A Brief Introduction to Dialectical Behaviour Therapy Dr.
70 Slides358.44 KB
A Brief Introduction to Dialectical Behaviour Therapy Dr. Nathalie Lovasz, C.Psych (Supervised Practice) Head of Adult DBT Program – The Mindfulness Clinic Dr. Andrew Spice, C.Psych (Supervised Practice) Head of Adolescent DBT Program – The Mindfulness Clinic

Agenda Overview of DBT – Definition, development, research, adaptations Section 1: Assessment and Case Conceptualization Areas of Dysregulation: Signs that DBT may be helpful Theoretical model Stages of treatment; organizing treatment targets hierarchically Section 2: Treatment Core treatment strategies: Validation and chain analysis DBT Skills – Distress Tolerance – Emotion Regulation – Interpersonal Effectiveness – Mindfulness Section 3: Additional Issues in DBT – DBT and Other Professionals – Recommended Readings – Further Training
What is DBT? Comprehensive cognitive-behavioural treatment – Developed by Dr. Marsha Linehan at University of Washington – Originally developed to treat chronically suicidal clients diagnosed with Borderline Personality Disorder – Found to be effective for suicidal clients with multiple other co-occurring behavioural problems
Development of DBT CBT did not work for clients with chronic suicidality and BPD – Change focus was invalidating – Clients unintentionally reinforced therapists for behaviours that were not helpful and punished/extinguished helpful behaviours – Unrelenting crisis interfered with treatment/skills acquisition Solutions: Validation, Dialectics, Treatment Hierarchy, Multi-modal treatment
Research Findings DBT has been found to reduce – Suicidality – Parasuicidal behavior – Treatment drop-out – Hospitalizations – Substance Use – Depression, Hopelessness, Anger (Linehan et al., 1991;1999; Koons et al., 2001, Verheul et al., 2003)
Adaptations of DBT Substance Use Adolescents/Children Binge Eating Bipolar Disorder Couples Inpatient
Components of a DBT Program 1. 2. 3. 4. Individual (DBT) Therapy Weekly Skills Training Group Phone Coaching Therapist Consultation Team DBT-informed Therapy: - Any treatment that does not include ALL FOUR of the above components - E.g. CBT therapy that incorporates some DBT skills Group only Skills Training Skills Group Individual Therapy without Phone Coaching Skills Group, Individual Therapy, Phone Coaching but no consultation team

Assessment and Case Conceptualization
Symptoms of Borderline Personality Disorder Emotion Dysregulation – Unstable Emotions/Mood – Intense Anger/Difficulty Controlling Anger Interpersonal Dysregulation – Unstable/Intense Relationships – Frantic Efforts to Avoid Abandonment Behavioural Dysregulation – Impulsive/Self-Damaging Behaviours – Suicide/Self-harm Identity/Self Dysregulation – Unstable Sense of Self/Identity – Feelings of Emptiness Cognitive Dysregulation – Stress Related Paranoid Thoughts – Dissociation
Practice 1 Identify Areas of Dysregulation in a Practice Case Choose one of the two case vignettes provided. Identify as many areas of dysregulation as possible in the case vignette: Emotion Interpersonal Cognitive Behavioural Identity/Self
Biosocial Model of BPD EMOTIONAL VULNERABILITY Emotional Sensitivity: More easily triggered emotions – Responding with intense emotions to things that may not cause any emotion for someone else – “Thinner emotional skin” Emotional Reactivity: More intense emotions – Higher emotional baseline Slow Return to Baseline: Emotions that stick around longer
Biosocial Model of BPD INVALIDATION Emotional Fit: It can be difficult for people with less intense emotions to understand or teach those with more intense emotions how to manage their emotions Denial/Suppression of Emotions: With more intense emotions, people either doubt and ignore their emotions until they explode or become more intense in emotional expressions Reciprocal Effects: Emotions that are more intense than average are more likely to be dismissed by others Absence/Abuse/Neglect: These can also teach people to ignore, doubt, or push away emotions
Biosocial Model of BPD EMOTIONAL VULNERABILITY INVALIDATION BORDERLINE PERSONALITY DISORDER
Practice 2 Apply the Biosocial Model to a Practice Case Choose one of the vignettes provided. Identify any information you have that applies to the Biosocial Model: Emotional Vulnerability Experiences of Invalidation

