terminology) codes. Surgical versus Anesthesia CPT codes CMS (Center for Medicare Services) defines the relative value units (RVUs) for each Anesthesia CPT code with input from the ASA. Base units includes the preop assessment and preparation time.
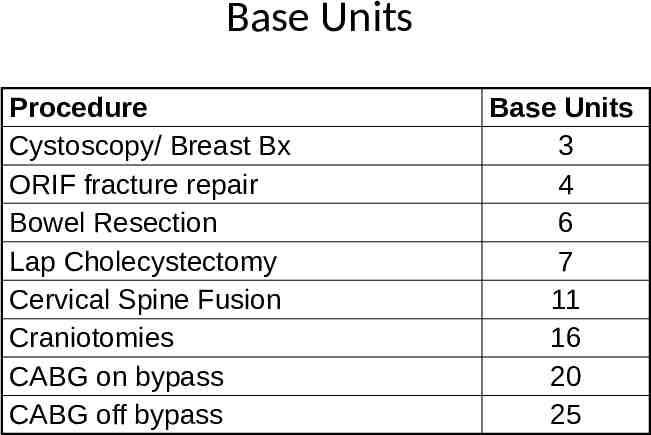
Base Units Procedure Cystoscopy/ Breast Bx ORIF fracture repair Bowel Resection Lap Cholecystectomy Cervical Spine Fusion Craniotomies CABG on bypass CABG off bypass Base Units 3 4 6 7 11 16 20 25
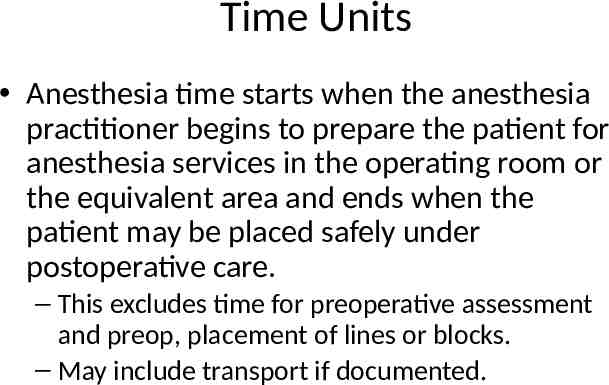
Time Units Anesthesia time starts when the anesthesia practitioner begins to prepare the patient for anesthesia services in the operating room or the equivalent area and ends when the patient may be placed safely under postoperative care. – This excludes time for preoperative assessment and preop, placement of lines or blocks. – May include transport if documented.
Time Units One time unit is equal to 15 mintues The CMS now effectively treats time units as a continuous variable, thus – 180 min 12 units – 185 min 12.33 units The time factor means each anesthetic is unique, making anesthesia billing the most complex in medicine.
Qualifying Circumstance/Modifiers Allows units for provision of anesthesia services under particularly difficult circumstances that necessitate the skills of a physician beyond those usually required. – Emergencies, deliberate hypotension, hypothermia. Allows units for certain specific procedures – Arterial lines, central lines, PA catheters, regional blocks (with GA), TEE
Conversion Factor Unless reimbursement is non-par, this is essentially determined by the payer. – Managed care organizations negotiate discounted conversion factors with participating providers. CMS is usually among the lowest. – Reimbursement for Medical Assistance is lower still. – Indigent typically No Pay.
