Alcohol Withdrawal Syndrome: Assessment, Documentation, and
25 Slides1,010.98 KB
Alcohol Withdrawal Syndrome: Assessment, Documentation, and Treatment options May 2019
OBJECTIVES Introduce the PAWSS score Discuss documentation requirements for CIWA-ar Identify treatment strategies including different medications with proper dosing
Pathophysiology of AWS Abrupt cessation of alcohol exposure Over activity of NMDA receptors Decreased inhibitory activity due to downregulation at GABA receptors Increased activity of dopamine

Clinical Manifestations Clinical spectrum – Hangover – Tremor – Hallucinations – Abnormal movements – Seizures – Delirium tremens
Alcohol Withdrawal Syndrome Early withdrawal: 6h after cessation; last 448h – Symptoms are autonomic (tremor, hyperactivity, insomnia, HA) – Minor: pts always have intact orientation and conscious – Moderate: hallucinations and illusions while conscious, can last up to 6 days
Withdrawal seizures Early phase of withdrawal 90% occur within 48h of cessation Most pts have repeated seizures Up to 5% may progress to status epilepticus Strong risk factor for progression to DTs Seizure occurring later than 48h suggest other causes (head trauma, combined drug withdrawal)
Delirium Tremens Appear 48-72h p cessation; may last for 2wks Acute onset Global confusion, hallucinations, autonomic overactivity, tremor, fever, agitation, diaphoresis Hypoactive delirium: decreased arousal and psychomotor activity – Associated with worse prognosis, delayed dx