Stages of Treatment Stage I: Stabilization – Focus: Treatment Hierarchy: – – – – Reduce Life-Threatening Behaviours Reduce Therapy-Interfering Behaviours Reduce Quality-of-Life-Interfering Behaviours Increase Skills that Replace Ineffective Coping – Goal: Move from behavioural dyscontrol to control to achieve a normal life expectancy

Target Hierarchy in Stage I 1. Life-Threatening Behaviours – Suicide – NSSI 2. Therapy-Interfering Behaviours – E.g. Missing sessions, not completing homework, behaviours that interfere with therapist’s motivation to treat client 3. Quality-of-Life-Interfering Behaviours – E.g. Substance use, eating disordered behaviours, inability to keep employment, educational Issues 4. Skills Acquisition – To replace dysfunctional behaviours
Stages of Treatment Stage II: Suffering in Silence – Focus: – Address inhibited emotional experiencing – Reduce PTSD symptoms – Goal: Move from quiet desperation to full emotional experiencing
Stages of Treatment Stage III: Build a Life Worth Living – Focus: Problems in Living – Goal: Life of ordinary Happiness and Unhappiness Stage IV: Address Issues of Meaning (Optional) – Focus: Spiritual Fulfilment Connectedness to Greater Whole – Goal: Move from incompleteness to ongoing capacity for Experiences of Joy and Freedom
Practice 3 Identify stages of treatment and applicability of the treatment hierarchy to a practice case 1. Choose one of the provided case vignettes. List any therapy goals you and the client might choose to work on 2. Identify at what stage of treatment you would work on each of these goals 3. For Stage I Goals, create a treatment hierarchy: Life-Threatening Behaviours Therapy-Interfering Behaviours Quality-of-Life Interfering Behaviours Skills Acquisition

Treatment
Core DBT Strategies Validation and problem-solving form the core of DBT – All other strategies built around them Problem-solving strategies are change-based – Analyzing behaviour, committing to change, taking steps to change Validation strategies are acceptance-based – Engaging client in understanding actions, emotions, and thoughts
Core DBT Strategies: Validation VALIDATION MEANS: – Communicating to the client that their responses make sense and are understandable within current life context – Finding the kernel of truth in the client’s perspective or situation – Acknowledging causes of emotions, thoughts, and behaviours
Core DBT Strategies: Validation IMPORTANT THINGS TO VALIDATE: – – – – Emotions: Feelings, wanting, suffering, difficulties Thoughts: Beliefs, opinions, or thoughts Actions Abilities REMEMBER: – – – – Every invalid response makes sense in some way Validation is not necessarily agreeing Validation doesn’t mean you like it Only validate the valid
A “How To” Guide to Validation PAY ATTENTION: Listen actively with body and mind. REFLECT BACK: Say back what you heard descriptively and non-judgmentally. READ MINDS: Be sensitive to what is not being said by the client. Be open to correction. UNDERSTAND: Look for how the client’s emotions, thoughts, and actions make sense given their history, state of mind, or current situation, even if you don’t approve of the behaviour, emotion, or action itself.
A “How To” Guide to Validation ACKNOWLEDGE THE VALID: Show you are taking the client seriously by what you say and do SHOW EQUALITY: Be yourself! Treat the client as an equal, not as fragile or incompetent
Practice 4 Practice validation 1. Get into pairs 2. One person will be the “storyteller,” one person will be the “validator” 3. The storyteller tells a story of something that recently happened to them and that elicited some emotion 4. The validator listens and responds only with validation 5. Switch roles
Core DBT Strategies: Chain Analysis Core problem-solving strategy Purpose: examine events and situational factors leading up to and following a problematic response
Steps of a Chain Analysis 1. Choose a specific instance of behavior to analyze 2. Describe the behavior specifically – Topography (“What exactly did you do?”; “What exactly do you mean by that?”) – Frequency (“How many times did you do that?”) – Intensity (“How intense was the feeling on a 1-100 scale?”)
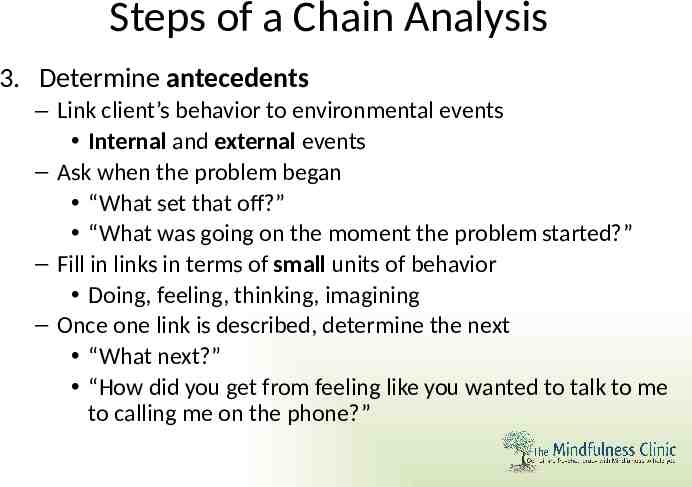
Steps of a Chain Analysis 3. Determine antecedents – Link client’s behavior to environmental events Internal and external events – Ask when the problem began “What set that off?” “What was going on the moment the problem started?” – Fill in links in terms of small units of behavior Doing, feeling, thinking, imagining – Once one link is described, determine the next “What next?” “How did you get from feeling like you wanted to talk to me to calling me on the phone?”