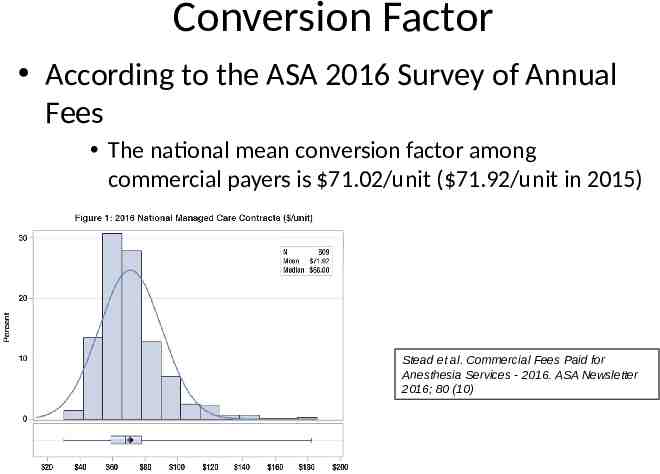
Conversion Factor According to the ASA 2016 Survey of Annual Fees The national mean conversion factor among commercial payers is 71.02/unit ( 71.92/unit in 2015) Stead et al. Commercial Fees Paid for Anesthesia Services - 2016. ASA Newsletter 2016; 80 (10)
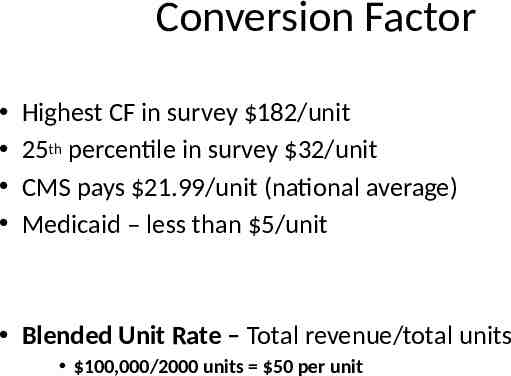
Conversion Factor Highest CF in survey 182/unit 25th percentile in survey 32/unit CMS pays 21.99/unit (national average) Medicaid – less than 5/unit Blended Unit Rate – Total revenue/total units 100,000/2000 units 50 per unit
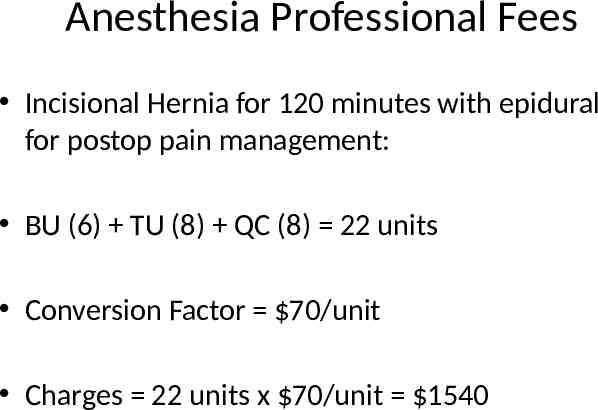
Anesthesia Professional Fees Incisional Hernia for 120 minutes with epidural for postop pain management: BU (6) TU (8) QC (8) 22 units Conversion Factor 70/unit Charges 22 units x 70/unit 1540
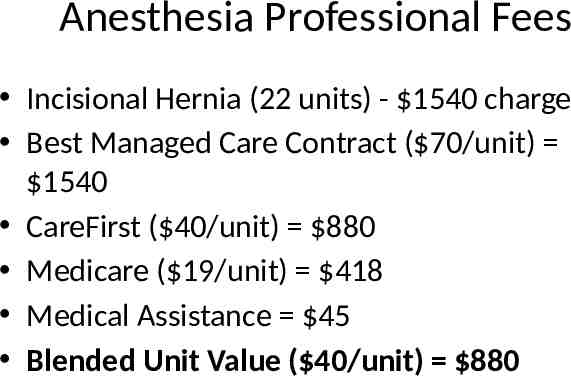
Anesthesia Professional Fees Incisional Hernia (22 units) - 1540 charge Best Managed Care Contract ( 70/unit) 1540 CareFirst ( 40/unit) 880 Medicare ( 19/unit) 418 Medical Assistance 45 Blended Unit Value ( 40/unit) 880
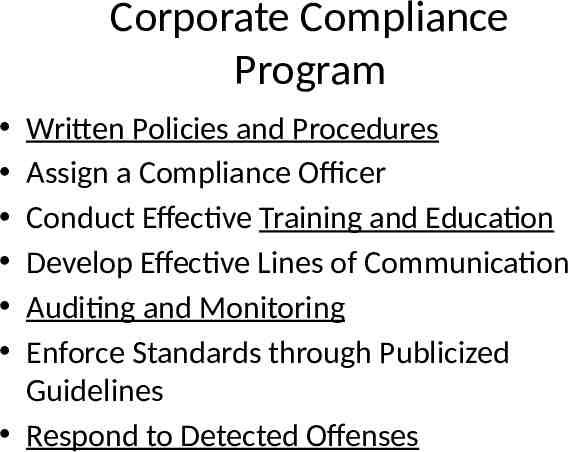
Corporate Compliance Program Written Policies and Procedures Assign a Compliance Officer Conduct Effective Training and Education Develop Effective Lines of Communication Auditing and Monitoring Enforce Standards through Publicized Guidelines Respond to Detected Offenses
Stonemetz Tip! Tip 1: When evaluating practices, ask what is the blended unit value. – Each group should know this value – Be very cautious accepting position unless you are reimbursed according to the blended unit value.