Risk factors for developing severe AWS Previous episodes of alcohol withdrawal Previous alcohol withdrawal seizures History of delirium tremens History of alcohol rehabilitation treatment Previous episodes of blackouts Concomitant use of CNS-depressant agents or illicit drugs Recent alcohol intoxication Blood Alcohol Level 200mg/dL Evidence of increased autonomic activity
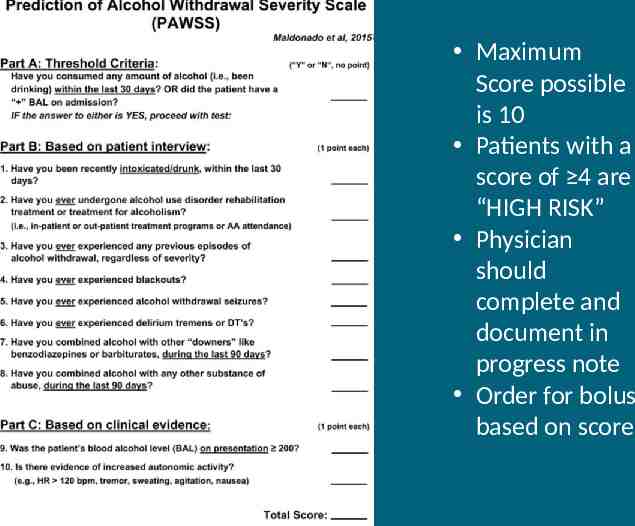
Maximum Score possible is 10 Patients with a score of 4 are “HIGH RISK” Physician should complete and document in progress note Order for bolus based on score
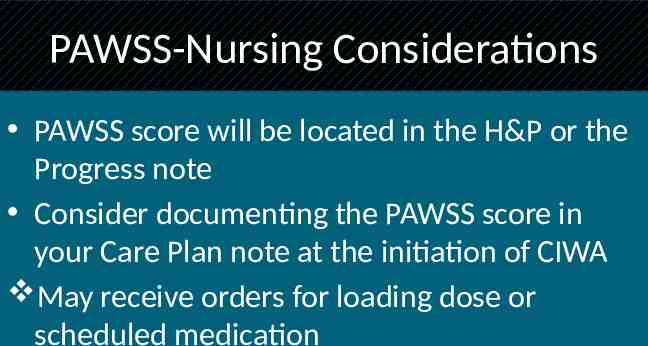
PAWSS-Nursing Considerations PAWSS score will be located in the H&P or the Progress note Consider documenting the PAWSS score in your Care Plan note at the initiation of CIWA May receive orders for loading dose or scheduled medication
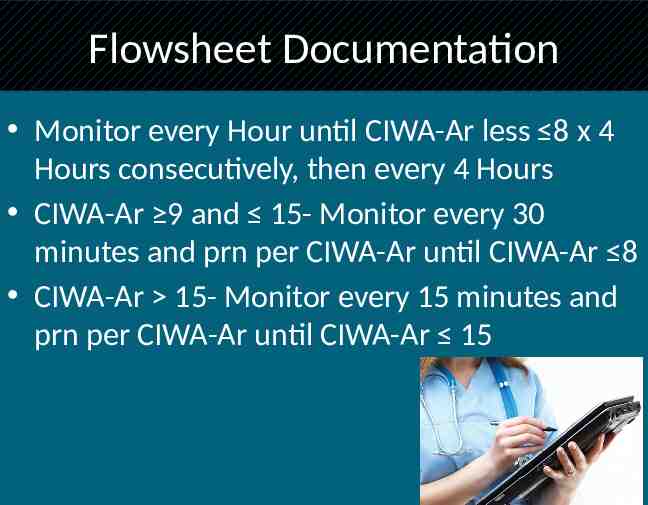
Flowsheet Documentation Monitor every Hour until CIWA-Ar less 8 x 4 Hours consecutively, then every 4 Hours CIWA-Ar 9 and 15- Monitor every 30 minutes and prn per CIWA-Ar until CIWA-Ar 8 CIWA-Ar 15- Monitor every 15 minutes and prn per CIWA-Ar until CIWA-Ar 15
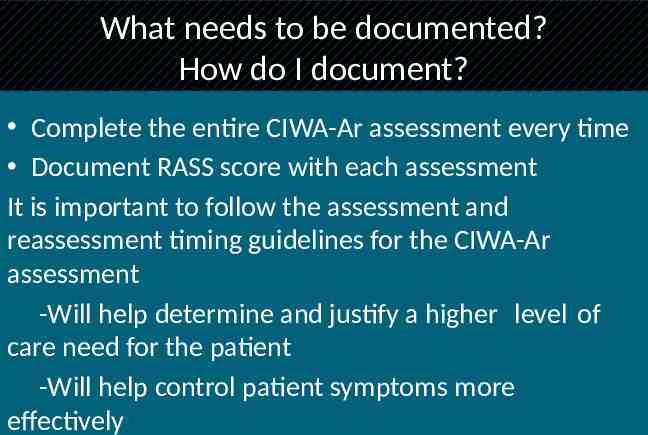
What needs to be documented? How do I document? Complete the entire CIWA-Ar assessment every time Document RASS score with each assessment It is important to follow the assessment and reassessment timing guidelines for the CIWA-Ar assessment -Will help determine and justify a higher level of care need for the patient -Will help control patient symptoms more effectively