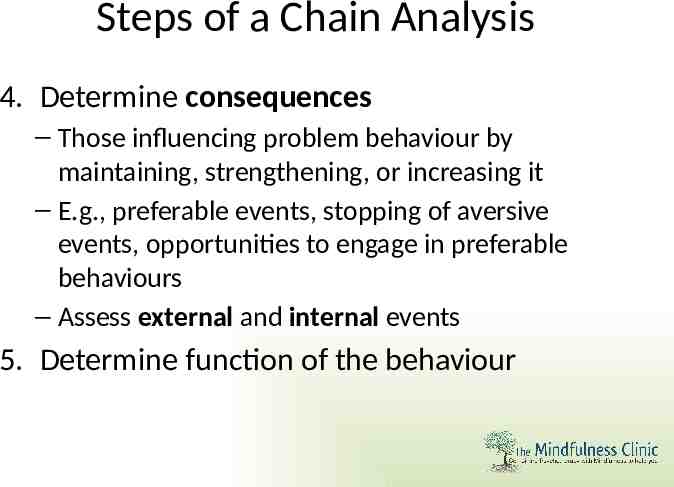
Steps of a Chain Analysis 4. Determine consequences – Those influencing problem behaviour by maintaining, strengthening, or increasing it – E.g., preferable events, stopping of aversive events, opportunities to engage in preferable behaviours – Assess external and internal events 5. Determine function of the behaviour
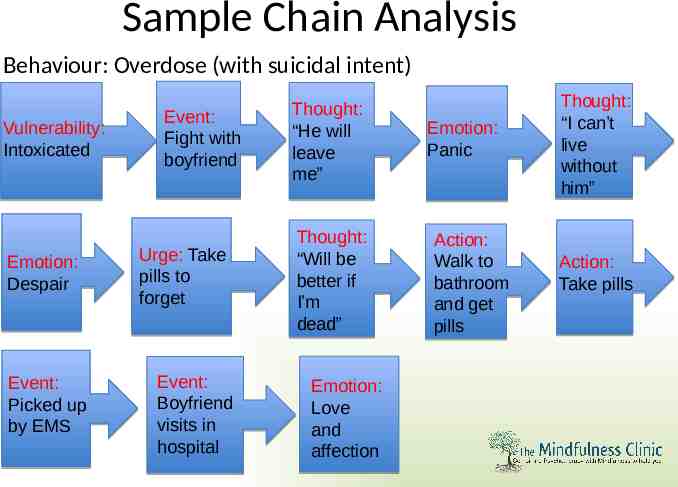
Sample Chain Analysis Behaviour: Overdose (with suicidal intent) Vulnerability: Intoxicated Emotion: Despair Event: Picked up by EMS Event: Fight with boyfriend Urge: Take pills to forget Event: Boyfriend visits in hospital Thought: “He will leave me” Thought: “Will be better if I’m dead” Emotion: Love and affection Emotion: Panic Action: Walk to bathroom and get pills Thought: “I can’t live without him” Action: Take pills
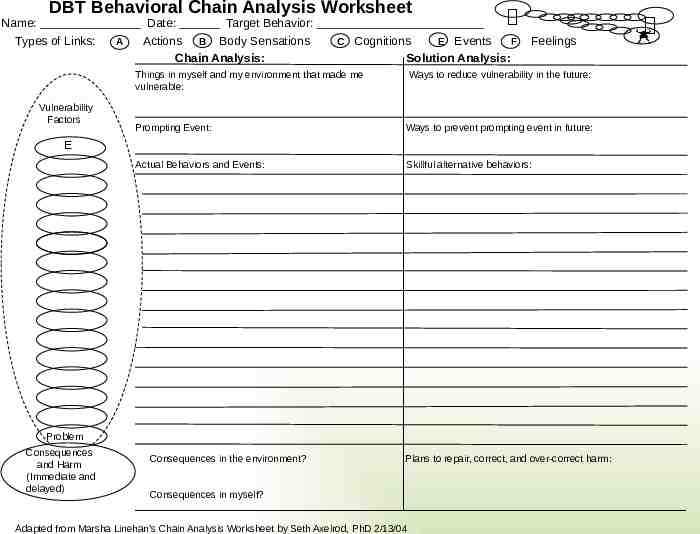
DBT Behavioral Chain Analysis Worksheet Name: Date: Target Behavior: Types of Links: A Actions B Body Sensations Chain Analysis: C Cognitions E Events F Solution Analysis: Things in myself and my environment that made me vulnerable: Vulnerability Factors Feelings Ways to reduce vulnerability in the future: Prompting Event: Ways to prevent prompting event in future: Actual Behaviors and Events: Skillful alternative behaviors: E Problem Behavior Consequences and Harm (Immediate and delayed) Consequences in the environment? Plans to repair, correct, and over-correct harm: Consequences in myself? Adapted from Marsha Linehan’s Chain Analysis Worksheet by Seth Axelrod, PhD 2/13/04

Practice 5 Practice chain analysis using a practice case 1. Get into pairs 2. Choose one of the two vignettes provided 3. One person will role play the client, one person will role play the counsellor 4. Choose a specific behaviour from the case vignette to chain analyze e.g., cutting, waiting for faculty member in the parking lot 5. Role play a chain analysis of this behaviour. The counsellor will have to ask as many questions as needed to “fill in the links of the chain”
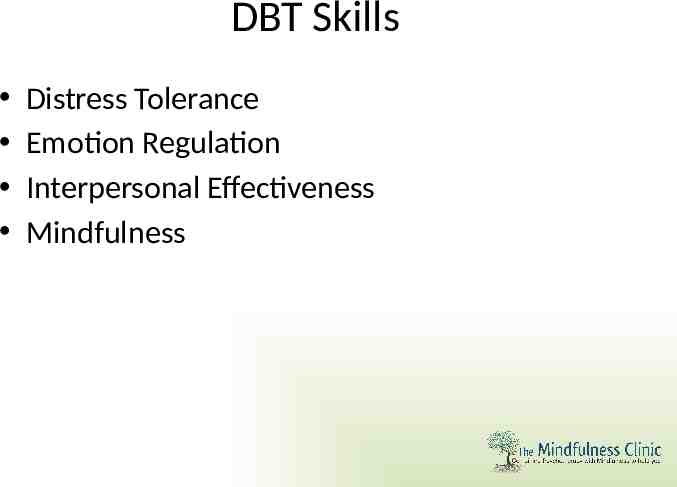
DBT Skills Distress Tolerance Emotion Regulation Interpersonal Effectiveness Mindfulness
Distress Tolerance “How to get through a crisis without making things worse”
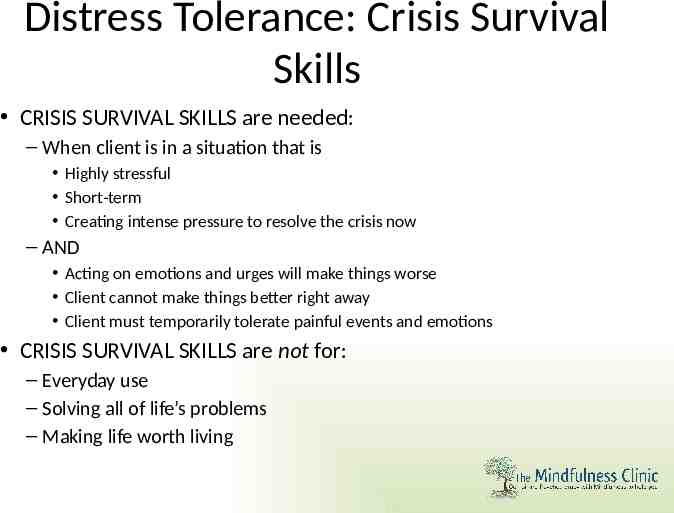