Distribution of Revenue How group revenue will be distributed to individual physicians can either be a straight salary or a productivity based compensation model. – Straight salary is often offered to new associates, while productivity based compensation is reserved for partners. Productivity based compensation models lie on a continuum between two extremes
Hunter Model You eat what you kill! Your income is based strictly on the revenue from the cases you do. Pros Strong incentive to increase efficiency and take on more challenging cases. Associated with high productivity. Cons Makes time spent on administrative duties, scholarly activities and overnight call relatively costly. The risk of patient to patient payer variability is taken on by individual physicians. This can be particularly costly for new and relatively naïve associates.
Time-Based Compensation Compensation is based on the number of hours or days worked. Pros – Easy to incorporate additional compensation for call, overtime, administrative time and scholarly work. – Spreads inter-patient payer risk. Cons – Less incentive for challenging cases and high efficiency. Associated with lower productivity.
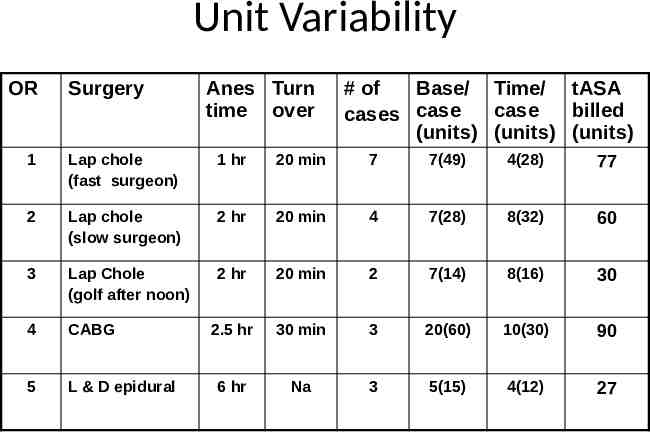
Unit Variability OR Surgery Anes Turn time over # of Base/ Time/ tASA case billed cases case (units) (units) (units) 1 Lap chole (fast surgeon) 1 hr 20 min 7 7(49) 4(28) 77 2 Lap chole (slow surgeon) 2 hr 20 min 4 7(28) 8(32) 60 3 Lap Chole (golf after noon) 2 hr 20 min 2 7(14) 8(16) 30 4 CABG 2.5 hr 30 min 3 20(60) 10(30) 90 5 L & D epidural 6 hr Na 3 5(15) 4(12) 27
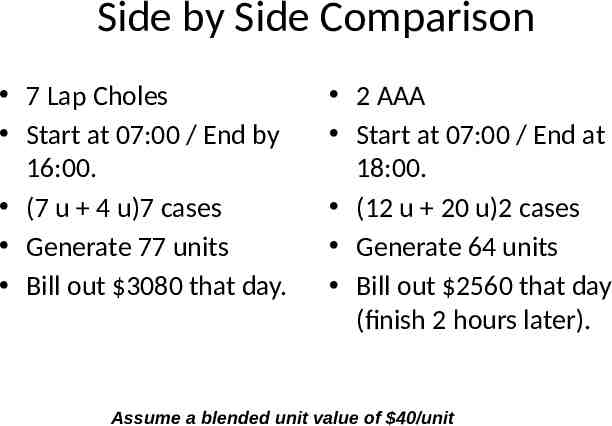
Side by Side Comparison 7 Lap Choles Start at 07:00 / End by 16:00. (7 u 4 u)7 cases Generate 77 units Bill out 3080 that day. 2 AAA Start at 07:00 / End at 18:00. (12 u 20 u)2 cases Generate 64 units Bill out 2560 that day (finish 2 hours later). Assume a blended unit value of 40/unit