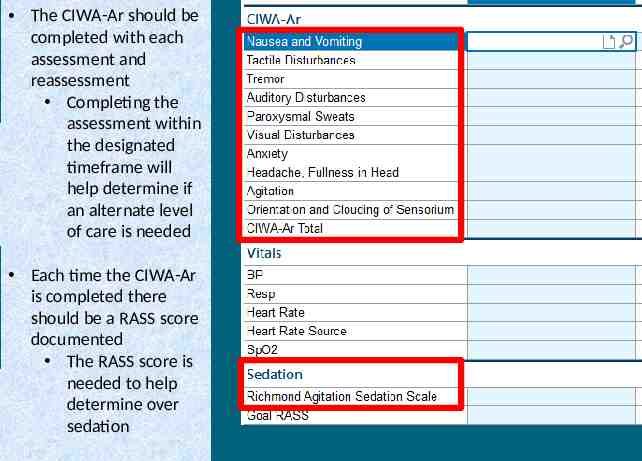
The CIWA-Ar should be completed with each assessment and reassessment Completing the assessment within the designated timeframe will help determine if an alternate level of care is needed Each time the CIWA-Ar is completed there should be a RASS score documented The RASS score is needed to help determine over sedation
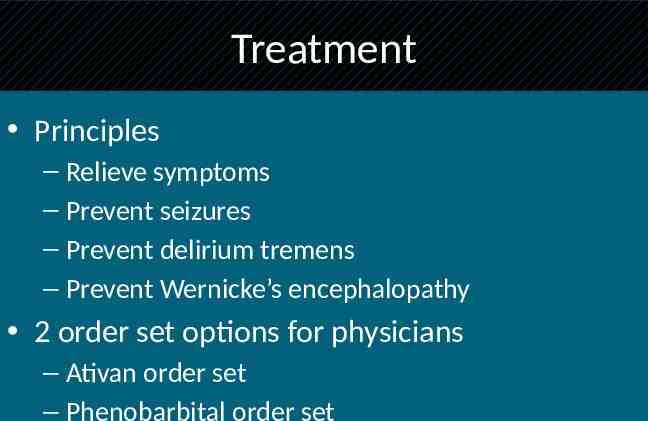
Treatment Principles – Relieve symptoms – Prevent seizures – Prevent delirium tremens – Prevent Wernicke’s encephalopathy 2 order set options for physicians – Ativan order set – Phenobarbital order set
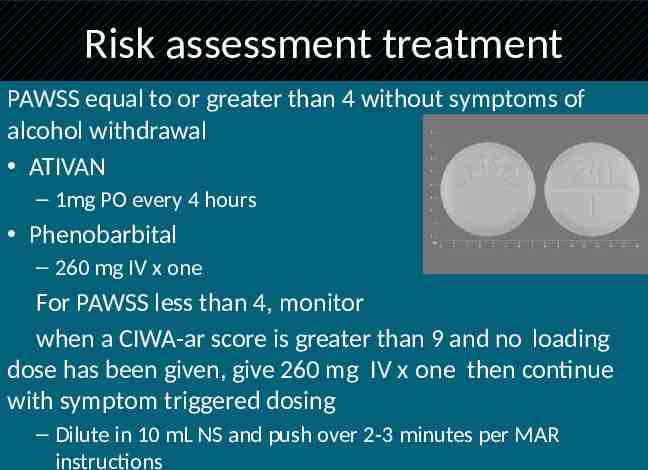
Risk assessment treatment PAWSS equal to or greater than 4 without symptoms of alcohol withdrawal ATIVAN – 1mg PO every 4 hours Phenobarbital – 260 mg IV x one For PAWSS less than 4, monitor when a CIWA-ar score is greater than 9 and no loading dose has been given, give 260 mg IV x one then continue with symptom triggered dosing – Dilute in 10 mL NS and push over 2-3 minutes per MAR instructions
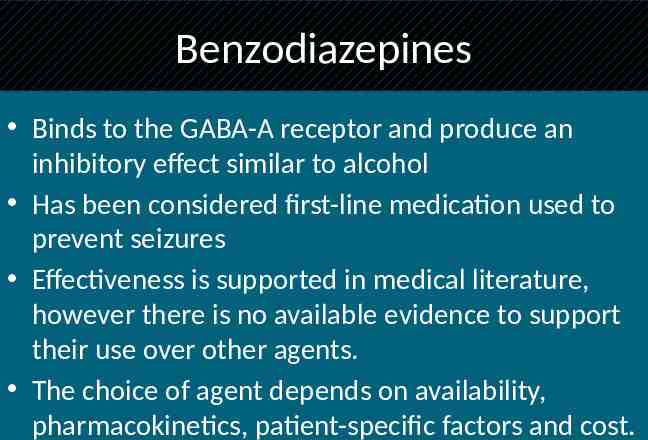
Benzodiazepines Binds to the GABA-A receptor and produce an inhibitory effect similar to alcohol Has been considered first-line medication used to prevent seizures Effectiveness is supported in medical literature, however there is no available evidence to support their use over other agents. The choice of agent depends on availability, pharmacokinetics, patient-specific factors and cost.