Distress Tolerance: Crisis Survival Skills CRISIS SURVIVAL SKILLS are needed: – When client is in a situation that is Highly stressful Short-term Creating intense pressure to resolve the crisis now – AND Acting on emotions and urges will make things worse Client cannot make things better right away Client must temporarily tolerate painful events and emotions CRISIS SURVIVAL SKILLS are not for: – Everyday use – Solving all of life’s problems – Making life worth living
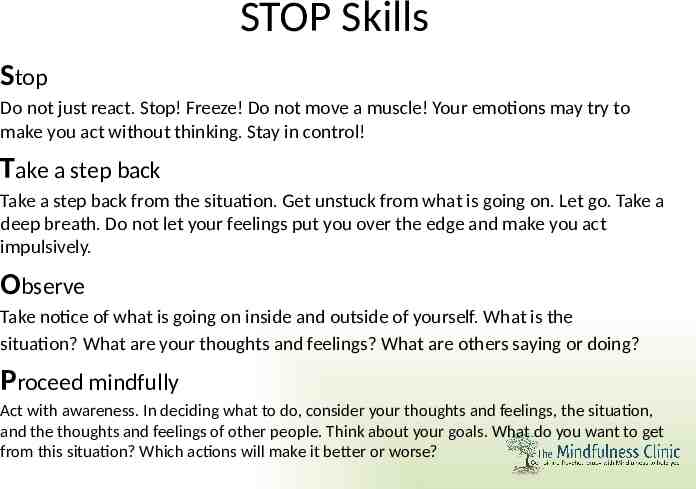
STOP Skills Stop Do not just react. Stop! Freeze! Do not move a muscle! Your emotions may try to make you act without thinking. Stay in control! Take a step back Take a step back from the situation. Get unstuck from what is going on. Let go. Take a deep breath. Do not let your feelings put you over the edge and make you act impulsively. Observe Take notice of what is going on inside and outside of yourself. What is the situation? What are your thoughts and feelings? What are others saying or doing? Proceed mindfully Act with awareness. In deciding what to do, consider your thoughts and feelings, the situation, and the thoughts and feelings of other people. Think about your goals. What do you want to get from this situation? Which actions will make it better or worse?
TIPP Skills TIP YOUR TEMPERATURE INTENSELY EXERCISE PACE YOUR BREATHING PROGRESSIVELY RELAX YOUR MUSCLES
TIPP Skills Tip the TEMPERATURE of your face: use ice water to calm yourself down fast by changing the response of your autonomic nervous system – Put your face in a bowl of ICE WATER (30 seconds) – OR splash ICE WATER on your face, – OR hold a gel ICE pack (or zip-lock ICE WATER) on your face. INTENSELY EXERCISE to calm down a body revved up by emotion – Engage in intense exercise, if only for a short while. – Expend your body’s stored up physical energy by: Running, Walking , Fast Jumping, Playing Basketball, Weight Lifting, etc.
TIPP Skills PACE YOUR BREATHING BY SLOWING IT DOWN – Slow your pace of inhaling and exhaling way down (on average 5 to 7 breath cycles per minute). – Breathe deeply from the abdomen. – Breathe more slowly out than when breathing in (for example, 4 seconds in and 8 seconds out). PROGRESSIVELY RELAX YOUR MUSCLES – Starting with your hands, moving to your forearms, upper arms, shoulders, neck, forehead, eyes, cheeks & lips, tongue & jaw, chest, upper back, stomach, buttocks, thighs, calves, ankles, feet. – TENSE (5 seconds), then let go and RELAX each muscle (all the way). – NOTICE the tension. NOTICE the difference when relaxed.