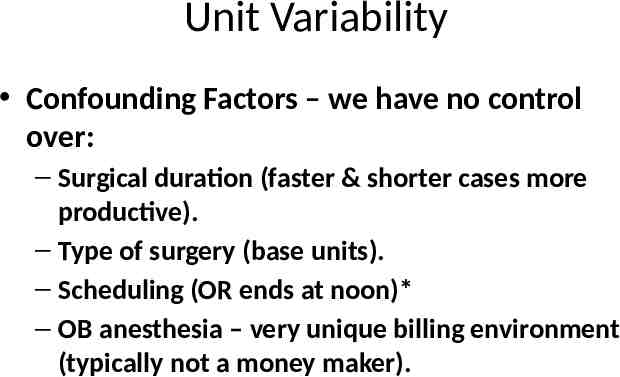
Unit Variability Confounding Factors – we have no control over: – Surgical duration (faster & shorter cases more productive). – Type of surgery (base units). – Scheduling (OR ends at noon)* – OB anesthesia – very unique billing environment (typically not a money maker).
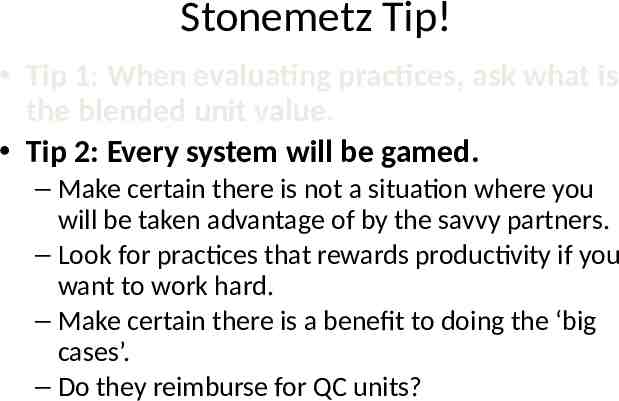
Stonemetz Tip! Tip 1: When evaluating practices, ask what is the blended unit value. Tip 2: Every system will be gamed. – Make certain there is not a situation where you will be taken advantage of by the savvy partners. – Look for practices that rewards productivity if you want to work hard. – Make certain there is a benefit to doing the ‘big cases’. – Do they reimburse for QC units?
Looking for a job Location! Location! Location! Check out the Payer Mix (demographics). Is very expensive to move after the first year (buy-in). What if there are no openings at the group you want to join? Do not use an agent to find a position. Every occupation becomes a job; Find your passion.
Type of Practice All MD practice – Lower income – Potentially higher malpractice risk All CRNA practice – High call percentage – Putting out fires Hybrid MD/CRNA – Highest income potential – Lower call percentage
Stonemetz Tip Tip 1: When evaluating practices, ask what is the blended unit value. Tip 2: Every system will be gamed. Tip 3: Make sure you like your partners. – A corporation is a marriage. – Divorce is always ugly. – The worse investment you will ever make is to choose the wrong spouse or wrong partners.
Contract Negotiation Do not hire an attorney! Look for: – Group needs to purchase your malpractice tail regardless of reason you leave. – Watch out for non-competes. Do your negotiations on the Addendum (Attachment), not the body of the contract. Save the attorney for the partnership agreement.

Happy Hunting!!