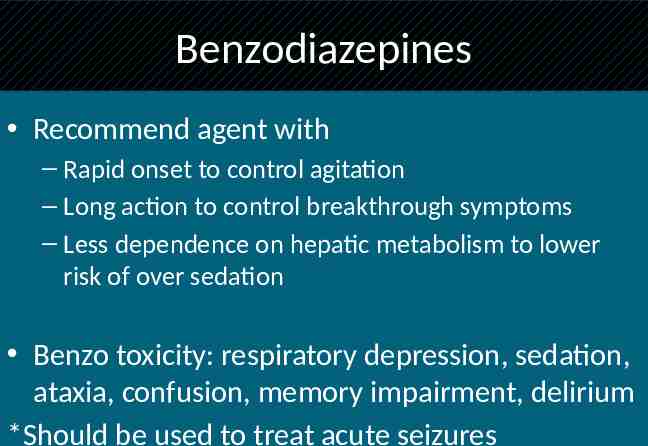
Benzodiazepines Recommend agent with – Rapid onset to control agitation – Long action to control breakthrough symptoms – Less dependence on hepatic metabolism to lower risk of over sedation Benzo toxicity: respiratory depression, sedation, ataxia, confusion, memory impairment, delirium *Should be used to treat acute seizures
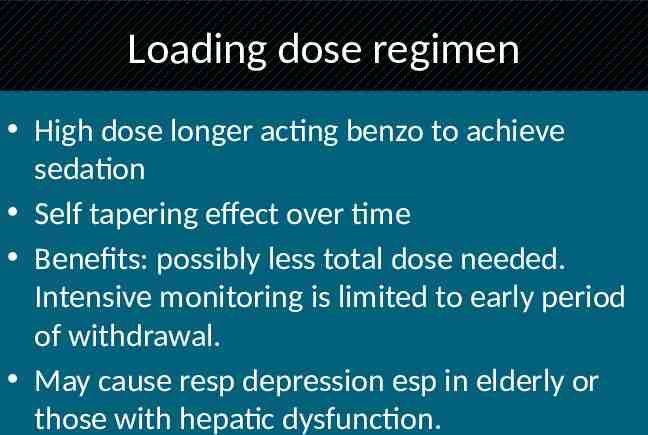
Loading dose regimen High dose longer acting benzo to achieve sedation Self tapering effect over time Benefits: possibly less total dose needed. Intensive monitoring is limited to early period of withdrawal. May cause resp depression esp in elderly or those with hepatic dysfunction.
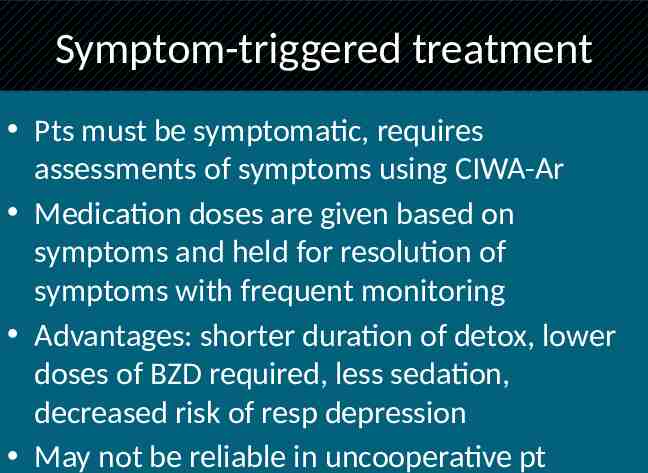
Symptom-triggered treatment Pts must be symptomatic, requires assessments of symptoms using CIWA-Ar Medication doses are given based on symptoms and held for resolution of symptoms with frequent monitoring Advantages: shorter duration of detox, lower doses of BZD required, less sedation, decreased risk of resp depression May not be reliable in uncooperative pt