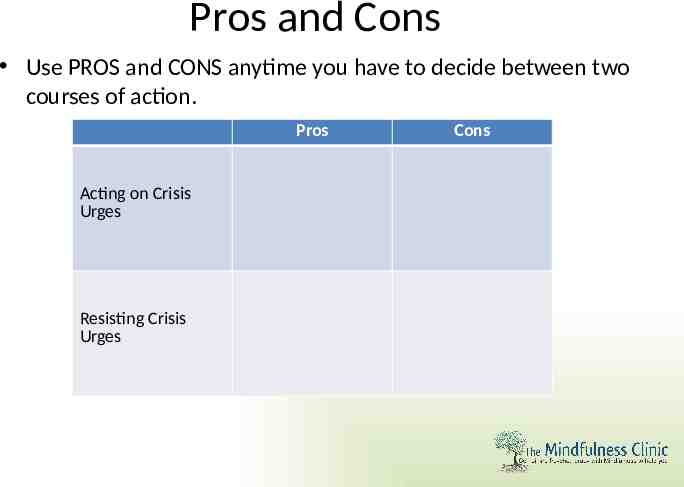
Pros and Cons Use PROS and CONS anytime you have to decide between two courses of action. Pros Acting on Crisis Urges Resisting Crisis Urges Cons
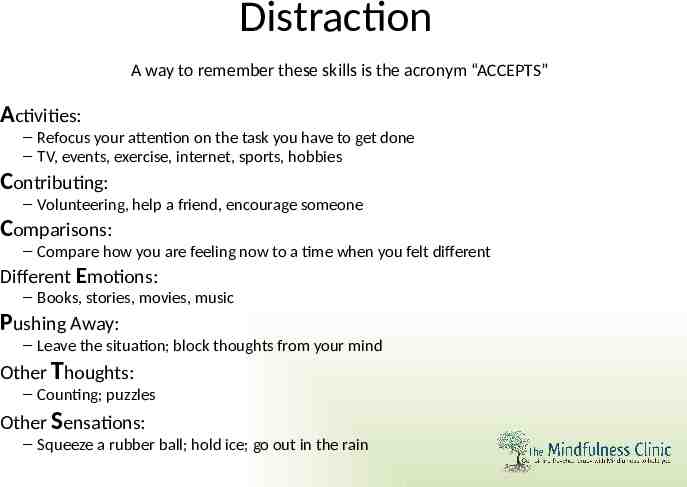
Distraction A way to remember these skills is the acronym “ACCEPTS” Activities: – Refocus your attention on the task you have to get done – TV, events, exercise, internet, sports, hobbies Contributing: – Volunteering, help a friend, encourage someone Comparisons: – Compare how you are feeling now to a time when you felt different Different Emotions: – Books, stories, movies, music Pushing Away: – Leave the situation; block thoughts from your mind Other Thoughts: – Counting; puzzles Other Sensations: – Squeeze a rubber ball; hold ice; go out in the rain
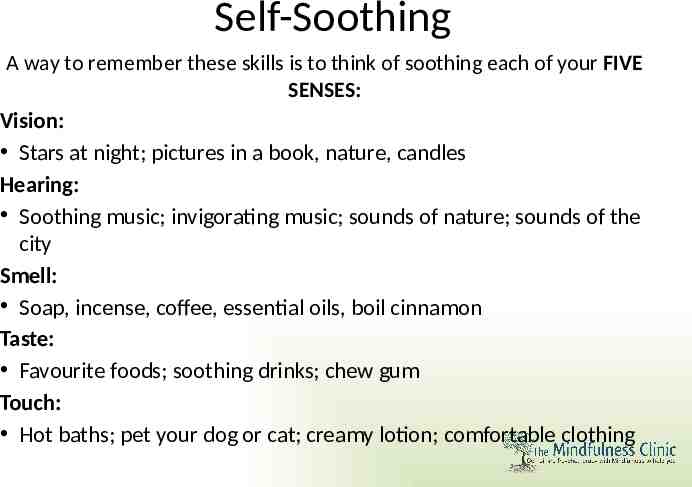
Self-Soothing A way to remember these skills is to think of soothing each of your FIVE SENSES: Vision: Stars at night; pictures in a book, nature, candles Hearing: Soothing music; invigorating music; sounds of nature; sounds of the city Smell: Soap, incense, coffee, essential oils, boil cinnamon Taste: Favourite foods; soothing drinks; chew gum Touch: Hot baths; pet your dog or cat; creamy lotion; comfortable clothing
Group Discussion 1 Discuss how Distress Tolerance skills may be helpful to our practice cases At your table, choose one case vignette. 1. How could these distress tolerance skills help the client in the vignettes accomplish their treatment goals? 2. How would you teach these skills to a client?
Emotion Regulation “How to understand emotions, change ineffective emotions, and be less vulnerable to negative emotions”
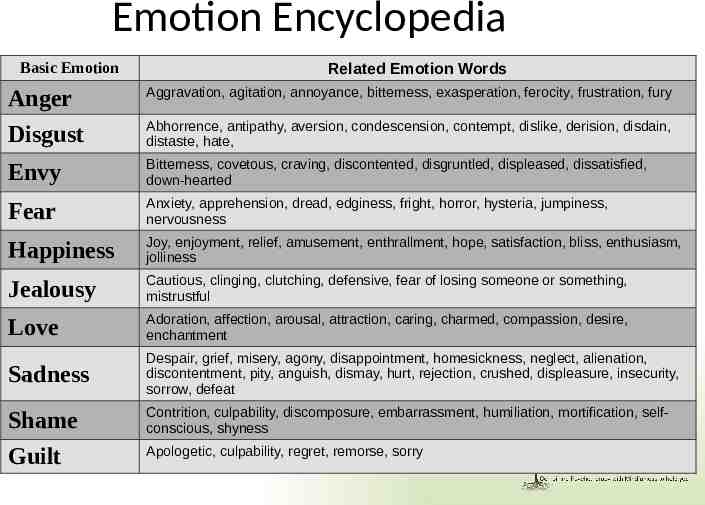
Emotion Encyclopedia Basic Emotion Related Emotion Words Anger Aggravation, agitation, annoyance, bitterness, exasperation, ferocity, frustration, fury Disgust Abhorrence, antipathy, aversion, condescension, contempt, dislike, derision, disdain, distaste, hate, Envy Bitterness, covetous, craving, discontented, disgruntled, displeased, dissatisfied, down-hearted Fear Anxiety, apprehension, dread, edginess, fright, horror, hysteria, jumpiness, nervousness Happiness Joy, enjoyment, relief, amusement, enthrallment, hope, satisfaction, bliss, enthusiasm, jolliness Jealousy Cautious, clinging, clutching, defensive, fear of losing someone or something, mistrustful Love Adoration, affection, arousal, attraction, caring, charmed, compassion, desire, enchantment Sadness Despair, grief, misery, agony, disappointment, homesickness, neglect, alienation, discontentment, pity, anguish, dismay, hurt, rejection, crushed, displeasure, insecurity, sorrow, defeat Shame Contrition, culpability, discomposure, embarrassment, humiliation, mortification, selfconscious, shyness Guilt Apologetic, culpability, regret, remorse, sorry
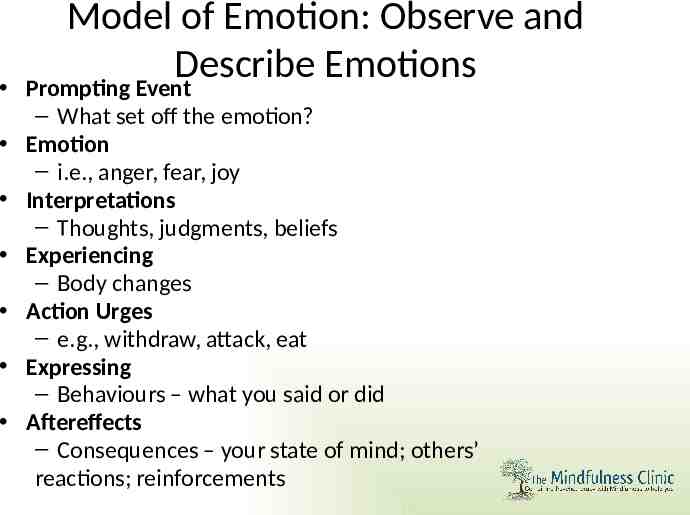
Model of Emotion: Observe and Describe Emotions Prompting Event – What set off the emotion? Emotion – i.e., anger, fear, joy Interpretations – Thoughts, judgments, beliefs Experiencing – Body changes Action Urges – e.g., withdraw, attack, eat Expressing – Behaviours – what you said or did Aftereffects – Consequences – your state of mind; others’ reactions; reinforcements
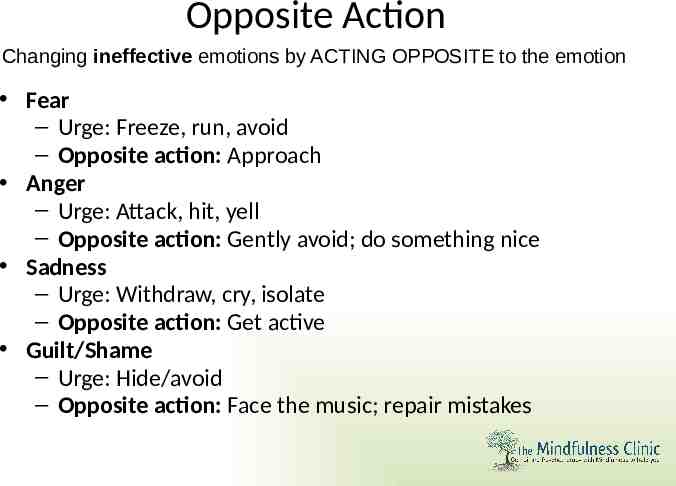
Opposite Action Changing ineffective emotions by ACTING OPPOSITE to the emotion Fear – Urge: Freeze, run, avoid – Opposite action: Approach Anger – Urge: Attack, hit, yell – Opposite action: Gently avoid; do something nice Sadness – Urge: Withdraw, cry, isolate – Opposite action: Get active Guilt/Shame – Urge: Hide/avoid – Opposite action: Face the music; repair mistakes
Group Discussion 2 Discuss how Emotion Regulation skills may be helpful to our practice cases At your table, choose one case vignette. 1. How could these emotion regulation skills help the client in the vignettes accomplish their treatment goals? 2. How would you teach these skills to a client?