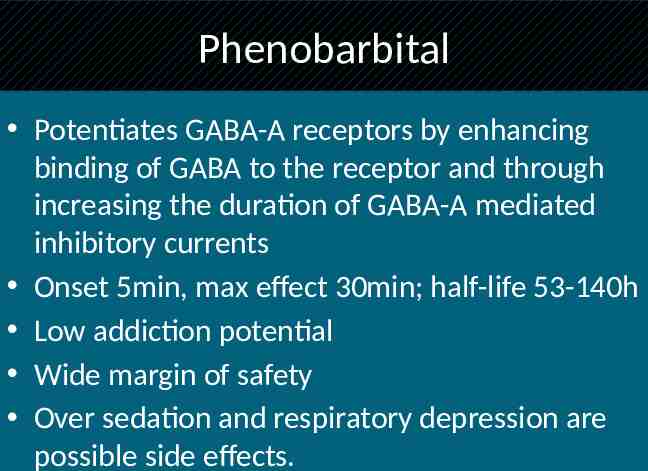
Phenobarbital Potentiates GABA-A receptors by enhancing binding of GABA to the receptor and through increasing the duration of GABA-A mediated inhibitory currents Onset 5min, max effect 30min; half-life 53-140h Low addiction potential Wide margin of safety Over sedation and respiratory depression are possible side effects.
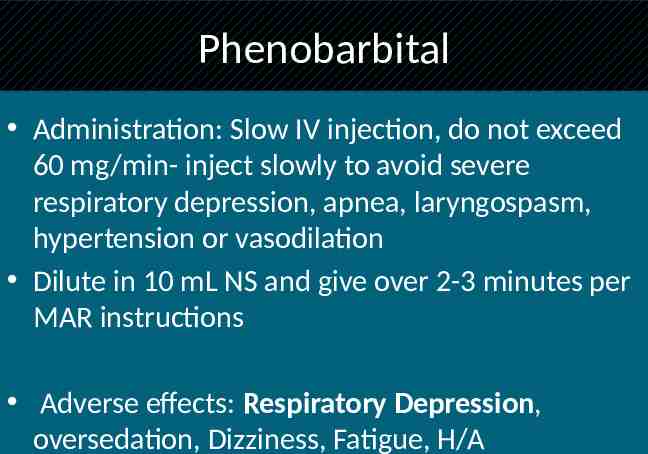
Phenobarbital Administration: Slow IV injection, do not exceed 60 mg/min- inject slowly to avoid severe respiratory depression, apnea, laryngospasm, hypertension or vasodilation Dilute in 10 mL NS and give over 2-3 minutes per MAR instructions Adverse effects: Respiratory Depression, oversedation, Dizziness, Fatigue, H/A
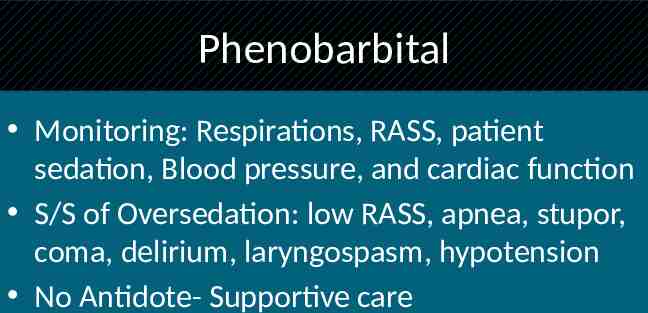