Interpersonal Effectiveness “How to get your needs met while maintaining your relationships and selfrespect”
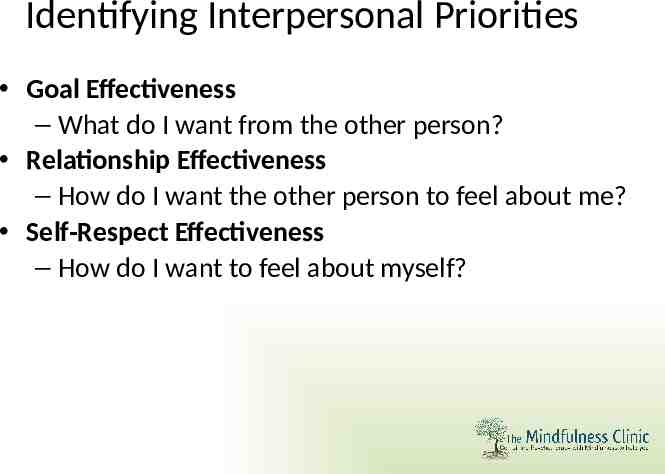
Identifying Interpersonal Priorities Goal Effectiveness – What do I want from the other person? Relationship Effectiveness – How do I want the other person to feel about me? Self-Respect Effectiveness – How do I want to feel about myself?
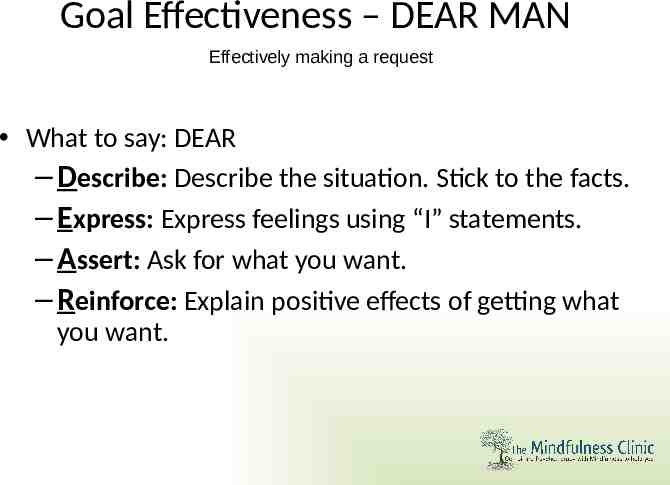
Goal Effectiveness – DEAR MAN Effectively making a request What to say: DEAR – Describe: Describe the situation. Stick to the facts. – Express: Express feelings using “I” statements. – Assert: Ask for what you want. – Reinforce: Explain positive effects of getting what you want.
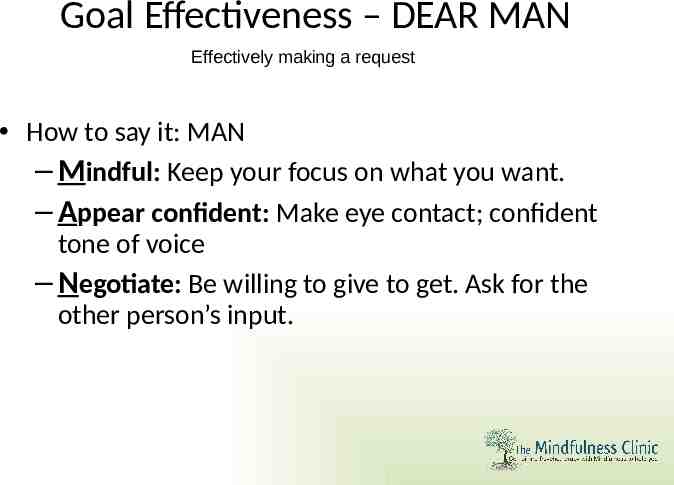
Goal Effectiveness – DEAR MAN Effectively making a request How to say it: MAN – Mindful: Keep your focus on what you want. – Appear confident: Make eye contact; confident tone of voice – Negotiate: Be willing to give to get. Ask for the other person’s input.
Practice 6 Practice using DEAR MAN to make a request 1. Get into pairs 2. One person will make a request using DEAR MAN for something a person might ask of another person 3. Switch roles
Mindfulness “How to pay attention to the present moment without judgment, rejection, or attachment”
Mindfulness “WHAT” SKILLS Observe Describe Participate “HOW” SKILLS Non-judgmental Effective One-mindful
Non-judgmental Notice, but don’t evaluate as “good” or “bad” Acknowledge harmful and helpful, but don’t judge – E.g., replace “You’re a jerk” with “I feel mad when you do that” Catch judgments so that you have more control over your emotions Steps 1. Notice judgments 2. Don’t judge your judgments 3. Replace judgments with descriptions (things you can see, hear, feel, taste, touch)
Practice 9 Practice non-judgmental 1. Get into pairs 2. Think of a difficult client you have worked with or choose a client from the case vignettes 3. Describe your client to the other person without judgment 4. For the listener: pay attention and note any judgments that occur 5. Switch roles
Additional Issues in DBT Interacting with Other Professionals Further Training Recommended Readings
DBT and Other Professionals Ancillary mental health treatments are acceptable in DBT – However, there can be only one primary individual therapist at a time “Consultation to the patient” approach: – Teach the client to act as their own agent in obtaining appropriate care – Do not intervene, solve problems, or act for the patient with other professionals Rationale: – Teaching effective self-care – Decreasing “splitting” – Promoting respect for the client
When Another Professional Calls: Obtain as much information about the situation as they will give Provide caller with necessary information the client cannot give, and verify information client has given Tell them to follow their normal procedures Ask to talk to the client Coach client on how to best cope with situation and interact with the professionals
Further Training and Certification Training Opportunities – Behavioral Tech Founded by Marsha Linehan Gold Standard for Training Online workshops/training, Web Shorts, Multi-day Workshops, Consultation, Intensive Trainings for Individuals and Teams http://behavioraltech.org/training/ – Oshawa Psychotherapy Training Institute Facilitated by Clinicians from CAMH Four-part Training – 2 days each, often offered to suit 9-5 work schedules (evening and weekend) Parts can be taken individually http:// www.oshawapsychotherapytraining.com/courses/certificate-programs/d bt-1
Further Training and Certification Training Opportunities – CAMH Dialectical Behaviour Therapy Certificate Program Four-part training – A-D, 8 evenings each http://www.camh.ca/en/education/about/AZCourses – The Mindfulness Clinic Supervision, Consultation, Individualized Workshops DBT Training Courses may be offered in the future Parts can be taken individually http://www.themindfulnessclinic.ca/therapy-training/dialecti cal-behaviour-therapy-dbt /
Further Training and Certification DBT Certification – Offered through Linehan Institute – Requires: Graduate Degree from Accredited Institution Licensed as independent mental health provider 40-hours of Didactic DBT Training Completion of Treatment with at Least Three DBT cases using full-mode DBT 12-months and current participation on DBT consultation team Read skills manual, complete all homework in skills manual, facilitate teaching of all skills in manual in individual or group format Exam Letter of Recommendation Work Product Demonstration Demonstrated Mindfulness Experience – Other Certification Programs Exist but do not offer the same standards/credibility
Options for Treatment Referrals in Ontario Publically Funded Toronto, ON – Centre for Addiction and Mental Health – Davenport Perth Neighbourhood Centre – Surfing Tsunamis Program London, ON – London Health Sciences Centre – Victoria Hospital Hamilton, ON – St. Joseph’s Health Care DBT Program

Options for Treatment Referrals in Ontario Private Treatment Options – The Mindfulness Clinic: Toronto, ON Comprehensive Adult and Adolescent DBT Program – Individual Therapy – Adult Skills Training Groups – Adolescent Multi-Family Skills Training Groups – Phone Coaching – Weekly Therapist Consultation Team – More info: http ://www.themindfulnessclinic.ca/therapy-training/dialec tical-behaviour-therapy-dbt /
Options for Treatment Referrals in Ontario Private Treatment Options Broadview Psychology: Toronto, ON http://www.broadviewpsychology.com/ Behavioural Health: Guelph, ON Comprehensive DBT Program http://www.behaviouralhealth.net Dr. Carmen Weiss & Associates: Burlington, ON Group and Individual DBT-based Treatment http://drcarmenweiss.ca/group-options/dialectical-behavio ur-therapy-dbt-options/
Further Reading
Further Reading

References Dimeff, L. A., & Koerner, K. (Eds.) (2007). Dialectical Behavior Therapy in clinical practice: Applications across disorders and settings. New York: Guilford Press. Linehan, M. M. (1993). Cognitive Behavioral Treatment of Borderline Personality Disorder. New York: Guilford Press. Linehan, M. M., Armstrong, H. E., Suarez, A., Allmon, D., & Heard, H. L. (1991). Cognitive-behavioral treatment of chronically parasuicidal borderline patients. Archives of General Psychiatry, 48, 1060-1064. Koerner, K. (2011). Doing Dialectical Behavior Therapy: A practical guide. New York: Guilford Press. Koons, C. R., Robins, C. J., Tweed, J. L., Lynch, T. R., Gonzalez, A. M., Morse, J. Q., Bishop, G. K., Butterfield, M. I., & Bastian, L. A. (2001). Efficacy of Dialectical Behavior Therapy in Women Veterans with Borderline Personality Disorder. Behavior Therapy, 32, 371-390. Linehan, M. M., Schmidt, H., Dimeff, L. A., Kanter, J. W., Craft, J. C., Comtois, K. A., & Recknor, K. L. (1999). Dialectical Behavior Therapy for Patients with Borderline Personality Disorder and Drug-Dependence. American Journal on Addiction, 8, 279-292. Miller, A. L., Rathus, J. H., & Linehan, M. M. (2006). Dialectical Behavior Therapy with suicidal adolescents. New York: Guilford Press. Verheul, R., Van Den Bosch, L. M. C., Koeter, M. W. J., De Ridder, M. A. J. , Stijnen, T., & Van Den Brink, W. (2003). Dialectical Behaviour Therapy for Women with Borderline Personality Disorder, 12-month, Randomised Clinical Trial in The Netherlands. British Journal of Psychiatry, 182, 135-140.