Phenobarbital Monitoring: Respirations, RASS, patient sedation, Blood pressure, and cardiac function S/S of Oversedation: low RASS, apnea, stupor, coma, delirium, laryngospasm, hypotension No Antidote- Supportive care
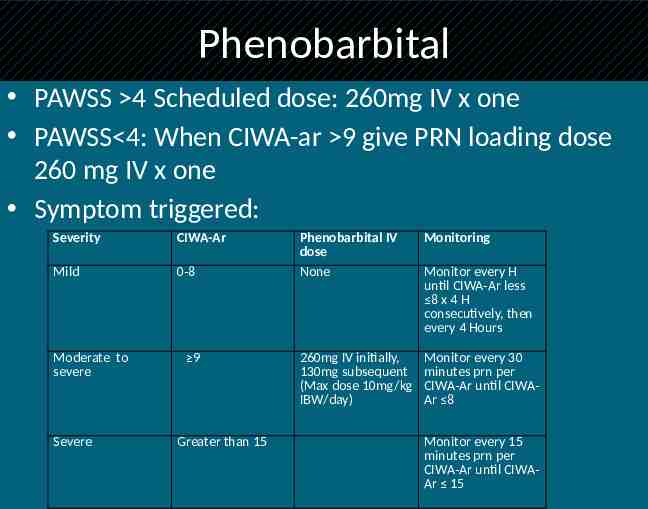
Phenobarbital PAWSS 4 Scheduled dose: 260mg IV x one PAWSS 4: When CIWA-ar 9 give PRN loading dose 260 mg IV x one Symptom triggered: Severity CIWA-Ar Mild 0-8 Moderate to severe Severe 9 Greater than 15 Phenobarbital IV dose None Monitoring 260mg IV initially, 130mg subsequent (Max dose 10mg/kg IBW/day) Monitor every 30 minutes prn per CIWA-Ar until CIWAAr 8 Monitor every H until CIWA-Ar less 8 x 4 H consecutively, then every 4 Hours Monitor every 15 minutes prn per CIWA-Ar until CIWAAr 15
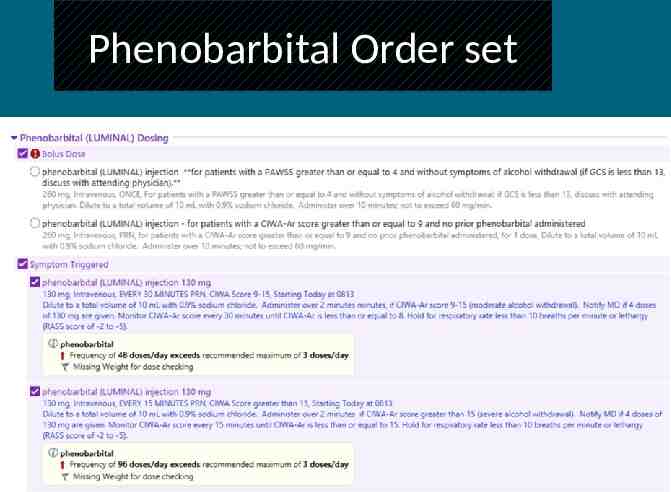
Phenobarbital Order set
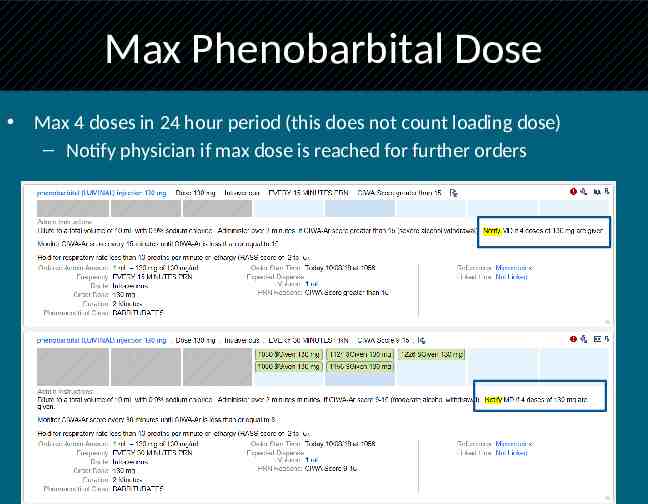
Max Phenobarbital Dose Max 4 doses in 24 hour period (this does not count loading dose) – Notify physician if max dose is reached for further orders